Sirolimus (Monograph)
Brand name: Rapamune
Drug class: mTOR Inhibitors, Miscellaneous
Warning
- Immunosuppression
-
Immunosuppression may result in increased susceptibility to infection and possible development of lymphoma or other malignancies.
-
Only clinicians experienced in immunosuppressive therapy and management of renal transplant patients should prescribe sirolimus for prophylaxis of organ rejection in patients receiving renal transplants.
-
Patients should be managed in facilities equipped and staffed with adequate laboratory and supportive medical resources; the clinician responsible for maintenance therapy should have complete information for patient follow-up.
- Use Not Recommended in Liver or Lung Transplant Patients
-
Safety and efficacy of sirolimus as immunosuppressive therapy not established in liver or lung transplant patients; such use is not recommended.
-
Use of sirolimus in combination with tacrolimus associated with excess mortality and graft loss in de novo liver transplant recipients; concurrent use of sirolimus with cyclosporine or tacrolimus associated with an increased risk of hepatic artery thrombosis.
-
Cases of bronchial anastomotic dehiscence, most fatal, reported in de novo lung transplant patients when sirolimus was used as part of an immunosuppressive regimen.
Introduction
Mammalian target of rapamycin (mTOR) inhibitor; immunosuppressive agent.
Uses for Sirolimus
Renal Allotransplantation
Prevention of renal allograft rejection in patients ≥13 years of age. The manufacturer recommends therapeutic drug monitoring in all patients receiving the drug.
In patients at low to moderate immunologic risk, it is recommended that sirolimus be used initially with both cyclosporine and corticosteroids; cyclosporine should be withdrawn 2–4 months after transplantation.
In patients at high immunologic risk (defined as Black recipients and/or repeat renal transplant recipients who lost a previous allograft for immunologic reasons and/or patients with high panel-reactive antibodies), it is recommended that sirolimus be used in combination with cyclosporine and corticosteroids for the first year following transplantation.
Safety and efficacy not established in patients <13 years old, or in pediatric renal transplant patients considered at high immunologic risk.
Safety and efficacy of de novo use of sirolimus without cyclosporine not established.
Safety and efficacy of conversion from calcineurin inhibitors (e.g., cyclosporine, tacrolimus) to sirolimus in maintenance renal transplant patients not established.
KDIGO clinical practice guideline states that immunosuppressive medication recommendations are complex as combinations of multiple drug classes are utilized and choices between varying regimens are determined through an evaluation of benefits and harms.
KDIGO recommends that if mTOR inhibitors including sirolimus are used, these agents should not be initiated until graft function is established and surgical wounds are healed.
The KDIGO guideline also states that mTOR inhibitors do not improve patient outcomes when administered either as replacement agents for calcineurin inhibitors or antiproliferative agents, or as add-on therapy, and possess significant acute and chronic adverse effects (e.g., dyslipidemia, bone marrow suppression).
Consensus recommendations from the ACCP, AST, and the ISHLT state there is no standardized approach to maintenance immunosuppression management in solid organ transplantation and a variety of factors may impact the choice of agents including the transplanted organ, center-specific protocols, provider expertise, insurance and cost issues, and patient characteristics and tolerability of therapy.
The consensus recommendations also state that mTOR inhibitors are not commonly utilized as first line maintenance immunosuppression but rather as second-line therapy in place of or in combination with other first line agents for various indications.
Lymphangioleiomyomatosis
Treatment of lymphangioleiomyomatosis (LAM).
The American Thoracic Society and Japanese Respiratory Society clinical practice guideline for the diagnosis and management of LAM strongly recommends treatment with sirolimus rather than observation for patients with LAM with abnormal/declining lung function.
The guideline also conditionally recommends treatment with sirolimus for selected patients with LAM with problematic chylous effusions prior to invasive management.
Hepatic Transplantation
Prevention of rejection of liver allografts† [off-label].
The manufacturer states that safety and efficacy as immunosuppressive therapy have not been established in liver transplant patients and that such use is therefore not recommended.
Associated with adverse outcomes in patients following liver transplantation, including excess mortality, graft loss, and hepatic artery thrombosis when used in combination with other immunosuppressants (e.g., cyclosporine, tacrolimus).
Lung Transplantation
Prevention of rejection of lung allografts† [off-label].
The manufacturer states that safety and efficacy as immunosuppressive therapy have not been established in lung transplant patients and that such use is therefore not recommended.
Cases of bronchial anastomotic dehiscence, mostly fatal, reported in de novo lung transplant patients who received sirolimus in combination with other immunosuppressants.
