Topotecan (Monograph)
Brand name: Hycamtin
Drug class: Antineoplastic Agents
VA class: AN900
Chemical name: (S)-10-[(Dimethylamino)methyl]-4-ethyl-4,9-dihydroxy-1H-pyrano[3′,4′:6,7]indolizino[1,2-b]quinoline-3,14(4H,12H)-dione monohydrochloride
Molecular formula: C23H23N3O5•ClH
CAS number: 119413-54-6
Warning
- Experience of Supervising Clinician
-
Administer only under supervision of qualified clinicians experienced in use of cytotoxic therapy. Adequate diagnostic and treatment facilities should be readily available to manage complications.
- Myelosuppression
-
Severe myelosuppression (neutropenia) resulting in infection and death may occur. (See Hematologic Effects under Cautions.)
-
Do not administer to patients with baseline neutrophil counts <1500/mm3 and a platelet count <100,000/mm3 .
-
Monitor peripheral blood cell counts frequently.
Introduction
Antineoplastic agent; a semisynthetic derivative of camptothecin.
Uses for Topotecan
Ovarian Cancer
Treatment of advanced ovarian cancer in patients with disease that has recurred or progressed following therapy with platinum-based (i.e., cisplatin, carboplatin) regimens.
Small Cell Lung Cancer
Second-line therapy for treatment-sensitive small cell lung cancer (defined as disease initially responding to first-line chemotherapy with subsequent relapse no sooner than 60–90 days following completion of first-line therapy when topotecan is administered IV or at least 45 days following completion of first-line therapy when topotecan is administered orally).
Cervical Cancer
Used in combination with cisplatin for the treatment of stage IV-B, recurrent, or persistent cervical cancer not amenable to curative treatment with surgery and/or radiation therapy.
Related/similar drugs
methotrexate, Keytruda, carboplatin, pembrolizumab, fluorouracil, Avastin, cyclophosphamide
Topotecan Dosage and Administration
General
-
Consult specialized references for procedures for proper handling and disposal of antineoplastic drugs.
-
Individualize dosage based on body surface area and patient tolerance.
Administration
Administer orally or by IV infusion.
Oral Administration
Administer topotecan capsules orally, with or without food. (See Food under Pharmacokinetics).
Capsules should be swallowed whole; do not crush, chew, divide, or open.
IV Administration
Administer by IV infusion only.
Handle cautiously (by trained nonpregnant personnel); use protective equipment (e.g., vertical laminar flow hood, goggles, gloves, and protective gowns). Immediately treat accidental contact with the skin by copious lavage with soap and water; flush mucosa with copious amounts of water.
Reconstitution
Reconstitute vial containing 4 mg of topotecan with 4 mL of sterile water for injection to provide a solution containing 1 mg/mL.
Dilution
Must be diluted in 5% dextrose or 0.9% sodium chloride injection prior to IV administration.
Dilute calculated daily dose in a suitable volume (e.g., 50–250 mL) of 5% dextrose or 0.9% sodium chloride injection.
Lyophilized drug contains no preservatives; prepare solutions immediately before use.
Rate of Administration
Administer by IV infusion over a period of 30 minutes.
Dosage
Available as topotecan hydrochloride; dosage expressed in terms of topotecan.
Prior to administration of the initial course of therapy, patient must have a baseline neutrophil count ≥1500/mm3 and a platelet count ≥100,000/mm3.
Do not administer a subsequent course of therapy until recovery of patient's hematologic function (neutrophil count >1000/mm3, platelet count >100,000/mm3, and hemoglobin ≥9 g/dL [with transfusion if necessary]).
Adults
Ovarian Cancer
IV
1.5 mg/m2 daily for 5 consecutive days every 21 days.
A minimum of 4 courses of therapy is recommended in patients without progression of disease, provided intolerable toxicity does not develop. Median time to response averages 9–12 weeks; response may not be achieved if therapy is discontinued prematurely.
Small Cell Lung Cancer
Oral
2.3 mg/m2 once daily for 5 consecutive days every 21 days.
Round calculated daily dosage to the nearest 0.25 mg and prescribe the minimum number of 1-mg and 0.25-mg capsules; use the same number of capsules for each of the 5 days.
