Oxsoralen-Ultra
Generic name: methoxsalen (oral) [ meth-OX-a-len ]
Brand names: 8-Mop, Oxsoralen-Ultra
Drug class: Psoralens
What is Oxsoralen-Ultra?
Oxsoralen-Ultra works by enhancing the body's sensitivity to ultraviolet light A (UVA).
Oxsoralen-Ultra is used in combination with UVA light therapy to treat severe psoriasis.
Oxsoralen-Ultra can cause harmful effects on your vision and on your skin (premature aging or skin cancer). Oxsoralen-Ultra is used only for severe psoriasis that has not improved with other treatments. You must remain under the care of a doctor while taking this medicine.
Oxsoralen-Ultra may also be used for purposes not listed in this medication guide.
Oxsoralen-Ultra side effects
Get emergency medical help if you have signs of an allergic reaction: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Oxsoralen-Ultra may cause serious side effects. Call your doctor at once if you have:
-
severe skin redness within 24 hours after UVA treatment;
-
swelling, severe itching, or severe skin discomfort;
-
skin redness and swelling with blisters;
-
worsening of your psoriasis;
-
a new skin lesion, or a mole that has changed in size or color; or
-
blurred vision, tunnel vision, eye pain or swelling, or seeing halos around lights.
Mild skin redness may occur and can last for 1 or 2 days. This is a normal side effect after UVA treatment and may not be a sign of severe sunburn. Ask your doctor if you have concerns about any redness or swelling.
Common side effects of Oxsoralen-Ultra may include:
-
itching, redness;
-
nausea;
-
feeling nervous; or
-
sleep problems (insomnia).
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Related/similar drugs
methotrexate, Humira, adalimumab, Stelara, Remicade, cyclosporine
Warnings
You should not use Oxsoralen-Ultra if you are sensitive to light, if you have lens damage in your eye, or if you have had skin cancer.
Oxsoralen-Ultra can cause harmful effects on your vision and on your skin. You must avoid natural sunlight for up to 48 hours after UVA treatment.
Oxsoralen-Ultra and 8-Mop are not equivalent medicines and may not have the same dosing schedule.
Before taking this medicine
You should not use Oxsoralen-Ultra if you are allergic to Oxsoralen-Ultra or similar medicines, or if you have:
-
lupus, porphyria, albinism, or other conditions that make you more sensitive to light;
-
a history of skin cancer (melanoma or squamous cell carcinoma); or
-
damage to the lenses of your eyes caused by surgery, injury, or genetic condition.
Before your UVA treatment: Do not expose your skin to sunlight for at least 24 hours before you take Oxsoralen-Ultra. Avoid applying sunscreen to areas of psoriasis that will be treated with UVA therapy.
You may need to have your eyes examined before you start taking Oxsoralen-Ultra.
To make sure Oxsoralen-Ultra is safe for you, tell your doctor if you have ever had:
-
liver or kidney disease;
-
cataracts;
-
extreme sensitivity to sunlight (if you sunburn easily); or
-
radiation or x-ray therapy, or treatment with arsenic trioxide (Trisenox).
It is not known whether Oxsoralen-Ultra taken orally will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant.
It may not be safe to breast-feed a baby while you are using this medicine. Ask your doctor about any risks.
How should I take Oxsoralen-Ultra?
You may need to have your eyes examined first.
Follow all directions on your prescription label. Use the medicine exactly as directed.
Oxsoralen-Ultra doses are based on weight. Tell your doctor if you gain or lose weight.
You will take Oxsoralen-Ultra a certain number of hours before you are scheduled to receive UVA treatment. Soft gelatin capsules (Oxsoralen-Ultra) are more easily absorbed than hard gelatin capsules (8-Mop). The timing of your dose will depend on the type of capsule you are taking.
You may need to keep taking Oxsoralen-Ultra for a short time after UVA treatment. Follow your doctor's dosing instructions very carefully.
Take this medicine with low-fat food or milk if it upsets your stomach.