Heart Transplantation
Prevention of rejection of heart allografts† [off-label]. May offer benefit in heart transplant patients with reduced or withdrawn calcineurin inhibitor therapy by stabilizing or modestly improving renal function and by decreasing the incidence and/or reducing progression of chronic allograft vasculopathy.
Pancreas Transplantation
Prevention of rejection of pancreas allografts† [off-label] (often performed simultaneously with a kidney transplant). The 2022 ACCP, AST, and ISHLT consensus recommendations for use of maintenance immunosuppression in solid organ transplantation state that replacing a calcineurin inhibitor with an mTOR inhibitor and mycophenolic acid with or without corticosteroids in pancreas transplant patients can result in improvement of calcineurin-associated renal toxicity with minimal impact on allograft and patient survival.
Intestinal Transplantation
Prevention of rejection of intestinal allografts† [off-label]. Associated with a beneficial impact on graft rejection or dysfunction in some studies.
Other Uses
Prevent rejection of vascular composite allografts.
Sirolimus Dosage and Administration
General
Patient Monitoring
-
Monitoring of sirolimus trough concentrations is recommended for all patients, and should be used to adjust sirolimus therapy in conjunction with clinical and laboratory parameters.
-
Examine patients for skin changes periodically.
-
Monitor for signs and symptoms of infection; including reactivation of latent viral infections.
-
Perform routine laboratory testing for assessment of renal function and monitoring of lipids and urinary proteins).
Administration
Oral Administration
Administer orally once daily. Give consistently with or without food to minimize variability of systemic exposure.
Do not crush, chew, or split tablets; use oral solution in patients unable to take tablets.
Although commercially available tablets and oral solution are not bioequivalent, manufacturer states that 2 mg doses given as conventional tablets and as oral solution are therapeutically equivalent and may be interchangeable on a mg-per-mg basis at doses ≤2 mg. Not known whether these formulations are therapeutically equivalent at doses >2 mg.
Administer sirolimus 4 hours after administration of cyclosporine formulations for emulsion (modified), since concomitant administration increases rate and extent of sirolimus absorption.
Dilution and Administration of Oral Solution
Consult manufacturer’s instructions regarding insertion of adapter assembly into bottle and withdrawal of prescribed dose (using syringe provided by manufacturer).
Empty contents of syringe into a glass or plastic cup containing ≥60 mL of water or orange juice; stir vigorously for 1 minute and administer immediately. Refill container with ≥120 mL of the diluent, stir vigorously, and ingest rinse solution. Use only glass or plastic containers. Do not administer with grapefruit juice or use grapefruit juice as diluent (see Interactions); do not use apple juice or other liquids as diluents. Use syringe once and then discard.
If mouth of bottle must be wiped clean, use dry cloth to avoid introducing water or other liquid into the bottle.
Dosage
When used for the prevention of renal allograft rejection, frequent sirolimus dosage adjustments based on non-steady-state sirolimus concentrations can lead to overdosing or underdosing since sirolimus has a long half-life. Once maintenance dosage is adjusted, maintain patient on the new dosage for at least 7–14 days before making subsequent dosage adjustment based on drug concentrations.
In most patients, dose adjustments can be estimated based on the following equation:
New sirolimus dose = current sirolimus dose × (target concentration / current concentration)
A loading dose should be considered in addition to a new maintenance dose when it is necessary to increase trough sirolimus concentrations. Estimate the loading dose based on the following equation:
Sirolimus loading dose = 3 × (new maintenance dose - current maintenance dose)
Do not give >40 mg of sirolimus within any 1-day period. If an estimated daily dose is >40 mg because of the addition of a loading dose, give loading dose over a 2-day period. The manufacturer recommends monitoring trough whole blood concentrations of sirolimus at least 3–4 days after administering loading dose(s).
Pediatric Patients
Renal Allotransplantation
Concomitant Sirolimus and Cyclosporine Therapy in Patients at Low to Moderate Immunologic Risk
OralChildren ≥13 years of age who weigh ≥40 kg: Loading dose should be equivalent to 3 times the maintenance dosage; e.g., 6 mg as a loading dose in de novo renal transplant recipients and a maintenance dosage of 2 mg daily. No efficacy advantage with higher loading and maintenance dosages (loading dose of 15 mg followed by a maintenance dosage of 5 mg daily) in overall patient population. 2-mg daily maintenance dosage associated with a superior safety profile compared with the 5-mg daily dosage.
Children ≥13 years of age who weigh <40 kg: Initially, 3 mg/m2 as a loading dose in de novo renal transplant recipients. Maintenance dosage of 1 mg/m2 daily.
