Intelence Side Effects
Generic name: etravirine
Medically reviewed by Drugs.com. Last updated on Jun 20, 2023.
Note: This document contains side effect information about etravirine. Some dosage forms listed on this page may not apply to the brand name Intelence.
Applies to etravirine: oral tablet.
Serious side effects of Intelence
Along with its needed effects, etravirine (the active ingredient contained in Intelence) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking etravirine:
More common
- Rash
Less common
- Blurred vision
- burning, numbness, tingling, or painful sensations
- dizziness
- headache
- nervousness
- pounding in the ears
- slow or fast heartbeat
- unsteadiness or awkwardness
- weakness in the arms, hands, legs, or feet
Rare
- Blistering, peeling, or loosening of the skin
- chills
- cough
- diarrhea
- fever
- hives, itching
- hoarseness
- irritation
- joint pain, stiffness, or swelling
- muscle pain
- red skin lesions, often with a purple center
- red, irritated eyes
- redness of the skin
- sore throat
- sores, ulcers, or white spots in the mouth or on the lips
- swelling of the eyelids, face, lips, hands, or feet
- tightness in the chest
- trouble with breathing or swallowing
- unusual tiredness or weakness
Incidence not known
- Dark urine
- general feeling of tiredness or weakness
- headache
- light-colored stools
- stomach pain, continuing
- swollen, painful, or tender lymph glands in the neck, armpit, or groin
- vomiting
- yellow eyes or skin
Other side effects of Intelence
Some side effects of etravirine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common
- Stomach pain
For Healthcare Professionals
Applies to etravirine: oral tablet.
General
The safety report of this drug is based on 599 HIV-1-infected, therapy-experienced patients receiving 200 mg twice daily in combination with background regimen; the median exposure was 52.3 weeks. The most commonly reported side effects (of all intensities) were rash, diarrhea, nausea, and headache. Discontinuation due to side effects occurred in 5.2% of patients using this drug; a total of 2.2% of HIV-1-infected patients in phase 3 trials discontinued this drug due to rash.[Ref]
Hepatic
Grade 2 or higher abnormalities representing a worsening from baseline of AST, ALT, and total bilirubin have been reported in 27.8%, 25%, and 7.1%, respectively, in patients coinfected with hepatitis B and/or C virus as compared to 6.7%, 7.5%, and 1.8% reported in non-coinfected patients.
Grades 2, 3, and 4 elevated ALT have been reported in 6%, 3%, and 1% of patients, respectively. Grades 2, 3, and 4 elevated AST have been reported in 6%, 3%, and less than 1% of patients, respectively.[Ref]
Very common (10% or more): Worsening from baseline of AST (up to 27.8%), worsening from baseline of ALT (up to 25%)
Common (1% to 10%): Worsening from baseline of total bilirubin, elevated ALT, elevated AST
Uncommon (0.1% to 1%): Hepatomegaly, cytolytic hepatitis, hepatic steatosis, hepatitis
Frequency not reported: Hepatic failure[Ref]
Other
Very common (10% or more): Elevated total cholesterol (up to 20%), elevated low-density lipoprotein (up to 13%)
Common (1% to 10%): Elevated triglycerides, fatigue
Uncommon (0.1% to 1%): Sluggishness
Frequency not reported: Pyrexia
Antiretroviral therapy:
-Frequency not reported: Increased weight[Ref]
Grades 2 and 3 elevated total cholesterol have been reported in 20% and 8% of patients, respectively. Grades 2 and 3 elevated low-density lipoprotein have been reported in 13% and 7% of patients, respectively. Grades 2, 3, and 4 elevated triglycerides have been reported in 9%, 6%, and 4% of patients, respectively.[Ref]
Dermatologic
Very common (10% or more): Rash (up to 19.2%)
Common (1% to 10%): Night sweats, lipohypertrophy, prurigo, dry skin
Uncommon (0.1% to 1%): Hyperhidrosis, face swelling, angioneurotic edema, erythema multiforme, acquired lipodystrophy
Rare (0.01% to 0.1%): Stevens-Johnson syndrome
Very rare (less than 0.01%): Toxic epidermal necrolysis
Frequency not reported: Contact dermatitis, erythema, pruritus
Postmarketing reports: Toxic epidermal necrolysis (fatal cases), Stevens-Johnson syndrome (fatal cases), drug rash with eosinophilia and systemic symptoms (DRESS)[Ref]
During clinical trials, rash generally was mild to moderate, occurred chiefly in the second week of therapy, and was infrequent after the fourth week. Rash usually resolved within 1 to 2 weeks on continued use of the drug. The incidence of rash was higher in women taking this drug (at least grade 2 rash: 15%) compared to men (at least grade 2 rash: 9.5%). Discontinuation due to rash occurred in 5% of women compared to 1.9% of men. Patients with a history of nonnucleoside reverse transcriptase inhibitor-related rash did not appear to be at increased risk.[Ref]
Gastrointestinal
Grades 2, 3, and 4 elevated pancreatic amylase have been reported in 7%, 7%, and 2% of patients, respectively. Grades 2, 3, and 4 elevated lipase have been reported in 4%, 2%, and 1% of patients, respectively.[Ref]
Very common (10% or more): Diarrhea (up to 18%), nausea (up to 14.9%)