IV
1.5 mg/m2 daily for 5 consecutive days every 21 days.
A minimum of 4 courses of therapy is recommended in patients without progression of disease, provided intolerable toxicity does not develop. Median time to response averages 5–7 weeks; response may not be achieved if therapy is discontinued prematurely.
Cervical Cancer
IV
0.75 mg/m2 daily for 3 consecutive days (days 1, 2, and 3) every 21 days; administer cisplatin 50 mg/m2 by IV infusion on day 1 of each 21-day cycle (after the topotecan dose).
Dosage Modification for Toxicity
Ovarian Cancer
IVIf severe neutropenia occurs (i.e., neutrophil count <500/mm3), reduce dose in subsequent courses to 1.25 mg/m2; alternatively, administer granulocyte colony stimulation factor (G-CSF; filgrastim) 24 hours after the final dose of topotecan in the subsequent treatment course (i.e., beginning on day 6 of the 21-day treatment course).
If platelet count is <25,000/mm3, reduce dose in subsequent courses to 1.25 mg/m2.
Small Cell Lung Cancer
OralIf severe neutropenia (i.e., neutrophil count <500/mm3 associated with fever or infection or lasting for ≥7 days) or neutropenia (neutrophils 500–1000/mm3 lasting beyond day 21 of the treatment course) occurs, reduce dose in subsequent courses to 1.9 mg/m2 daily.
If platelet count is <25,000/mm3, reduce dose in subsequent courses to 1.9 mg/m2 daily.
If grade 3 or 4 diarrhea occurs, reduce dose in subsequent courses to 1.9 mg/m2 daily. If necessary, consider the same dose reduction to 1.9 mg/m2 daily for grade 2 diarrhea.
IVIf severe neutropenia occurs (i.e., neutrophil count <500/mm3), reduce dose in subsequent courses to 1.25 mg/m2; alternatively, administer granulocyte colony stimulation factor (G-CSF; filgrastim) 24 hours after the final dose of topotecan in the subsequent treatment course (i.e., beginning on day 6 of the 21-day treatment course).
If platelet count is <25,000/mm3, reduce dose in subsequent courses to 1.25 mg/m2.
Cervical Cancer
IVIf severe febrile neutropenia occurs (i.e., neutrophil count <1000/mm3 with a temperature of 38°C), reduce dose to 0.6 mg/m2 for subsequent courses. Alternatively, administer G-CSF 24 hours after the final dose of topotecan in the subsequent treatment course (i.e., beginning on day 4 of the 21-day treatment course). If febrile neutropenia still occurs with G-CSF, reduce topotecan dosage to 0.45 mg/m2 for subsequent courses.
If platelet count is <10,000/mm3, reduce dose in subsequent courses to 0.6 mg/m2.
Special Populations
Hepatic Impairment
No dosage adjustment required in patients with plasma bilirubin >1.5 but <10 mg/dL.
Renal Impairment
Ovarian Cancer
IV
Reduce dosage in patients with Clcr of 20–39 mL/minute to 0.75 mg/m2 daily for 5 consecutive days every 21 days.
Experience in patients with Clcr ≤19 mL/minute is too limited to make dosage recommendations.
Small Cell Lung Cancer
Oral
Reduce dosage in patients with Clcr of 30–49 mL/minute to 1.8 mg/m2daily for 5 consecutive days every 21 days.
Insufficient experience in patients with Clcr of <30 mL/minute to make dosage recommendations.
IV
Reduce dosage in patients with Clcr of 20–39 mL/minute to 0.75 mg/m2 daily for 5 consecutive days every 21 days.
Experience in patients with Clcr ≤19 mL/minute is too limited to make dosage recommendations.
Cervical Cancer
IV
Initiate treatment in combination with cisplatin only if SCr ≤1.5 mg/dL. In clinical trials, cisplatin was discontinued if SCr >1.5 mg/dL; insufficient data available regarding continuing topotecan therapy after cisplatin is discontinued.
Geriatric Patients
No dosage adjustments required except those related to renal impairment. (See Renal Impairment under Dosage and Administration.)
Cautions for Topotecan
Contraindications
-
Known or suspected pregnancy. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
-
Nursing women.
-
Severe bone marrow depression.