Therapeutic drug monitoring recommended in all patients to maintain sirolimus blood concentrations within the recommended range.
Sirolimus Therapy following Cyclosporine Withdrawal in Patients at Low to Moderate Immunologic Risk
OralChildren ≥13 years of age: As cyclosporine is gradually discontinued over a 4- to 8-week period, increase sirolimus dosage to maintain target trough whole blood concentrations of 16–24 ng/mL for the first year post-transplantation. Thereafter, target sirolimus concentrations should be 12–20 ng/mL.
Patients at High Immunologic Risk
OralChildren ≥13 years of age who weigh ≥40 kg receiving concomitant sirolimus and cyclosporine therapy: Loading dose of ≤15 mg on day 1 post-transplantation. On day 2, initial maintenance dosage of 5 mg daily. Obtain trough sirolimus concentration between days 5 and 7; adjust maintenance dosage as necessary.
Initially, cyclosporine dosage of up to 7 mg/kg daily given in divided doses. Subsequently, adjust dosage to achieve target trough blood concentrations. Minimum prednisone dosage of 5 mg daily.
May use antibody induction therapy.
Adults
Renal Allotransplantation
Concomitant Sirolimus and Cyclosporine Therapy in Patients at Low to Moderate Immunologic Risk
OralAdults who weigh ≥40 kg: Loading dose should be equivalent to 3 times the maintenance dosage; e.g., 6 mg as a loading dose in de novo renal transplant recipients and a maintenance dosage of 2 mg daily. No efficacy advantage with higher loading and maintenance dosages (loading dose of 15 mg followed by a maintenance dosage of 5 mg daily) in overall patient population. 2-mg daily maintenance dosage associated with a superior safety profile compared with the 5-mg daily dosage.
Adults who weigh <40 kg: Initially, 3 mg/m2 as a loading dose in de novo renal transplant recipients. Maintenance dosage of 1 mg/m2 daily.
Therapeutic drug monitoring recommended in all patients to maintain sirolimus blood concentrations within the recommended range.
Sirolimus Therapy following Cyclosporine Withdrawal in Patients at Low to Moderate Immunologic Risk
OralAs cyclosporine is gradually discontinued over a 4- to 8-week period, increase sirolimus dosage to maintain target trough whole blood concentrations of 16–24 ng/mL for the first year post transplantation. Thereafter, target sirolimus concentrations should be 12–20 ng/mL.
Patients at High Immunologic Risk
OralAdults who weigh ≥40 kg receiving concomitant sirolimus and cyclosporine therapy: Loading dose of ≤15 mg on day 1 post-transplantation. On day 2, initial maintenance dosage of 5 mg daily. Obtain trough sirolimus concentration between days 5 and 7; adjust maintenance dosage as necessary.
Initially, cyclosporine dosage of up to 7 mg/kg daily given in divided doses. Subsequently, adjust dosage to achieve target trough blood concentrations. Minimum prednisone dosage of 5 mg daily.
May use antibody induction therapy.
Lymphangioleiomyomatosis
OralInitially, 2 mg daily. Obtain whole blood trough concentrations in 10–20 days; adjust dosage to maintain concentrations between 5–15 ng/mL. If subsequent dosage adjustment is required, the manufacturer states that the new dose can be estimated based on the following equation:
new sirolimus dose = current sirolimus dose × (target concentration ÷ current concentration)
The manufacturer cautions that frequent sirolimus dosage adjustments based on non-steady-state sirolimus concentrations can lead to overdosing or underdosing since sirolimus has a long half-life. Once the maintenance dosage is adjusted, maintain the patient on the new sirolimus dosage for at least 7–14 days before subsequent dosage adjustment is made based on drug concentrations. Once a stable dose is achieved, perform therapeutic drug monitoring at least every 3 months.
Special Populations
Hepatic Impairment
Reduce maintenance dosage by approximately one-third in patients with mild or moderate hepatic impairment and by approximately one-half in patients with severe hepatic impairment; loading dose does not require modification.
Renal Impairment
Dosage adjustment is not necessary.
Low Body Weight
The initial dosage of sirolimus for the prevention of renal allograft rejection in patients ≥13 years of age who weigh <40 kg should be 1 mg/m2 daily based on body surface area, with a loading dose of 3 mg/m2
Geriatric Patients
Routine dosage adjustment based solely on advanced age does not appear to be necessary. However, manufacturer recommends cautious dosage selection, usually starting at lower end of dosage range, reflecting the greater frequency of decreased hepatic or cardiac function and of concomitant diseases or other drug therapy in this population.
