Viramune Side Effects
Generic name: nevirapine
Medically reviewed by Drugs.com. Last updated on Feb 26, 2024.
Note: This document contains side effect information about nevirapine. Some dosage forms listed on this page may not apply to the brand name Viramune.
Applies to nevirapine: oral suspension, oral tablet, oral tablet extended release.
Warning
Oral route (Tablet; Tablet, Extended Release; Suspension)
Severe, life-threatening, in some cases fatal, hepatotoxicity and skin reactions (eg, Stevens-Johnson syndrome, toxic epidermal necrolysis, and hypersensitivity reactions characterized by rash, constitutional findings, and organ dysfunction) have been reported. Women, including pregnant women, or patients with higher CD4+ cell counts are at higher risk of hepatotoxicity. Permanently discontinue nevirapine following severe hepatic, skin, or hypersensitivity reactions. Check transaminase levels immediately for all patients who develop a rash during the first 18 weeks of treatment. Monitor patients intensively during the first 18 weeks of therapy with nevirapine to detect potentially life-threatening hepatotoxicity or skin reactions. Extra vigilance is warranted during the first 6 weeks of therapy, which is the period of greatest risk for adverse events. Strictly follow the 14-day lead-in period with immediate-release nevirapine 200 mg daily dosing.
Serious side effects of Viramune
Along with its needed effects, nevirapine (the active ingredient contained in Viramune) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking nevirapine:
Less common
- Decreased appetite
- swelling of the feet or lower legs
Rare
- Pain, numbness, or tingling of the hands, arms, legs, or feet
- sleepiness or unusual drowsiness
- stomach pain
- tingling, burning, or prickly sensations
Incidence not known
- Black, tarry stools
- blistering, peeling, or loosening of the skin
- bone pain
- chest pain
- chills
- clay-colored stools
- cough
- dark urine
- diarrhea
- difficulty swallowing
- dizziness
- fast heartbeat
- fever
- general tiredness and weakness
- headache
- hives, itching, skin rash
- joint or muscle pain
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or genitals
- loss of appetite
- lower back or side pain
- muscle cramps, spasms, pain, or stiffness
- nausea
- painful or difficult urination
- pale skin
- puffiness or swelling of the eyelids or around the eyes, face, lips, or tongue
- red skin lesions, often with a purple center
- red, irritated eyes
- seizures
- sore throat
- sores, ulcers, or white spots in the mouth or on the lips
- stomach pain, continuing
- swollen glands
- tightness in the chest
- trouble breathing
- troubled breathing with exertion
- unpleasant breath odor
- unusual bleeding or bruising
- unusual tiredness or weakness
- vomiting
- vomiting of blood
- yellow eyes and skin
Get emergency help immediately if any of the following symptoms of overdose occur while taking nevirapine:
Symptoms of overdose
- Chest pain
- cough
- decrease in weight
- dizziness or lightheadedness
- feeling of constant movement of self or surroundings
- headache
- pain in the ankles or knees
- painful, red lumps under the skin, mostly on the legs
- sensation of spinning
- trouble sleeping
Other side effects of Viramune
Some side effects of nevirapine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common
- Difficulty with moving
- pain in the joints
For Healthcare Professionals
Applies to nevirapine: oral suspension, oral tablet, oral tablet extended release.
General
Serious side effects have occurred with this drug. The most serious side effects have included hepatitis, hepatic failure, Stevens-Johnson syndrome, toxic epidermal necrolysis, drug reaction with eosinophilia and systemic symptoms, and hypersensitivity reactions. Hepatitis/hepatic failure have been isolated or associated with signs of hypersensitivity which have included severe rash or rash accompanied by fever, general malaise, fatigue, muscle/joint aches, blisters, oral lesions, conjunctivitis, facial edema, eosinophilia, granulocytopenia, lymphadenopathy, or renal dysfunction.
The most commonly reported side effects were rash, allergic reactions, nausea, abnormal liver function tests, headache, fatigue, somnolence, hepatitis, abdominal pain, vomiting, diarrhea, pyrexia, and myalgia.[Ref]
Dermatologic
The most common clinical toxicity was rash. Rashes were usually mild to moderate, maculopapular erythematous cutaneous eruptions, with or without pruritus, located on the face, trunk, and extremities. Rash has occurred most often during the first 6 weeks of therapy. Utilization of the 14-day lead-in period with an immediate-release formulation has been shown to reduce the frequency of rash.