-
Known hypersensitivity to topotecan or any ingredient in the formulation.
Warnings/Precautions
Warnings
Hematologic Effects
Risk of dose-limiting and potentially fatal myelosuppression, manifested commonly as neutropenia, thrombocytopenia, and anemia. Pancytopenia reported. Myelosuppression occurs frequently, may be severe, and may require transfusions.
Neutrophil nadirs usually occur at day 12 and 15 with IV and oral administration, respectively. Platelet nadirs usually occur at day 15 with IV and oral administration. Median duration of neutropenia is 7 days with IV and oral administration and median duration of thrombocytopenia is 5 and 3 days with IV and oral administration, respectively. Median nadir for anemia occurs at day 15.
Careful hematologic monitoring required; perform peripheral blood cell counts prior to and at frequent intervals during therapy. Withhold subsequent courses of therapy until neutrophil count is >1000/mm3, platelet count is >100,000/mm3, and hemoglobin is ≥9 g/dL (with transfusion if necessary).
Neutropenic Colitis
Neutropenic colitis, a sequela of drug-induced neutropenia, has been reported and can be fatal.
Consider possibility of neutropenic colitis if patients present with fever, neutropenia, and abdominal pain.
Diarrhea
Diarrhea occurs commonly in patients receiving topotecan capsules; may be severe, life-threatening, and require hospitalization..
Diarrhea may occur at the same time as neutropenia and its sequelae. (See Neutropenic Colitis under Cautions.)
If diarrhea occurs, manage aggressively (e.g., antidiarrheal and anti-infective therapy, changes in fluid and diet requirements, hospitalization).
Other GI Effects
Nausea, vomiting, abdominal pain, constipation, intestinal obstruction, and stomatitis reported.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm; teratogenicity and embryolethality demonstrated in animals. Avoid pregnancy during therapy. If used during pregnancy or patient becomes pregnant, apprise of potential fetal hazard.
General Precautions
Local Effects
Extravasation may result in mild local effects (e.g., erythema, bruising).
Nervous System Effects
Possible asthenia or fatigue.
Specific Populations
Pregnancy
Category D. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Lactation
Distributed in high concentrations into milk in rats; not known whether topotecan is distributed into human milk. Discontinue nursing because of potential risk to nursing infants. (See Contraindications under Cautions.)
Pediatric Use
Safety and efficacy not established.
Geriatric Use
Oral administration: increased risk of diarrhea relative to younger patients.
IV administration: No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out.
Substantially eliminated by kidneys; assess renal function periodically and select dosage with caution since geriatric patients more likely to have decreased renal function.
Hepatic Impairment
Pharmacokinetics not substantially altered in patients with impaired hepatic function (i.e., plasma bilirubin >1.5 to <10 mg/dL).
Renal Impairment
Decreased clearance; increased risk of toxicity in patients with renal impairment. Dosage adjustments recommended depending on degree of renal impairment. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Neutropenia, leukopenia, thrombocytopenia, anemia, nausea, vomiting, diarrhea, constipation, abdominal pain, stomatitis, anorexia, fatigue, fever, pain, asthenia, alopecia, rash, dyspnea, cough, headache, infection/sepsis.
Drug Interactions
Does not inhibit CYP isoenzymes 1A2, 2A6, 2C8, 2C9, 2C19, 2D6, 2E, 3A, or 4A or dihydropyrimidine dehydrogenase in vitro.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antineoplastic agents (paclitaxel) |
Increased myelosuppression |
Dose reduction may be necessary (see Dosage Modification for Toxicity under Dosage and Administration) |
|
Antineoplastic agents, platinum (cisplatin, carboplatin) |
Possible sequence-dependent myelosuppression |
Lower doses of each drug required with administration of cisplatin on day 1 compared with day 5 of the topotecan dosing schedule |
|
G-CSF (filgrastim) |
Prolonged duration of neutropenia if administered concomitantly |
Initiate G-CSF 24 hours after completion of the last topotecan dose in a course of therapy (see Dosage under Dosage and Administration) |
|
P-glycoprotein inhibitors (e.g., cyclosporine A, ketoconazole, ritonavir, saquinavir) |
Insignificant increased topotecan exposure |
Avoid concomitant use If used concomitantly, closely monitor for adverse effects |
Topotecan Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed following oral administration, with peak plasma concentrations attained within 1–2 hours.