Cautions for Sirolimus
Contraindications
-
Known hypersensitivity to sirolimus or its derivatives or any ingredient in the sirolimus formulation.
Warnings/Precautions
Warnings
Increased Susceptibility to Infection and Possible Development of Lymphoma
Possible increased susceptibility to infection (including opportunistic infections [e.g., tuberculosis], fatal infections, and sepsis) and possible development of lymphoma or other malignancies, particularly of the skin. (See Boxed Warning.)
Excess Mortality, Graft Loss, and Hepatic Artery Thrombosis in Liver Transplant Patients
Use in combination with other immunosuppressants (e.g., cyclosporine, tacrolimus) associated with increased risk of hepatic artery thrombosis, graft loss, and death in de novo liver transplant recipients. (See Boxed Warning.)
Safety and efficacy of sirolimus as immunosuppressive therapy in liver transplant patients not established; such use is not recommended by manufacturer.
Bronchial Anastomotic Dehiscence in Lung Transplant Patients
Cases of bronchial anastomotic dehiscence, mostly fatal, reported in de novo lung transplant patients who received sirolimus in combination with other immunosuppressants. Safety and efficacy of sirolimus as immunosuppressive therapy in lung transplant patients not established; such use is not recommended by manufacturer. (See Boxed Warning.)
Other Warnings/Precautions
Hypersensitivity Reactions
Hypersensitivity reactions, including anaphylactic or anaphylactoid reactions, angioedema, exfoliative dermatitis, and hypersensitivity vasculitis, reported.
Angioedema
Associated with angioedema. Concurrent use of other drugs causing angioedema (e.g., ACE inhibitors, angiotensin II receptor antagonists, NSAIAs) may increase risk of developing angioedema.
Fluid Accumulation and Impairment of Wound Healing
Impaired or delayed wound healing, including lymphocele and wound dehiscence, reported. Lymphocele, a known surgical complication of renal transplantation, occurred more often in sirolimus-treated patients and appeared to be dose-related. Abnormal wound healing following transplant surgery, including fascial dehiscence, incisional hernia, and anastomotic disruption (e.g., wound, vascular, airway, ureteral, biliary), also reported.
Consider appropriate measures to minimize such complications (i.e., patient selection based on BMI, reduced sirolimus dosage, use of closed suction drains, modifications of surgical technique). Patients with a BMI >30 kg/m2 may be at increased risk of abnormal wound healing.
Fluid accumulation, including peripheral edema, lymphedema, pleural effusion, ascites, and pericardial effusions (including hemodynamically important effusions and tamponade requiring intervention in children and adults), reported.
Hyperlipidemia
Increases in serum cholesterol and triglyceride concentrations requiring treatment reported.
Monitor serum lipids; initiate appropriate treatment (diet, exercise, lipid-lowering agents, as indicated) if hyperlipidemia occurs.
Carefully consider risks/benefits of sirolimus in patients with preexisting hyperlipidemia.
In clinical trials, concomitant use of sirolimus and HMG-CoA reductase inhibitors and/or fibric acid derivatives generally was well tolerated. However, manufacturer recommends monitoring patients receiving sirolimus and cyclosporine therapy who are concurrently receiving an HMG-CoA reductase inhibitor and/or fibric acid derivative for possible development of rhabdomyolysis and other possible adverse effects (e.g., hepatic toxicity) described in the prescribing information for these antilipemic agents.
Decline in Renal Function
Increases in Scr and decreases in GFR reported in patients receiving cyclosporine and sirolimus concurrently compared with those receiving cyclosporine with placebo or azathioprine.
Monitor renal function closely in patients receiving maintenance immunosuppressive regimens that include sirolimus and cyclosporine. Consider appropriate adjustments of the immunosuppressive regimen, including discontinuance of sirolimus and/or cyclosporine, in patients with elevated or increasing Scr.
In patients with low to moderate immunologic risk, consider administering sirolimus in combination with cyclosporine for >4 months post-transplantation only if potential benefits outweigh possible risks.
Use other nephrotoxic drugs with caution. (See Interactions.)
In patients with delayed graft function, sirolimus may delay recovery of renal function.
Proteinuria
Increased urinary protein excretion commonly observed following conversion from calcineurin inhibitors (e.g., cyclosporine, tacrolimus) to sirolimus in maintenance renal transplant recipients. Safety and efficacy of such conversion not established.
Manufacturer recommends periodic quantitative monitoring of urinary protein excretion in sirolimus-treated patients. If proteinuria occurs, early treatment may help prevent long-term adverse effects on graft survival.