During clinical trials, grade 1 and 2 rashes were reported in 13% of patients using an immediate-release formulation during the first 6 weeks of therapy; grade 3 and 4 rashes were reported in 2% of patients using an immediate-release formulation.
During 1 study, side effects of at least moderate intensity included rash (including rash, maculopapular rash, erythema nodosum, erythematous rash, papular rash, skin reaction, Stevens-Johnson syndrome, DRESS) in 4% and 5% of patients using the immediate-release and extended-release formulations, respectively. DRESS was characterized by rash with constitutional symptoms (e.g., fever, arthralgia, myalgia, lymphadenopathy) plus visceral involvement (e.g., hepatitis, eosinophilia, granulocytopenia, renal dysfunction).
Severe and life-threatening skin reactions (including fatal cases) have been reported. These have included cases of Stevens-Johnson syndrome, toxic epidermal necrolysis, and hypersensitivity reactions characterized by rash, constitutional findings, and organ dysfunction.
Rash was reported in about half of patients with symptomatic hepatic side effects.[Ref]
Very common (10% or more): Rash (including maculopapular erythematous cutaneous eruptions, with or without pruritus)
Common (1% to 10%): Moderate/severe rash (including rash, maculopapular rash, erythema nodosum, erythematous rash, papular rash, skin reaction, Stevens-Johnson syndrome, drug reaction with eosinophilia and systemic symptoms [DRESS])
Uncommon (0.1% to 1%): Toxic epidermal necrolysis, urticaria, angioedema
Frequency not reported: Severe and life-threatening skin reactions (including fatal cases), allergic dermatitis[Ref]
Other
Very common (10% or more): Decreased phosphate (up to 38%), elevated cholesterol (up to 19%), elevated low-density lipoprotein (LDL) (up to 15%)
Common (1% to 10%): Fatigue, pyrexia
Frequency not reported: Asthenia, influenza-like symptoms, elevated alkaline phosphatase, elevated total cholesterol, elevated triglycerides
Postmarketing reports: Fever, drug withdrawal (as a result of drug interactions), decreased serum phosphorus[Ref]
Grade 2 decreased phosphate was reported in 38% and 33% of patients using the immediate-release and extended-release formulations, respectively. Grade 3 decreased phosphate was reported in 6% and 7% of patients using the immediate-release and extended-release formulations, respectively. Grade 4 decreased phosphate was reported in less than 1% of patients using the immediate-release formulation.
Grade 2 elevated cholesterol (240 to 300 mg/dL) was reported in 18% and 19% of patients using the immediate-release and extended-release formulations, respectively. Grade 3 elevated cholesterol (greater than 300 mg/dL) was reported in 4% and 3% of patients using the immediate-release and extended-release formulations, respectively.
The incidence of grade 2 elevated LDL (160 to 190 mg/dL) was 15% with each formulation. The incidence of grade 3 elevated LDL (greater than 190 mg/dL) was 5% with each formulation.
During 1 study, side effects of at least moderate intensity included fatigue (immediate-release: 2%; extended-release: 2%) and pyrexia (immediate-release: 2%; extended-release: 1%).
Fever and influenza-like symptoms accompanied some hepatic events.[Ref]
Hepatic
Very common (10% or more): Elevated ALT (up to 14%), symptomatic hepatic events (up to 11%)
Common (1% to 10%): Elevated AST, asymptomatic transaminase elevations (AST/ALT), clinical hepatitis (including hepatitis, hepatotoxicity, acute hepatitis, liver disorder, toxic hepatitis, hepatic failure, jaundice), elevated bilirubin, asymptomatic elevations in GGT, abnormal liver function tests (included increased ALT, increased transaminases, increased AST, increased GGT, increased hepatic enzyme, hypertransaminasemia)
Frequency not reported: Liver enzyme abnormalities (AST, ALT, GGT), severe and life-threatening hepatotoxicity (including fatal cases), progression to hepatic failure (with transaminase elevation, with or without hyperbilirubinemia, hepatic encephalopathy, prolonged partial thromboplastin time, or eosinophilia), hepatic-renal failure syndromes
Postmarketing reports: Jaundice, fulminant and cholestatic hepatitis, hepatic necrosis, hepatic failure[Ref]
Elevated ALT (greater than 250 units/L: up to 14%) has been reported with the immediate-release formulation. Grade 2 elevated ALT (2.6 to 5 times the upper limit of normal [2.6 to 5 x ULN]) was reported in 13% and 10% of patients using the immediate-release and extended-release formulations, respectively. Grade 3 elevated ALT (5.1 to 10 x ULN) was reported in 3% and 4% of patients using the immediate-release and extended-release formulations, respectively. Grade 4 elevated ALT (greater than 10 x ULN) was reported in 4% and 2% of patients using the immediate-release and extended-release formulations, respectively.