If your doctor changes your brand, strength, or type of methoxsalen, your dose needs and UVA light therapy schedule may change. Oxsoralen-Ultra and 8-Mop are not equivalent medicines and may not have the same dosing schedule.
Oxsoralen-Ultra will make you more sensitive to sunlight, which can cause harmful effects on your vision and on your skin (premature aging or skin cancer).
For at least 8 hours after you take Oxsoralen-Ultra:
-
Avoid exposure to sunlight or tanning beds.
-
Even sunlight shining through clouds or through a glass window can expose you to harmful UV rays.
-
Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors or near a window.
-
Do not apply sunscreen to areas of active psoriasis that will be treated with UVA therapy.
For 24 to 48 hours after you receive UVA treatment:
-
You must protect your skin and eyes from natural sunlight (even sun shining through a window).
-
Do not expose your skin to any sunlight. Wear protective clothing including a hat and gloves. Use a sunscreen with a minimum SPF of 30, and apply it to all uncovered skin areas exposed to light.
-
Wear sunglasses for at least 24 hours after treatment.
-
For utmost protection, wear a pair of wraparound UVA-absorbing sunglasses, even while you are indoors near a window.
You may develop cataracts if you do not properly protect your eyes after Oxsoralen-Ultra and UVA treatment.
Follow your doctor's instructions about applying topical psoriasis medications or any moisturizing lotions after your Oxsoralen-Ultra and UVA treatment.
Check your skin regularly for signs of skin cancer, such as a small growth or nodule, a scaly or crusted lesion, a brownish spot or speckles, or a change in the size, color, or feel of a mole. You may need to check your skin for signs of cancer throughout the rest of your life.
Store Oxsoralen-Ultra at room temperature away from moisture, heat, and light.
What happens if I miss a dose?
Call your doctor for instructions if you did not take Oxsoralen-Ultra at the correct time before your scheduled UVA treatment. You may need to reschedule.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. You may be instructed to make yourself vomit and stay in a dark room for 24 hours. You will be extremely sensitive to light after an overdose.
What should I avoid while taking Oxsoralen-Ultra?
Avoid exposure to sunlight or artificial UV rays other than your scheduled light therapy treatments.
What other drugs will affect Oxsoralen-Ultra?
Tell your doctor about all your current medicines and any you start or stop using. Oxsoralen-Ultra can make your skin even more sensitive to sunlight if you also use certain other medicines, especially:
-
an antibiotic or a sulfa drug;
-
certain antimicrobial soaps;
-
a diuretic or "water pill";
-
coal tar applied to the skin or scalp--such as Neutrogena T/Gel, Psoriasin, Tegrin Medicated;
-
medicine to treat mental illness--fluphenazine, prochlorperazine, thioridazine, and others; or
-
a staining dye--such as methylene blue, toluidine blue, rose bengal, or methyl orange.
This list is not complete. Other drugs may interact with methoxsalen, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed in this medication guide.
More about Oxsoralen-Ultra (methoxsalen)
- Check interactions
- Compare alternatives
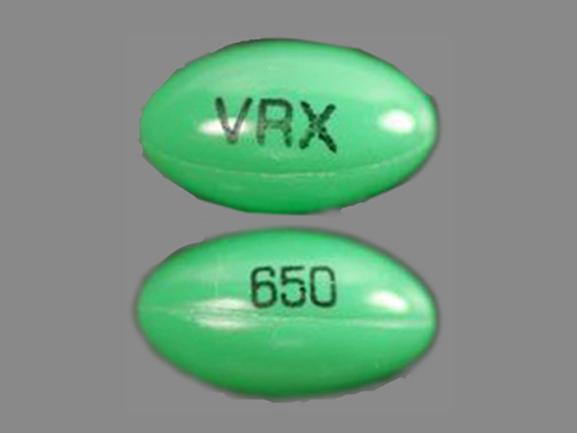
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Generic availability
- Drug class: psoralens
- Breastfeeding
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2024 Cerner Multum, Inc. Version: 5.01.