Latent Viral Infections
Increased risk of reactivation of latent viral infections in immunosuppressed patients, including those receiving sirolimus. (See BK Virus-associated Nephropathy [BKVN] and also Progressive Multifocal Leukoencephalopathy [PML] under Cautions.)
BK Virus-associated Nephropathy (BKVN)
BKVN observed in immunosuppressed renal transplant patients, including those receiving sirolimus. Principally observed in renal transplant patients (usually within the first year post-transplantation); may result in severe allograft dysfunction and/or graft loss. Risk appears to correlate with degree of overall immunosuppression rather than use of specific immunosuppressant.
Monitor patients for signs of BKVN (e.g., deterioration of renal function); if BKVN develops, institute early treatment and consider initially reducing immunosuppressive therapy. Treatment approaches used anecdotally include antiviral therapy (e.g., cidofovir), leflunomide, IV immunoglobulins, and fluoroquinolone antibiotics; additional experience and well-controlled studies needed to establish optimal treatment.
Progressive Multifocal Leukoencephalopathy (PML)
PML, an opportunistic viral infection of the brain caused by the polyomavirus JC (also called the JC virus), reported in patients receiving immunosuppressants, including sirolimus. Risk factors include immunosuppressive therapies and impairment of immune function.
Commonly presents with hemiparesis, apathy, confusion, cognitive impairment, and ataxia; consider possible diagnosis of PML in any immunocompromised patient experiencing neurologic manifestations. Consider consulting with a neurologist as clinically indicated.
Decreasing total immunosuppression may improve outcome, but may also increase risk of graft rejection in transplant recipients; consider the potential risks versus benefits of reduced immunosuppression in such cases. Although optimal treatment not established, antiviral agents (e.g., cidofovir) have been successfully used in the treatment of PML in several transplant recipients. Early diagnosis and rapid initiation of treatment appear essential for patient recovery.
Interstitial Lung Disease/Non-Infectious Pneumonitis
Cases of ILD (including pneumonitis, bronchiolitis obliterans organizing pneumonia [BOOP], and pulmonary fibrosis), some fatal, with no identified infectious etiology reported. In some cases, the ILD was reported with pulmonary hypertension (including pulmonary arterial hypertension [PAH]) as a secondary event. Risk may increase as trough sirolimus concentration increases. In some cases, ILD resolved upon sirolimus discontinuance or dosage reduction.
De Novo Use Without Cyclosporine
Safety and efficacy of de novo use without cyclosporine not established in renal transplant patients.
Increased Risk of Calcineurin Inhibitor-induced HUS/TTP/TMA
Concomitant use with a calcineurin inhibitor (e.g., cyclosporine, tacrolimus) may increase risk of hemolytic uremic syndrome/thrombotic thrombocytopenic purpura/thrombotic microangiopathy (HUS/TTP/TMA).
Antimicrobial Prophylaxis
Cases of Pneumocystis jiroveci (formerly Pneumocystis carinii) pneumonia reported in sirolimus-treated patients not receiving antimicrobial prophylaxis. Manufacturer recommends antimicrobial prophylaxis for P. jiroveci pneumonia for 1 year following transplantation.
Manufacturer recommends cytomegalovirus (CMV) prophylaxis for 3 months after transplantation, particularly in patients at increased risk for CMV disease.
Different Sirolimus Trough Concentration Reported between Chromatographic and Immunoassay Methodologies
Various chromatographic and immunoassay methodologies used in clinical practice to measure sirolimus whole blood concentrations. Patient sample values from different assays may not be interchangeable.
Skin Cancer
Increased risk for skin cancer with immunosuppressive therapy. Limit exposure to sunlight and other UV light; use of protective clothing, sunglasses, and broad-spectrum sunscreen with a high protection factor is recommended.
Immunizations
Avoid use of live vaccines during treatment with sirolimus including measles, mumps, rubella, oral polio, BCG, yellow fever, varicella, and TY21a typhoid. Immunosuppressants may affect response to vaccination; therefore, vaccination may be less effective during treatment with sirolimus.
Interaction with Potent Inhibitors and Inducers of CYP3A4 and/or P-glycoprotein
Avoid concurrent administration of sirolimus with potent inhibitors of CYP3A4 and/or P-glycoprotein (e.g., itraconazole, ketoconazole, voriconazole, clarithromycin, erythromycin,) or potent inducers of CYP3A4 and/or P-glycoprotein (e.g., rifampin, rifabutin).