Elevated AST (greater than 250 units/L: up to 8%) has been reported with the immediate-release formulation. Grade 2 elevated AST (2.6 to 5 x ULN) was reported in 9% and 7% of patients using the immediate-release and extended-release formulations, respectively. Grade 3 elevated AST (5.1 to 10 x ULN) was reported in 2% and 3% of patients using the immediate-release and extended-release formulations, respectively. The incidence of grade 4 elevated AST (greater than 10 x ULN) was 2% with each formulation.
In clinical trials, symptomatic hepatic events (regardless of severity) were reported in up to 11% of patients. Rash was reported in about half of patients with symptomatic hepatic side effects. Fever and influenza-like symptoms accompanied some hepatic events.
In 1 study, after the lead-in period, the incidence of any hepatic event was 9% with the immediate-release formulation and 6% with the extended-release formulation. Symptomatic hepatic events (anorexia, jaundice, vomiting) were reported in 3% and 2% of patients using the immediate-release and extended-release formulations, respectively. The incidence of grade 3 or 4 ALT/AST elevation was 8% with each formulation.
During 1 study, side effects of at least moderate intensity included clinical hepatitis (including hepatitis, hepatotoxicity, acute hepatitis, liver disorder, toxic hepatitis, hepatic failure, jaundice) in 4% and 2% of patients using the immediate-release and extended-release formulations, respectively.
Asymptomatic transaminase elevations (AST/ALT greater than 5 x ULN) have been reported in up to 9% of patients. Elevated bilirubin (greater than 2.5 mg/dL) has been reported in 2% of patients.
Liver enzyme abnormalities (AST, ALT, GGT) occurred more often in patients using this drug than in controls.
Severe, life-threatening, and in some cases fatal, hepatotoxicity (including fulminant and cholestatic hepatitis, hepatic necrosis, and hepatic failure) has been reported. In some cases, patients presented with nonspecific prodromal signs/symptoms of hepatitis (including fatigue, malaise, anorexia, nausea, jaundice, liver tenderness/hepatomegaly, with or without initially abnormal transaminase levels). Some events (particularly those with rash and other symptoms) progressed to hepatic failure with transaminase elevation, with or without hyperbilirubinemia, hepatic encephalopathy, prolonged partial thromboplastin time, or eosinophilia. Patients without HIV using this drug for postexposure prophylaxis have reported serious hepatotoxicity, including hepatic failure.[Ref]
Hematologic
Very common (10% or more): Decreased neutrophils (up to 13%)
Common (1% to 10%): Decreased hemoglobin, granulocytopenia
Uncommon (0.1% to 1%): Decreased platelets
Frequency not reported: Thrombocytopenia
Postmarketing reports: Anemia, neutropenia, eosinophilia[Ref]
Decreased neutrophils (less than 750/mm3), hemoglobin (less than 8 g/dL), and platelets (less than 50,000/mm3) have been reported in up to 13%, up to 3%, and up to 1% of patients, respectively.
Grade 2 decreased neutrophils (750 to 999/mm3) was reported in 7% and 4% of patients using the immediate-release and extended-release formulations, respectively. The incidence of grade 3 decreased neutrophils (500 to 749/mm3) was 2% with each formulation. The incidence of grade 4 decreased neutrophils (less than 500/mm3) was 1% with each formulation.[Ref]
Hypersensitivity
Common (1% to 10%): Hypersensitivity (including anaphylactic reaction, angioedema, urticaria)
Uncommon (0.1% to 1%): Anaphylactic reaction
Postmarketing reports: Allergic reactions (including anaphylaxis, angioedema, bullous eruptions, ulcerative stomatitis, urticaria), hypersensitivity syndrome, hypersensitivity reactions (with rash associated with constitutional findings such as fever, blistering, oral lesions, conjunctivitis, facial edema, muscle/joint aches, general malaise, fatigue, or significant hepatic abnormalities, drug reaction with eosinophilia and systemic symptoms, plus hepatitis, eosinophilia, granulocytopenia, lymphadenopathy, and/or renal dysfunction)[Ref]
Gastrointestinal
Common (1% to 10%): Nausea, elevated amylase, diarrhea, abdominal pain
Frequency not reported: Pancreatitis
Postmarketing reports: Vomiting[Ref]
During 1 study, side effects of at least moderate intensity included diarrhea (immediate-release: 4%; extended-release: 4%), abdominal pain (immediate-release: 2%; extended-release: 3%), and nausea (immediate-release: 2%; extended-release: 1%).