Bioavailability is approximately 40%.
Food
Extent of absorption following oral administration similar in fed and fasted states, however tmax delayed; capsules can be given without regard to food.
Distribution
Plasma Protein Binding
Approximately 35%.
Elimination
Metabolism
Principally undergoes reversible pH-dependent hydrolysis. Minor metabolic pathway in the liver to an N-demethylated metabolite.
Elimination Route
Following IV administration, excreted in urine (51%) and in feces (18%) mainly as total topotecan.
Following oral administration, excreted in urine (20%) and in feces (33%) mainly as total topotecan.
Half-life
Terminal elimination half-life following IV administration: 2–3 hours.
Terminal elimination half-life following oral administration: 3–6 hours.
Special Populations
In male patients, increased clearance.
In patients with renal impairment, clearance is decreased and half-life is 5 hours.
In patients with hepatic impairment, clearance is decreased; however, half-life is increased only slightly.
Stability
Storage
Oral
Capsules
20–25°C (may be exposed to 15–30°C); protect from light.
Parenteral
Powder for Injection
20–25°C; protect from light. Use immediately after reconstitution. Following dilution with infusion solution, use drug within 24 hours.
Compatibility
Parenteral
Solution CompatibilityHID
|
Compatible |
|
Dextrose 5% in water |
|
Sodium chloride 0.9% |
Drug Compatibility
|
Compatible |
|
Carboplatin |
|
Cimetidine HCl |
|
Cisplatin |
|
Cyclophosphamide |
|
Doxorubicin HCl |
|
Etoposide |
|
Gemcitabine HCl |
|
Granisetron HCl |
|
Ifosfamide |
|
Methylprednisolone sodium succinate |
|
Metoclopramide HCl |
|
Ondansetron HCl |
|
Oxaliplatin |
|
Paclitaxel |
|
Palonosetron HCl |
|
Prochlorperazine edisylate |
|
Vincristine sulfate |
|
Incompatible |
|
Dexamethasone sodium phosphate |
|
Fluorouracil |
|
Mitomycin |
|
Pemetrexed disodium |
|
Variable |
|
Ticarcillin disodium–clavulanate potassium |
Actions
-
A type I DNA topoisomerase inhibitor.
-
Exerts cytotoxic effects during the S-phase of DNA synthesis through an interaction with the DNA-DNA topoisomerase cleavable complex.
-
Stabilizes cleavable complex and prevents the topoisomerase from religating the single-strand breaks.
-
Interferes with the moving replication fork, inducing replication arrest and lethal double-stranded breaks in DNA. This DNA damage is not efficiently repaired and apparently leads to apoptosis (programmed cell death).
-
Importance of recognizing and reporting adverse effects including myelosuppressive effects and infectious complications.
-
Risk of weakness or fatigue; use caution when driving or operating machinery until effects on individual are known.
-
Importance of not chewing, crushing, dividing, or opening the capsule. Capsules must be swallowed whole.
-
Risk of potentially severe diarrhea with oral topotecan. Importance of contacting clinician if severe diarrhea occurs.
-
If vomiting occurs following a dose of oral topotecan, do not take a replacement dose.
-
Importance of women informing clinicians immediately if they are or plan to become pregnant or plan to breast-feed; necessity for clinicians to advise women to avoid pregnancy during therapy and advise pregnant women of risk to the fetus.
-
Importance of patients informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as concomitant illnesses.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
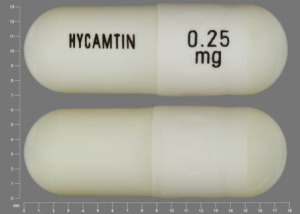
Oral |
Capsules |
0.25 mg (of topotecan) |
Hycamtin |
GlaxoSmithKline |
|
1 mg (of topotecan) |
Hycamtin |
GlaxoSmithKline |
||
|
Parenteral |
For injection, for IV infusion only |
4 mg (of topotecan) |
Hycamtin |
GlaxoSmithKline |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions April 1, 2009. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about topotecan
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1)
- Latest FDA alerts (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antineoplastics
- Breastfeeding
- En español