Cannabidiol Drug Interactions
Closely monitor for an increase in sirolimus blood levels and for adverse reactions suggestive of sirolimus toxicity when cannabidiol and sirolimus are co-administered,. Consider a dose reduction of sirolimus as needed when coadministered with cannabidiol.
Specific Populations
Pregnancy
Potential for fetal harm based on animal studies and the drug's mechanism of action. Animal studies showed that the drug was embryotoxic and fetotoxic at subtherapeutic doses. Advise pregnant females of the potential risk to a fetus. (See Females and Males of Reproductive Potential under Cautions.)
The National Transplantation Pregnancy Registry (NTPR) is a pregnancy registry for pregnant women receiving immunosuppressants following any solid organ transplantation; the NTPR encourages reporting of all immunosuppressant exposures during pregnancy in transplant patients by telephone at 877-955-6877 or via their website: [Web].
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Not known whether the drug has any effects on the breastfed child or on milk production. Consider known benefits of breastfeeding along with mother's need for the drug and potential adverse effects on the breastfed infant.
Females and Males of Reproductive Potential
Potential for fetal harm if administered to pregnant females. Advise females of reproductive potential to use highly effective contraception prior to initiation, during, and for 12 weeks after completion of sirolimus treatment.
Based on findings in animals, male and female fertility may be compromised by treatment with sirolimus.
Pediatric Use
Safety and efficacy not established in children <13 years of age for prophylaxis of organ rejection in renal transplantation.
Safety and efficacy established in pediatric and adolescent renal transplant patients ≥13 years of age at low to moderate immunologic risk.
Safety and efficacy data in pediatric and adolescent renal transplant patients <18 years of age at high immunologic risk (i.e., history of ≥1 acute rejection episodes and/or presence of chronic allograft nephropathy) did not support chronic use because of higher incidence of lipid abnormalities and deterioration of renal function and lack of demonstrated therapeutic benefit compared with a calcineurin inhibitor-based regimen.
Safety and efficacy in pediatric patients <18 years of age not established for the treatment of lymphangioleiomyomatosis.
Geriatric Use
Studies did not include sufficient numbers of patients >65 years of age to determine whether geriatric patients respond differently than younger patients. Differences in responses between geriatric patients and younger patients not identified.
Hepatic Impairment
Prolonged elimination; adjustment of the maintenance dosage and therapeutic drug monitoring recommended in all patients with hepatic impairment.
Safety and efficacy of sirolimus as immunosuppressive therapy in liver transplant patients not established; such use notrecommended.
Common Adverse Effects
Renal transplantation (≥30%): peripheral edema, hypercholesterolemia, hypertriglyceridemia, hypertension, increased serum creatinine concentrations, constipation, abdominal pain, diarrhea, headache, fever, urinary tract infection, anemia, nausea, arthralgia, pain, and thrombocytopenia.
Lymphangioleiomyomatosis (≥20%): stomatitis, diarrhea, abdominal pain, nausea, nasopharyngitis, acne, chest pain, peripheral edema, upper respiratory tract infection, headache, dizziness, myalgia, and hypercholesterolemia.
Drug Interactions
Metabolized by CYP3A4; also a substrate for P-glycoprotein.
Drugs Affecting Hepatic Microsomal Enzymes
CYP3A4 inhibitors: Potential pharmacokinetic interaction (increased blood concentrations of sirolimus).
CYP3A4 inducers: Potential pharmacokinetic interaction (decreased blood concentrations of sirolimus).
Nephrotoxic Drugs
Possible increased risk of nephrotoxicity with concurrent use of nephrotoxic drugs (e.g., aminoglycosides, amphotericin B); use with caution.