Grade 2 elevated amylase (1.6 to 2 x ULN) was reported in 4% and 5% of patients using the immediate-release and extended-release formulations, respectively. Grade 3 elevated amylase (2.1 to 5 x ULN) was reported in 4% and 2% of patients using the immediate-release and extended-release formulations, respectively. Grade 4 elevated amylase (greater than 5 x ULN) was reported in less than 1% of patients using the extended-release formulation.[Ref]
Nervous system
During 1 study, side effects of at least moderate intensity included headache; incidence was 4% with each formulation.[Ref]
Common (1% to 10%): Headache
Frequency not reported: Neuropathy, peripheral neuropathy
Postmarketing reports: Somnolence, paresthesia[Ref]
Musculoskeletal
During 1 study, side effects of at least moderate intensity included arthralgia; incidence was 2% with each formulation.[Ref]
Common (1% to 10%): Arthralgia, myalgia
Frequency not reported: Arthromyalgia, arthritis
Postmarketing reports: Rhabdomyolysis (associated with skin and/or liver reactions), arthralgia
Combination antiretroviral therapy:
-Frequency not reported: Osteonecrosis[Ref]
Cardiovascular
Uncommon (0.1% to 1%): Increased blood pressure
Metabolic
Frequency not reported: Hyperlactatemia, unspecified metabolic alterations, anorexia, acute porphyria
Postmarketing reports: Redistribution/accumulation of body fat (including central obesity, dorsocervical fat enlargement, peripheral wasting, facial wasting, breast enlargement, "cushingoid appearance")[Ref]
Immunologic
Frequency not reported: Immune reconstitution syndrome, autoimmune disorders in the setting of immune reconstitution (e.g., Graves' disease, polymyositis, Guillain-Barre syndrome)
Respiratory
Frequency not reported: Dry cough, dyspnea, interstitial pulmonary infiltration[Ref]
Psychiatric
Frequency not reported: Depression[Ref]
More about Viramune (nevirapine)
- Check interactions
- Compare alternatives
- Reviews (2)
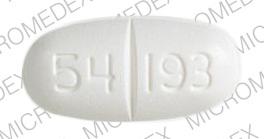
- Drug images
- Dosage information
- During pregnancy
- Generic availability
- Drug class: NNRTIs
- Breastfeeding
Patient resources
Professional resources
Other formulations
Related treatment guides
References
1. Gangar M, Arias G, O'Brien JG, Kemper CA. Frequency of cutaneous reactions on rechallenge with nevirapine and delavirdine. Ann Pharmacother. 2000;34:839-42.
2. Conway B. Initial therapy with protease inhibitor-sparing regimens: Evaluation of nevirapine and delavirdine. Clin Infect Dis. 2000;30:s130-4.
3. DeLuca A, Baldini F, Cingolani A, DiGiambenedetto S, Zaccarelli M, Tozzi V, Ammassari A, Murri R, Antinori A. Benefits and risks of switching from protease inhibitors to nevirapine with stable background therapy in patients with low or undetectable viral load: a multicentre study. Aids. 2000;14:1655-6.
4. Barreiro P, Soriano V, Casas E, Estrada V, Tellez MJ, Hoetelmans R, deRequena DG, JimenezNacher I, GonzalezLahoz J. Prevention of nevirapine-associated exanthema using slow dose escalation and/or corticosteroids. Aids. 2000;14:2153-7.
5. BersoffMatcha SJ, Miller WC, Aberg JA, vanderHorst C, Hamrick HJ, Powderly WG, Mundy LM. Sex differences in nevirapine rash. Clin Infect Dis. 2001;32:124-9.
6. Metry DW, Lahart CJ, Farmer KL, Hebert AA. Stevens-Johnson syndrome caused by the antiretroviral drug nevirapine. J Am Acad Dermatol. 2001;44:354-7.
7. Moyle G. The emerging roles of non-nucleoside reverse transcriptase inhibitors in antiretroviral therapy. Drugs. 2001;61:19-26.