Common (1% to 10%): Elevated pancreatic amylase, elevated lipase, abdominal pain, vomiting, gastroesophageal reflux disease, flatulence, gastritis, abdominal distension, constipation, dry mouth, stomatitis, elevated blood amylase
Uncommon (0.1% to 1%): Pancreatitis, hematemesis, retching[Ref]
Metabolic
Very common (10% or more): Elevated glucose levels (up to 15%)
Common (1% to 10%): Hypertriglyceridemia, hypercholesterolemia, hyperlipidemia, hyperglycemia, diabetes mellitus, anorexia, dyslipidemia
Antiretroviral therapy:
-Frequency not reported: Increased blood lipid levels, increased glucose levels[Ref]
Grades 2 and 3 elevated glucose levels have been reported in 15% and 4% of patients, respectively.[Ref]
Nervous system
Very common (10% or more): Headache (up to 10.9%)
Common (1% to 10%): Peripheral neuropathy, somnolence, paresthesia, hypoesthesia, amnesia
Uncommon (0.1% to 1%): Convulsion, syncope, disturbance in attention, hypersomnia, tremor, vertigo, hemorrhagic stroke[Ref]
Renal
Grades 2 and 3 elevated creatinine have been reported in 6% and 2% of patients, respectively.[Ref]
Common (1% to 10%): Elevated creatinine, renal failure[Ref]
Hematologic
Common (1% to 10%): Decreased neutrophils, decreased platelet count, decreased hemoglobin, decreased WBC count, anemia, thrombocytopenia
Frequency not reported: Hemolytic anemia[Ref]
Grades 2, 3, and 4 decreased neutrophils have been reported in 5%, 4%, and 2% of patients, respectively. Grades 2, 3, and 4 decreased platelet count have been reported in 3%, 1%, and less than 1% of patients, respectively. Grades 2, 3, and 4 decreased hemoglobin have been reported in 2%, less than 1%, and less than 1% of patients, respectively. Grades 2, 3, and 4 decreased WBC count have been reported in 2%, 1%, and 1% of patients, respectively.[Ref]
Cardiovascular
Common (1% to 10%): Hypertension, myocardial infarction
Uncommon (0.1% to 1%): Angina pectoris, atrial fibrillation
Frequency not reported: Mild atrioventricular block[Ref]
Psychiatric
Common (1% to 10%): Insomnia, anxiety, sleep disorders
Uncommon (0.1% to 1%): Abnormal dreams, confusional state, disorientation, nervousness, nightmares[Ref]
Ocular
Common (1% to 10%): Blurred vision[Ref]
Respiratory
Common (1% to 10%): Exertional dyspnea
Uncommon (0.1% to 1%): Bronchospasm[Ref]
Hypersensitivity
Uncommon (0.1% to 1%): Drug hypersensitivity
Postmarketing reports: Severe hypersensitivity reactions (including DRESS and cases of hepatic failure)[Ref]
Immunologic
Uncommon (0.1% to 1%): Immune reconstitution syndrome
Frequency not reported: Autoimmune disorders in the setting of immune reconstitution (e.g., Graves' disease, polymyositis, Guillain-Barre syndrome, autoimmune hepatitis)[Ref]
Endocrine
Uncommon (0.1% to 1%): Gynecomastia[Ref]
Musculoskeletal
Frequency not reported: Severe myopathy (including articular pain, muscular pain, weakness, stiffness, increased creatine kinase)
Postmarketing reports: Rhabdomyolysis
Combination antiretroviral therapy:
-Frequency not reported: Osteonecrosis[Ref]
More about Intelence (etravirine)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
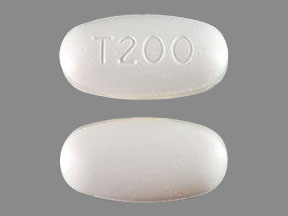
- Drug images
- Dosage information
- During pregnancy
- Generic availability
- FDA approval history
- Drug class: NNRTIs
- Breastfeeding
- En español
Patient resources
Professional resources
Related treatment guides
References
1. Cerner Multum, Inc. UK Summary of Product Characteristics.
2. Product Information. Intelence (etravirine). Ortho Biotech Inc. 2008.
3. Anti-HIV agents. Effectiveness of etravirine in treatment-experienced PHAs. TreatmentUpdate. 2007;19:3-5.
4. Etravirine: R165335, TMC 125, TMC-125, TMC125. Drugs R D. 2006;7:367-73.
5. Cerner Multum, Inc. Australian Product Information.
6. Etravirine(Intelence) for HIV infection. Med Lett Drugs Ther. 2008;50:47-8.
7. Cohen CJ, Berger DS, Blick G, et al. Efficacy and safety of etravirine (TMC125) in treatment-experienced HIV-1-infected patients: 48-week results of a phase IIb trial. AIDS. 2009;23:423-6.
8. Johnson LB, Saravolatz LD. Etravirine, a Next-Generation Nonnucleoside Reverse-Transcriptase Inhbitor. Clin Infect Dis. 2009.
9. Drugs for HIV infection. Treat Guidel Med Lett. 2009;7:11-22.
10. Peeters M, Janssen K, Kakuda TN, et al. Etravirine Has No Effect on QT and Corrected QT Interval in HIV-Negative Volunteers (June). Ann Pharmacother. 2008.
11. Borras-Blasco J, Navarro-Ruiz A, Borras C, Castera E. Adverse cutaneous reactions associated with the newest antiretroviral drugs in patients with human immunodeficiency virus infection. J Antimicrob Chemother. 2008;62:879-88.
12. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. Department of Health and Human Services. https://aidsinfo.nih.gov/contentfiles/lvguidelines/adultandadolescentgl.pdf 2019.
13. Anti-HIV agents. Brain side effects not common with etravirine. TreatmentUpdate. 2007;19:6-7.
14. Gruzdev B, Rakhmanova A, Doubovskaya E, et al. A randomized, double-blind, placebo-controlled trial of TMC125 as 7-day monotherapy in antiretroviral naive, HIV-1 infected subjects. AIDS. 2003;17:2487-94.
15. Tommasi C, Tempestilli M, Fezza R, et al. A rare case of severe myopathy associated with etravirine use. AIDS. 2010;24:1088-90.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.