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Acyclovir |
Pharmacokinetic interaction unlikely |
|
|
Anticonvulsants (carbamazepine, phenobarbital, phenytoin) |
Decreased blood sirolimus concentrations |
Use with caution |
|
Antifungals, azoles (fluconazole, itraconazole, ketoconazole, voriconazole) |
Increased bioavailability of sirolimus |
Use fluconazole with caution; adjust dosage of sirolimus and/or fluconazole if necessary Use of itraconazole, ketoconazole, and voriconazole not recommended; consider alternative antifungal therapy with less interaction potential |
|
Antilipemic agents |
Concurrent use of HMG-CoA reductase inhibitors and/or fibric acid derivatives appears to be well tolerated Clinically important pharmacokinetic interaction with atorvastatin unlikely |
Monitor for rhabdomyolysis and other adverse effects (e.g., hepatic toxicity) associated with antilipemic therapy |
|
Bromocriptine |
Possible increased blood sirolimus concentrations |
Use with caution |
|
Calcium-channel blocking agents (diltiazem, nicardipine, nifedipine, verapamil) |
Diltiazem: Increased bioavailability of sirolimus Nicardipine: Increased blood sirolimus concentrations Nifedipine: Pharmacokinetic interaction unlikely Verapamil: Increased bioavailability of sirolimus and verapamil |
Use with caution; adjust dosage of sirolimus and/or calcium-channel blocking agent as necessary Sirolimus dosage adjustment not required with concomitant use of nicardipine |
|
Cannabidiol |
Increase in sirolimus blood levels and adverse reactions suggestive of sirolimus toxicity |
Use with caution; adjust dosage of sirolimus as necessary |
|
Cimetidine |
Increased blood sirolimus concentrations |
Use with caution |
|
Cisapride |
Increased blood sirolimus concentrations |
Use with caution |
|
Clotrimazole |
Increased blood sirolimus concentrations |
Use with caution |
|
Contraceptives, oral |
Pharmacokinetic interaction unlikely |
|
|
Co-trimoxazole |
Pharmacokinetic interaction unlikely |
|
|
Cyclosporine |
Increased blood concentrations of sirolimus and cyclosporine Possible increased risk of calcineurin inhibitor-induced hemolytic uremic syndrome/thrombotic thrombocytopenic purpura/thrombotic microangiopathy |
Administer sirolimus 4 hours after modified cyclosporine oral solution or capsules |
|
Danazol |
Increased blood sirolimus concentrations |
Use with caution |
|
Digoxin |
Pharmacokinetic interaction unlikely |
|
|
Dronedarone |
Increased blood sirolimus concentrations; |
Manufacturer of dronedarone recommends monitoring sirolimus concentrations; adjust dosage if necessary Some clinicians suggest avoiding combined therapy; if cannot be avoided, they recommend reducing sirolimus dosage by 50–75% prior to initiating dronedarone and closely monitoring sirolimus concentrations, particularly during the titration phase |
|
Glyburide |
Hypoglycemic effect of glyburide not affected Clinically important pharmacokinetic interaction unlikely |
|
|
Grapefruit juice |
Increased bioavailability of sirolimus |
Avoid concomitant administration, do not use as diluent |
|
HIV protease inhibitors (e.g., indinavir, ritonavir) |
Increased blood sirolimus concentrations |
Use with caution |
|
Letermovir |
Increased blood sirolimus concentrations |
Use with caution |
|
Macrolide antibiotics (clarithromycin, erythromycin, troleandomycin) |
Increased blood sirolimus concentrations |
Concurrent use of clarithromycin or erythromycin and sirolimus not recommended; consider alternative anti-infective therapy with less interaction potential Use troleandomycin with caution; adjust dosage of sirolimus if necessary |
|
Metoclopramide |
Increased blood sirolimus concentrations |
Use with caution |
|
Prednisolone |
Pharmacokinetic interaction unlikely |
|
|
Rifabutin |
Decreased blood sirolimus concentrations |
Avoid concomitant use; consider alternative anti-infective therapy with less interaction potential |
|
Rifampin |
Decreased blood sirolimus concentrations |
Avoid concomitant use; consider alternative anti-infective therapy with less interaction potential |
|
Rifapentine |
Possible decreased blood sirolimus concentrations |
Use with caution; adjust dosage of sirolimus and/or rifapentine if necessary |
|
St. John’s wort |
Possible decreased sirolimus concentrations |
|
|
Tacrolimus |
Possible decreased exposure to tacrolimus Increased risk of hepatic artery thrombosis, graft loss, and death in de novo liver transplant recipients Possible increased risk of calcineurin inhibitor-induced hemolytic uremic syndrome/thrombotic thrombocytopenic purpura/thrombotic microangiopathy Increased risk of wound healing complications, impaired renal function, and insulin-dependent post-transplant diabetes mellitus in heart transplant recipients |
Concomitant use not recommended |
|
Vaccines |
Possible decreased response to vaccination |
Avoid use of live vaccines |
Sirolimus Pharmacokinetics
Absorption
Bioavailability
Rapidly but poorly absorbed from the GI tract. Following oral administration as solution, peak blood concentrations occur in approximately 1 hour in healthy individuals and in about 2 hours in renal transplant recipients. Systemic availability of oral solution is about 14%.
Sirolimus tablets are not bioequivalent to the oral solution; bioavailability of tablet is about 27% higher relative to the solution.