8. Prakash M, Poreddy V, Tiyyagura L, Bonacini M. Jaundice and hepatocellular damage associated with nevirapine therapy. Am J Gastroenterol. 2001;96:1571-4.
9. Claudio GA, Martin AF, de Dios Perrino S, Velasco AA. DRESS syndrome associated with nevirapine therapy. Arch Intern Med. 2001;161:2501-2.
10. Gonzalez De Requena D, Nunez M, Jimenez-Nacher I, Soriano V. Liver toxicity caused by nevirapine. AIDS. 2002;16:290-1.
11. Bonnet F, Lawson-Ayayi S, Thiebaut R, et al. A cohort study of nevirapine tolerance in clinical practice: French aquitaine cohort, 1997-1999. Clin Infect Dis. 2002;35:1231-7.
12. De Vries-Sluijs T, Dieleman J, Arts D, et al. Low Nevirapine Plasma Concentrations Predict Virological Failure in an Unselected HIV-1-Infected Population. Clin Pharmacokinet. 2003;42:599-605.
13. Gil P, de Gorgolas M, Estrada V, et al. Long-Term Efficacy and Safety of Protease Inhibitor Switching to Nevirapine in HIV-Infected Patients with Undetectable Virus Load. Clin Infect Dis. 2004;39:1024-9.
14. Timmermans S, Tempelman C, Godfried MH, et al. Nelfinavir and nevirapine side effects during pregnancy. AIDS. 2005;19:795-799.
15. Cerner Multum, Inc. UK Summary of Product Characteristics.
16. Piacenti FJ. An update and review of antiretroviral therapy. Pharmacotherapy. 2006;26:1111-33.
17. von Hentig N, Carlebach A, Gute P, et al. A comparison of the steady-state pharmacokinetics of nevirapine in men, nonpregnant women and women in late pregnancy. Br J Clin Pharmacol. 2006;62:552-9.
18. Gallant JE. Drug resistance after failure of initial antiretroviral therapy in resource-limited countries. Clin Infect Dis. 2007;44:453-5.
19. Maggiolo F, Arici C, Airoldi M, et al. Reasons for discontinuation of nevirapine-containing HAART: results from an unselected population of a large clinical cohort. J Antimicrob Chemother. 2007;59:569-72.
20. Sankatsing SU, Schouten WE. Diffuse interstitial pulmonary opacities induced by nevirapine. AIDS. 2007;21:1993-4.
21. Cerner Multum, Inc. Australian Product Information.
22. Borras-Blasco J, Navarro-Ruiz A, Borras C, Castera E. Adverse cutaneous reactions associated with the newest antiretroviral drugs in patients with human immunodeficiency virus infection. J Antimicrob Chemother. 2008;62:879-88.
23. Drugs for HIV infection. Treat Guidel Med Lett. 2009;7:11-22.
24. Panel on Antiretroviral Therapy and Medical Management. Guidelines for the use of antiretroviral agents in pediatric HIV infection. https://aidsinfo.nih.gov/contentfiles/lvguidelines/pediatricguidelines.pdf 2017.
25. Product Information. Viramune XR (nevirapine). Boehringer Ingelheim. 2017.
26. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents Living with HIV https://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf 2018.
27. Daquila RT, Hughes MD, Johnson VA, et al. Nevirapine, zidovudine, and didanosine compared with zidovudine and didanosine in patients with HIV-1 infection - a randomized, double-blind, placebo-controlled trial. Ann Intern Med. 1996;124:1019-30.
28. Product Information. Viramune (nevirapine). Boehringer-Ingelheim. 2001;PROD.
29. Martinez E, Blanco JL, Arnaiz JA, PerezCuevas JB, Mocroft A, Cruceta A, Marcos MA, Milinkovic A, GarciaViejo MA, Mallolas J,. Hepatotoxicity in HIV-1-infected patients receiving nevirapine-containing antiretroviral therapy. Aids. 2001;15:1261-8.
30. Antinori A, Baldini F, Girardi E, Cingolani A, Zaccarelli M, DiGiambenedetto S, Barracchini A, DeLongis P, Murri R, Tozzi V, Ammas. Female sex and the use of anti-allergic agents increase the risk of developing cutaneous rash associated with nevirapine therapy. Aids. 2001;15:1579-81.
31. Fagot JP, Mockenhaupt M, Bouwes-Bavinck JN, Naldi L, Viboud C, Roujeau JC. Nevirapine and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. AIDS. 2001;15:1843-1848.
