Suprapubic Prostatectomy
Medically reviewed by Drugs.com. Last updated on Jun 30, 2025.
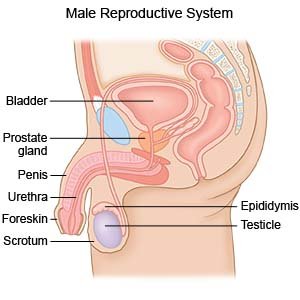
Suprapubic prostatectomy is surgery to remove part or all of your prostate gland. Your prostate gland is found below your bladder and surrounds the top of your urethra. Your urethra is a tube that carries urine from your bladder to the outside of your body. You may need suprapubic prostatectomy if you have an enlarged prostate.
 |
WHILE YOU ARE HERE:
Before your surgery:
- Informed consent is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
- An IV will be placed into a vein. You may be given liquid or medicine through the IV.
- Anesthesia is medicine to make you comfortable during the surgery. Healthcare providers will work with you to decide which anesthesia is best for you.
- General anesthesia will keep you asleep and free from pain during surgery. Anesthesia may be given through your IV. You may instead breathe it in through a mask or a tube placed down your throat. The tube may cause you to have a sore throat when you wake up.
- Spinal or epidural anesthesia numbs the area and dulls the pain. You may still feel pressure or pushing during surgery.
During your surgery:
Your surgeon will make an incision in your abdomen below your belly button. He or she will remove part or all of your prostate. A suprapubic catheter may be placed into your bladder through the cut in your abdomen to drain your urine. A drain may be placed near your bladder to remove extra blood and fluid. Your surgeon will use stitches or staples to close your incision.
Related medications
Sandostatin
Sandostatin is used to treat acromegaly and to reduce flushing episodes and watery diarrhea caused ...
Sandostatin LAR Depot
Sandostatin LAR Depot is used for acromegaly, carcinoid tumor, vasoactive intestinal peptide tumor
Dupixent
Dupixent is used to treat eczema, eosinophilic or oral-corticosteroid-dependent asthma, chronic ...
Lupron Depot
Lupron Depot is used to treat advanced prostate cancer, endometriosis, uterine fibroids, and ...
Casodex
Casodex (bicalutamide) is an anti-androgen and is used together with LHRH to treat prostate cancer ...
Xtandi
Xtandi (enzalutamide) is an anti-androgen used to treat prostate prostate cancer. Includes Xtandi ...
Zytiga
Zytiga (abiraterone) is used together with prednisone to treat prostate cancer that has spread to ...
Eligard
Eligard (leuprolide) reduces levels of testosterone and is used to treat prostate cancer. Includes ...
Pluvicto
Pluvicto (lutetium lu 177 vipivotide tetraxetan) is used for PSMA-positive metastatic ...
Lutetium lu 177 vipivotide tetraxetan
Lutetium lu 177 vipivotide tetraxetan is used for prostate cancer
After your surgery:
You will be taken to a room to rest until you are fully awake. You will be monitored closely for any problems. Do not get out of bed until your healthcare provider says it is okay. You will then be able to go home or be taken to your hospital room.
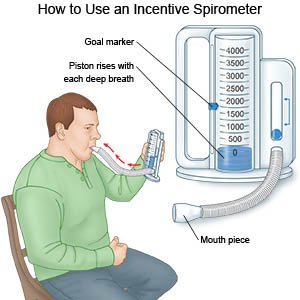
- Take deep breaths and cough 10 times each hour. This will decrease your risk for a lung infection. Take a deep breath and hold it for as long as you can. Let the air out and then cough strongly. Deep breaths help open your airway. You may be given an incentive spirometer to help you take deep breaths. Put the plastic piece in your mouth and take a slow, deep breath, then let the air out and cough. Repeat these steps 10 times every hour.
- You may need to walk around the same day of surgery, or the day after. Movement will help prevent blood clots. You may also be given exercises to do in bed. Do not get out of bed on your own until your healthcare provider says you can. Talk to healthcare providers before you get up the first time. They may need to help you stand up safely. When you are able to get up on your own, sit or lie down right away if you feel weak or dizzy. Then press the call light button to let healthcare providers know you need help.
- A Foley catheter will put into your bladder. A Foley catheter is a tube used to drain urine into a bag. Healthcare providers will remove the catheter as soon as possible to help prevent infection.
- A constant flow of fluid may be put through your bladder catheter. The fluid will flush out blood and prevent blood clots. The fluid will go in one bladder catheter and out another or in and out of the same bladder catheter.
- You will be able to eat and drink slowly after surgery. You will begin with ice chips or clear liquids such as water, broth, juice, and clear soft drinks. If your stomach does not become upset, you may then eat soft foods, such as ice cream and applesauce. Once you can eat soft foods easily, you may slowly begin to eat solid foods.
- Medicines may be given to relieve pain or to prevent an infection.
RISKS:
You may bleed more than expected or get an infection. Your bladder, urethra, penis, or nearby tissues may be damaged. Your urethra may become narrow and block the flow of urine. The muscle at the base of your bladder may shorten and cause you to leak urine. Urine may leak inside your body and collect in nearby areas, such as your scrotum. Your kidneys may stop working properly. You may get a blood clot in your leg. This may become life-threatening.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