Food
Administration of sirolimus (as oral solution or tablets) with high-fat meal increases mean total exposure by 23–35% compared with fasting; effect of food on peak blood concentration was inconsistent depending on the dosage form evaluated.
Special Populations
In renal transplant patients >65 years of age, sirolimus trough concentrations were similar to those observed in adults 18–65 years of age.
Distribution
Extent
Extensively partitioned into formed blood elements (mean blood-to-plasma ratio of sirolimus is 36 in stable renal allograft recipients).
Distributed into milk in animals; not known whether sirolimus distributes into human milk or crosses the placenta.
Plasma Protein Binding
Approximately 92% (mainly albumin [97%]; also α1-acid glycoprotein and lipoproteins).
Elimination
Metabolism
Extensively metabolized in the intestinal wall and liver by CYP3A4; also a substrate for P-glycoprotein; 7 major metabolites.
Present in human whole blood principally as sirolimus; sirolimus contributes >90% of the immunosuppressive activity.
Elimination Route
Excreted mainly in feces (91%).
Half-life
Terminal elimination half-life: About 62 hours in stable renal transplant patients.
Special Populations
In patients with mild, moderate, and severe hepatic impairment (Child-Pugh class A, B, and C), AUC is increased by 43, 94, and 189%, respectively; as severity of hepatic impairment increased, steady increases in mean sirolimus elimination half-lives and decreases in mean sirolimus clearance normalized for body weight observed.
Stability
Storage
Oral
Tablets
Tight, light-resistant container at 20–25°C.
Solution
2–8°C for solution in bottles; protect from light. Discard bottle 1 month after opening. May store solution at room temperature (≤25°C) for up to 15 days. May store solution in the amber syringe provided by manufacturer for up to 24 hours at 2–8°C or room temperature (≤25°C). Use immediately after dilution.
If slight haze develops when solution in bottles is refrigerated, allow to stand at room temperature and shake gently until haze disappears.
Actions
-
Mechanism of action appears to be distinct from that of other immunosuppressants (e.g., tacrolimus, cyclosporine). Sirolimus inhibits activation of mammalian target of rapamycin (mTOR); unlike tacrolimus and cyclosporine, sirolimus does not block calcineurin pathway.
-
Inhibits T lymphocyte activation and proliferation that occurs in response to antigenic and cytokine (e.g., interleukin-2, interleukin-4, interleukin-15) stimulation. Also inhibits interleukin-2-dependent and independent proliferation of B-lymphocytes and the production of antibodies (e.g., immunoglobulins A, M, and G).
-
Potent mTOR inhibitor immunosuppressive agent. In animal models, about 27 times as potent as tacrolimus.
-
Lymphangioleiomyomatosis (LAM) is a progressive, cystic lung disease in women associated with inappropriate activation of mTOR signaling, which regulates cellular growth and lymphangiogenesis. Sirolimus inhibits the activated mTOR pathway and thus the proliferation of LAM cells.
Advice to Patients
-
Advise patients, their families, and their caregivers to read the manufacturer's medication guide and instructions for use.
-
Inform patients that sirolimus may increase risk of skin cancer. Advise patients to limit exposure to sunlight or other UV light by wearing protective clothing and sunglasses and using broad spectrum sunscreen with a high protection factor.
-
Advise females of childbearing age of the potential fetal risks and instruct such women to use highly effective contraception prior to initiation of sirolimus therapy, during therapy, and for 12 weeks after discontinuance of therapy.
-
Importance of females informing their clinician if they are breast-feeding or plan to breast-feed. Effects of breast-feeding during treatment with sirolimus are unknown, but there is potential for serious adverse effects.
-
Advise patients that sirolimus may impair fertility in males and females.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements.
-
Inform patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
1 mg/mL* |
Rapamune |
Wyeth |
|
Sirolimus Oral Solution |
||||
|
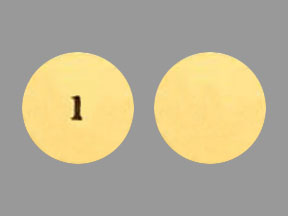
Tablets |
0.5 mg* |
Rapamune |
Wyeth |
|
|
Sirolimus Tablets |
||||
|
1 mg* |
Rapamune |
Wyeth |
||
|
Sirolimus Tablets |
||||
|
2 mg* |
Rapamune |
Wyeth |
||
|
Sirolimus Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Sirolimus vs Tacrolimus: How do they compare?
- Are Sirolimus and Rapamycin the same drug?
- What Is Sirolimus’s MOA (Mechanism of Action)?
More about sirolimus
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (8)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: mTOR inhibitors
- Breastfeeding
- En español