32. Wong KH, Chan KC, Lee SS. Sex differences in nevirapine rash. Clin Infect Dis. 2001;33:2096-7.
33. Drugs for HIV infection. Med Lett Drugs Ther. 2001;43:103-8.
34. Johnson S, Chan J, Bennett CL. Hepatotoxicity after prophylaxis with a nevirapine-containing antiretroviral regimen. Ann Intern Med. 2002;137:146-7.
35. Sanne I, Mommeja-Marin H, Hinkle J, et al. Severe Hepatotoxicity Associated with Nevirapine Use in HIV-Infected Subjects. J Infect Dis. 2005;191:825-9.
36. Liechty CA, Solberg P, Mwima G, Were W, Weidle PJ, Mermin J. Nevirapine-induced Stevens-Johnson syndrome in a mother and son. AIDS. 2005;19:993-994.
37. Joy S, Poi M, Hughes L, et al. Third-trimester maternal toxicity with nevirapine use in pregnancy. Obstet Gynecol. 2005;106:1032-8.
38. Joao EC, Calvet GA, Menezes JA, et al. Nevirapine toxicity in a cohort of HIV-1-infected pregnant women. Am J Obstet Gynecol. 2006;194:199-202.
39. Dahri K, Ensom MH. Efavirenz and Nevirapine in HIV-1 Infection : Is There a Role for Clinical Pharmacokinetic Monitoring? Clin Pharmacokinet. 2007;46:109-32.
40. Sidoroff A, Dunant A, Viboud C, et al. Risk factors for acute generalized exanthematous pustulosis (AGEP)-results of a multinational case-control study (EuroSCAR). Br J Dermatol. 2007;157:989-96.
41. Warnke D, Barreto J, Temesgen Z. Antiretroviral drugs. J Clin Pharmacol. 2007;47:1570-9.
42. CDC. Centers for Disease Control. Serious adverse events attributed to nevirapine regimens for postexposure prophylaxis after HIV exposures--worldwide, 1997--2000. MMWR Morb Mortal Wkly Rep. 2001;49(51):1153-6.
43. Das S, Allan PS, Wade AA. Adverse effects of nevirapine. Lancet. 2001;358:506; discussion 506.
44. Puro V, Soldani F, De Carli G, Lazarevic Z, Mattioli F, Ippolito G. Drug-induced aminotransferase alterations during antiretroviral HIV post-exposure prophylaxis. AIDS. 2003;17:1988-90.
45. Anderson PL. Pharmacologic perspectives for once-daily antiretroviral therapy. Ann Pharmacother. 2004;38:1969-70.
46. Peyriere H, Dereure O, Breton H, et al. Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist? Br J Dermatol. 2006;155:422-8.
47. Haas DW, Bartlett JA, Andersen JW, et al. Pharmacogenetics of nevirapine-associated hepatotoxicity: an adult AIDS clinical trials group collaboration. Clin Infect Dis. 2006;43:783-6.
48. Manfredi R, Calza L. Nevirapine versus efavirenz in 742 patients: no link of liver toxicity with female sex, and a baseline CD4 cell count greater than 250 cells/mul. AIDS. 2006;20:2233-2236.
49. Rivero A, Mira JA, Pineda JA. Liver toxicity induced by non-nucleoside reverse transcriptase inhibitors. J Antimicrob Chemother. 2007;59:342-6.
50. Soriano V, Puoti M, Sulkowski M, et al. Care of patients coinfected with HIV and hepatitis C virus: 2007 updated recommendations from the HCV-HIV International Panel. AIDS. 2007;21:1073-89.
51. Clarke S, Harrington P, Barry M, Mulcahy F. The tolerability of efavirenz after nevirapine-related adverse events. Clin Infect Dis. 2000;31:806-7.
52. Raffi F, Lewden C, Chene G. Is nevirapine-based therapy discontinuation in hepatitis C co-infected patients a more important mortality determinant than hypersensitivity. AIDS. 2008;22:435-6.
53. Dube M, Fenton M. Lipid abnormalities. Clin Infect Dis. 2003;36(Suppl 2):S79-83.
54. Panos G, Kopterides P, Falagas ME. Hyperlactatemia due to nevirapine. Ann Intern Med. 2006;145:867-8.
55. Pandie M, Sonderup M, Meissner P, Mendelson M. Acute porphyria precipitated by nevirapine. AIDS. 2010;24:2597-9.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.