Tolvaptan (Monograph)
Brand name: Samsca
Drug class: Vasopressin Antagonists
ATC class: C03XA01
Chemical name: N-[4-[(7-chloro-2,3,4,5-tetrahydro-5-hydroxy-1H-1-benzazepin-1-yl)carbonyl]-3-methylphenyl]-2-methyl-benzamide
Molecular formula: C26H25ClN2O3
CAS number: 150683-30-0
Warning
Risk Evaluation and Mitigation Strategy (REMS):
FDA approved a REMS for tolvaptan to ensure that the benefits outweigh the risk. The REMS may apply to one or more preparations of tolvaptan and consists of the following: communication plan, elements to assure safe use, and implementation system. See https://www.accessdata.fda.gov/scripts/cder/rems/.
Warning
-
Initiate or reinitiate tolvaptan only in a hospital setting, where serum sodium concentrations and therapeutic response can be monitored closely.
-
Too rapid a correction of hyponatremia (e.g., increases in serum sodium concentration of >12 mEq/L over 24 hours) may cause osmotic demyelination syndrome, resulting in dysarthria, mutism, dysphagia, lethargy, affective changes, spastic quadriparesis, seizures, coma, or death.
-
Slower rates of correction may be advisable in susceptible patients, including those with severe malnutrition, alcoholism, or advanced liver disease. (See Overly Rapid Correction of Serum Sodium Concentration under Cautions.)
Introduction
Selective, nonpeptide antagonist of arginine vasopressin (antidiuretic hormone) V2 receptors; benzazepine derivative.
Uses for Tolvaptan
Euvolemic or Hypervolemic Hyponatremia
Treatment of clinically important euvolemic or hypervolemic hyponatremia (serum sodium concentration of <125 mEq/L or less marked hyponatremia that is symptomatic and has resisted correction with fluid restriction), including cases in patients with heart failure or SIADH.
Not indicated for the treatment of hypovolemic hyponatremia.
Do not use in patients who require urgent intervention to raise serum sodium concentrations to prevent or treat serious neurologic manifestations.
Use of tolvaptan to increase serum sodium concentrations has not been established to provide symptomatic benefit to patients.
Tolvaptan Dosage and Administration
General
-
Avoid fluid restriction during first 24 hours of therapy. Advise patients that they may continue drinking fluids in response to thirst.
-
Following discontinuance of drug, advise patients to resume fluid restriction and monitor patients for changes in serum sodium concentration and fluid status.
Administration
Initiate or reinitiate tolvaptan only in a hospital setting, where serum sodium concentrations and therapeutic response can be monitored closely; too rapid a correction of hyponatremia may cause serious neurologic sequelae (e.g., osmotic demyelination syndrome). (See Boxed Warning and see Overly Rapid Correction of Serum Sodium Concentration under Cautions.)
Oral Administration
Administer orally without regard to meals.
Dosage
Adults
Euvolemic or Hypervolemic Hyponatremia
Oral
Initially, 15 mg once daily; dosage may be increased at intervals of ≥24 hours to 30 mg once daily and subsequently up to 60 mg once daily as needed to achieve the desired serum sodium concentration.
Limit therapy to 30 days to minimize risk of hepatic injury. (See Hepatic Injury under Cautions.)
Frequently monitor serum electrolytes and fluid status during initiation and titration of therapy.
Discontinue or interrupt therapy if serum sodium concentrations increase too rapidly or manifestations of hypovolemia occur. (See Overly Rapid Correction of Serum Sodium Concentration and also Dehydration and Hypovolemia under Cautions.)
Prescribing Limits
Adults
Euvolemic or Hypervolemic Hyponatremia
Oral
Maximum: 60 mg once daily. Doses >60 mg do not further increase aquaresis or serum sodium concentrations.
Limit therapy to 30 days to minimize risk of hepatic injury. (See Hepatic Injury under Cautions.)
Special Populations
Dosage adjustment based on gender, race, or cardiac function not necessary.
