Liothyronine Side Effects
Medically reviewed by Drugs.com. Last updated on Aug 12, 2024.
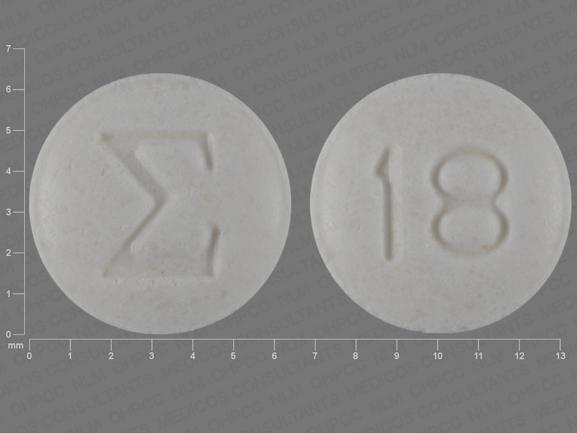
Applies to liothyronine: oral tablet.
Other dosage forms:
Important warnings
This medicine can cause some serious health issues
Oral route (tablet)
Thyroid hormones, including liothyronine sodium, either alone or with other therapeutic agents, should not be used for the treatment of obesity or for weight loss.
In euthyroid patients, doses within the range of daily hormonal requirements are ineffective for weight reduction.
Larger doses may produce serious or even life-threatening manifestations of toxicity, particularly when given in association with sympathomimetic amines such as those used for their anorectic effects.
Serious side effects of liothyronine
Along with its needed effects, liothyronine may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking liothyronine:
Incidence not known
- anxiety
- arm, back, or jaw pain
- blurred or double vision
- chest pain or discomfort
- chest tightness or heaviness
- crying
- decreased bone mineral density
- decreased urine output
- delusions of persecution, mistrust, suspiciousness, or combativeness
- diarrhea
- difficulty breathing
- dilated neck vein
- dizziness
- excessive
- sweating
- extreme tiredness or weakness
- eye pain
- fainting
- false or unusual sense of well-being
- fast, pounding, or irregular heartbeat or pulse
- feeling of discomfort
- feeling of unreality
- fever
- headache
- heat intolerance
- impaired fertility
- increased appetite
- increased blood pressure
- irregular breathing
- irritability
- itching, skin rash
- joint swelling
- limp pain in the hip or knee
- menstrual changes
- mental depression
- muscle aches, weakness, or cramps
- nausea
- nervousness
- pain or discomfort in the arms, jaw, back, or neck
- quick to react or overreact emotionally
- rapidly changing moods
- restlessness
- sense of detachment from self or body
- severe headache
- slow heartbeat
- stomach cramps
- swelling of the face, fingers, feet, or lower legs
- swollen lymph glands
- tremors
- trouble sitting still
- trouble sleeping
- vomiting
- weight gain or loss
Get emergency help immediately if any of the following symptoms of overdose occur while taking liothyronine:
Symptoms of overdose
- cold, clammy skin
- confusion about identity, place, and time
- difficulty in speaking
- dizziness
- double vision
- fast, weak pulse
- headache
- inability to move the arms, legs, or facial muscles
- inability to speak
- lightheadedness
- loss of consciousness
- nervousness
- seizure
- sensitivity to heat
- slow speech
- sweating
- trouble sleeping
- weight loss
Other side effects of liothyronine
Some side effects of liothyronine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Incidence not known
- feeling of warmth
- hair loss
- redness of the face, neck, arms, and occasionally, upper chest
For healthcare professionals
Applies to liothyronine: compounding powder, intravenous solution, oral tablet.
General
Reported side effects are usually indicative of excessive dosage and will usually disappear when the dose is reduced or treatment is stopped.[Ref]
Cardiovascular
- Common (1% to 10%): Arrhythmia, tachycardia, cardiopulmonary arrest, hypotension, myocardial infarction
- Frequency not reported: Angina, congestive heart failure, hypertension, flushing, palpitation[Ref]
Nervous system
- Frequency not reported: Headache, tremor, benign intracranial hypertension[Ref]
Dermatologic
Musculoskeletal
- Frequency not reported: Twitching, muscle cramps, muscle weakness, craniostenosis, premature closure of epiphysis[Ref]
Gastrointestinal
- Frequency not reported: Diarrhea, vomiting[Ref]
Immunologic
- Frequency not reported: Hypersensitivity reaction[Ref]
Local
- Frequency not reported: Phlebitis[Ref]
Psychiatric
Genitourinary
- Frequency not reported: Menstruation irregular[Ref]
Other
- Frequency not reported: Fever, edema, weight loss, heat intolerance[Ref]
References
1. (2001) "Product Information. Cytomel (liothyronine)." Monarch Pharmaceuticals Inc
2. (2005) "Product Information. Triostat (liothyronine)." JHP Pharmaceuticals
3. Cerner Multum, Inc. "UK Summary of Product Characteristics."
4. Cerner Multum, Inc. "Australian Product Information."
More about liothyronine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (97)
- Drug images
- Dosage information
- During pregnancy
- Drug class: thyroid drugs
- Breastfeeding
- En español
Patient resources
- Liothyronine drug information
- Liothyronine (Intravenous) (Advanced Reading)
- Liothyronine (Oral) (Advanced Reading)
- Liothyronine Tablets
- Liothyronine Injection
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Liothyronine side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.