Hepatic Impairment
Avoid use in patients with underlying liver disease, including cirrhosis. (See Hepatic Injury under Cautions.)
Renal Impairment
Dosage adjustment not necessary based on renal function; use not recommended in patients with Clcr <10 mL/minute. (See Renal Impairment under Cautions.)
Anuric patients not expected to benefit from therapy. (See Contraindications under Cautions.)
Geriatric Patients
Dosage adjustment not necessary. (See Geriatric Use under Cautions.)
Cautions for Tolvaptan
Contraindications
-
Patients requiring urgent intervention to acutely raise serum sodium concentrations; drug not studied in these patients.
-
Patients unable to sense or appropriately respond to thirst. Individuals unable to autoregulate fluid balance at substantially increased risk for overly rapid correction of serum sodium concentrations, hypernatremia, and hypovolemia. (See Overly Rapid Correction of Serum Sodium Concentration and see Dehydration and Hypovolemia, under Cautions.)
-
Hypovolemic hyponatremia. Risks associated with worsening hypovolemia, including complications such as hypotension and renal failure, outweigh possible benefits of therapy. (See Dehydration and Hypovolemia under Cautions.)
-
Concomitant use of potent CYP3A inhibitors (e.g., clarithromycin, indinavir, itraconazole, ketoconazole, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin). (See CYP3A Inhibitors under Interactions.)
-
Anuria. Anuric patients not expected to obtain clinical benefit from therapy.
Warnings/Precautions
Warnings
Overly Rapid Correction of Serum Sodium Concentration
Initiate or reinitiate tolvaptan only in a hospital setting, where serum sodium concentrations and therapeutic response can be monitored closely. (See Boxed Warning.)
Increases in serum sodium of >12 mEq/L over 24 hours may cause osmotic demyelination syndrome, resulting in dysarthria, mutism, dysphagia, lethargy, affective changes, spastic quadriparesis, seizures, coma, or death. Slower rates of correction may be advisable in susceptible patients, including those with severe malnutrition, alcoholism, or advanced liver disease. Patients with SIADH or very low baseline serum sodium concentrations may be at increased risk for too rapid a correction of serum sodium concentration.
Osmotic demyelination syndrome reported.
Monitor serum sodium concentrations and neurologic status, especially during initiation and following titration of therapy; if serum sodium concentrations increase too rapidly, discontinue or interrupt tolvaptan and consider administration of hypotonic fluid.
Avoid fluid restriction during the first 24 hours of therapy; may increase the risk of overly rapid correction of serum sodium concentration.
Other Warnings/Precautions
Hepatic Injury
May cause serious, potentially irreversible and fatal hepatic injury.
Increased incidence of ALT >3 times the ULN and 3 cases of serious hepatic injury (ALT >3 times the ULN with total bilirubin >2 times the ULN) reported during a 3-year placebo-controlled trial and its open-label extension in patients with autosomal dominant polycystic kidney disease† [off-label] receiving chronic tolvaptan therapy (up to 90 mg in the morning and 30 mg in the afternoon).
Hepatic abnormalities generally occurred during first 18 months of therapy and gradually improved following discontinuance. Serious hepatic injury occurred ≥3 months after treatment initiation, but ALT elevations observed during first 3 months of therapy.
Available data not adequate to exclude possibility of increased risk of irreversible and fatal hepatic injury in patients receiving tolvaptan (at lower dosages) for treatment of euvolemic or hypervolemic hyponatremia.
If symptoms suggestive of hepatic injury (e.g., fatigue, anorexia, upper right abdominal discomfort, dark urine, jaundice) occur, promptly discontinue therapy, perform liver function tests, institute appropriate treatment, and determine probable cause. Do not reinitiate therapy unless hepatic injury definitively established to be unrelated to the drug.
Limit duration of therapy to 30 days.
Avoid use in patients with underlying liver disease, including cirrhosis, because ability to recover from hepatic injury may be impaired.
Dehydration and Hypovolemia
Dehydration and hypovolemia may occur, especially in potentially volume-depleted patients receiving diuretics or those who are fluid restricted.
If clinically important signs or symptoms of hypovolemia occur, discontinue or interrupt tolvaptan and provide supportive care, including careful management of vital signs, fluid balance, and electrolytes.
Fluid restriction during therapy may increase risk of dehydration and hypovolemia. Patients should continue drinking fluids in response to thirst; use is contraindicated in patients unable to sense or appropriately respond to thirst and in those with hypovolemic hyponatremia. (See Contraindications under Cautions.)
Concomitant Use with Hypertonic Sodium Chloride
Concomitant use with hypertonic sodium chloride not recommended.
Hyperkalemia
Acute reduction of extracellular fluid volume may occur, resulting in increased serum potassium concentrations.
Monitor serum potassium concentrations after initiation of therapy in patients with a serum potassium concentration of >5 mEq/L and in those receiving drugs known to increase serum potassium concentrations (e.g., angiotensin II receptor antagonists, ACE inhibitors, potassium-sparing diuretics). (See Drugs Increasing Serum Potassium Concentration under Interactions.)
Hypernatremia
Hypernatremia reported.
Continue to monitor all patients, especially those who achieve normal serum sodium concentrations, to ensure concentrations remain within normal limits.
Management of hypernatremia may include dosage reduction or interruption of therapy in conjunction with modification of fluid intake or infusion to correct free-water deficit.
Specific Populations
Pregnancy
Category C.
Effect of drug on labor and delivery not known.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in children <18 years of age.
Geriatric Use
No substantial differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out. Dosage adjustment based on age not necessary.
Hepatic Impairment
Moderate or severe hepatic impairment does not appear to have clinically important effects on exposure to drug. However, avoid use in patients with underlying liver disease, including cirrhosis. (See Hepatic Injury under Cautions.)
Renal Impairment
Exposure and response to drug similar in individuals with Clcr of 10–79 mL/minute and in those with normal renal function. (See Absorption: Special Populations under Pharmacokinetics.)
No dosage adjustment necessary based on renal function; however, use not recommended in patients with Clcr <10 mL/minute. Not studied in clinical trials in patients with Clcr <10 mL/minute; unlikely to increase serum sodium concentrations in patients with very low levels of renal function.
Anuric patients not expected to benefit from therapy. (See Contraindications under Cautions.)
Common Adverse Effects
Thirst, dry mouth, pollakiuria or polyuria, asthenia, constipation, hyperglycemia, pyrexia, anorexia.
Drug Interactions
Mainly, if not exclusively, metabolized by CYP3A; weak inhibitor of CYP3A. Substrate and inhibitor of P-glycoprotein transport system.
Drugs Affecting Hepatic Microsomal Enzymes
Potent CYP3A inhibitors: Pharmacokinetic interaction (marked increase in exposure to tolvaptan). Insufficient experience available to determine dosage adjustment necessary to allow safe concomitant use; concomitant use is contraindicated. (See Contraindications under Cautions.)
Moderate CYP3A inhibitors: Effect on tolvaptan exposure not studied; substantial increase in exposure to tolvaptan expected. Avoid concomitant use.
CYP3A inducers: Potential pharmacokinetic interaction (decreased plasma tolvaptan concentrations) with concomitant use of potent CYP3A inducers. Avoid concomitant use with CYP3A inducers. If used concomitantly with CYP3A inducers, expected clinical effects of tolvaptan may not be observed at recommended dosage; monitor patient response and adjust dosage accordingly.
Drugs Affecting the P-glycoprotein Transport System
Inhibitors of the P-glycoprotein transport system: Potential pharmacokinetic interaction (increased tolvaptan concentrations); may require reduction of tolvaptan dosage based on clinical response.
Drugs Increasing Serum Potassium Concentration
Potential pharmacologic interaction (increased incidence of hyperkalemia); however, formal drug interaction studies not performed. Monitor serum potassium concentrations during concomitant use with drugs known to increase serum potassium concentrations. (See Hyperkalemia under Cautions.)
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Amiodarone |
No clinically important effects on pharmacokinetics of amiodarone or its active metabolite, desethylamiodarone; no apparent increase in tolvaptan concentrations |
|
|
Angiotensin II receptor antagonists |
Possible increased risk of hyperkalemia |
Monitor serum potassium concentrations |
|
ACE inhibitors |
Possible increased risk of hyperkalemia |
Monitor serum potassium concentrations |
|
Anticonvulsants (e.g., barbiturates, carbamazepine, phenytoin) |
Decreased plasma tolvaptan concentrations (effects similar to those of rifampin) expected |
Avoid concomitant use If used with barbiturates, carbamazepine, or phenytoin, expected clinical effects of tolvaptan may not be observed at recommended dosage; monitor patient response and adjust dosage accordingly |
|
Antimycobacterials (e.g., rifabutin, rifampin, rifapentine) |
Decreased plasma tolvaptan concentrations Rifampin: Reduced plasma tolvaptan concentrations by 85% |
Avoid concomitant use If used with rifabutin, rifampin, or rifapentine, expected clinical effects of tolvaptan may not be observed at recommended dosage; monitor patient response and adjust dosage accordingly |
|
Aprepitant |
Substantial increase in exposure to tolvaptan expected |
Avoid concomitant use |
|
Clarithromycin |
Marked increase in tolvaptan exposure (effects similar to those of ketoconazole) expected |
Concomitant use contraindicated; insufficient experience available to determine dosage adjustment necessary to allow safe concomitant use |
|
Cyclosporine |
Possible increased tolvaptan concentrations |
Reduction of tolvaptan dosage may be required based on clinical response |
|
Desmopressin |
Possible interference with V2 receptor agonist activity of desmopressin (e.g., failure to produce expected increases in von Willebrand factor antigen and factor VIII activity reported in patient with mild von Willebrand disease) |
Concomitant use not recommended |
|
Digoxin |
Increased AUC and peak concentration of digoxin; no clinically important effects on exposure to tolvaptan |
|
|
Diltiazem |
Substantial increase in exposure to tolvaptan expected |
Avoid concomitant use |
|
Diuretics, potassium-sparing |
Possible increased risk of hyperkalemia |
Monitor serum potassium concentrations |
|
Erythromycin |
Substantial increase in exposure to tolvaptan expected |
Avoid concomitant use |
|
Fluconazole |
Substantial increase in exposure to tolvaptan expected |
Avoid concomitant use |
|
Furosemide |
No apparent clinically important effects on furosemide pharmacokinetics or tolvaptan exposure 24-hour urine output is greater with tolvaptan than with furosemide, but is not substantially greater with combined tolvaptan/furosemide use than with tolvaptan alone |
|
|
Grapefruit juice |
Increased exposure to tolvaptan |
|
|
Hydrochlorothiazide |
No apparent clinically important effects on hydrochlorothiazide pharmacokinetics or tolvaptan exposure 24-hour urine output is greater with tolvaptan than with hydrochlorothiazide, but is not substantially greater with combined tolvaptan/hydrochlorothiazide use than with tolvaptan alone |
|
|
Indinavir |
Marked increase in tolvaptan exposure (effects similar to those of ketoconazole) expected |
Concomitant use contraindicated; insufficient experience available to determine dosage adjustment necessary to allow safe concomitant use |
|
Itraconazole |
Marked increase in tolvaptan exposure (effects similar to those of ketoconazole) expected |
Concomitant use contraindicated; insufficient experience available to determine dosage adjustment necessary to allow safe concomitant use |
|
Ketoconazole |
Ketoconazole 200 mg daily: Fivefold increase in tolvaptan exposure observed Ketoconazole 400 mg daily: Even greater increase in tolvaptan exposure expected |
Concomitant use contraindicated; insufficient experience available to determine dosage adjustment necessary to allow safe concomitant use |
|
Lovastatin |
Increased exposure to lovastatin and its active metabolite, lovastatin-β hydroxyacid; not considered clinically important No clinically important effects on exposure to tolvaptan |
|
|
Nefazodone |
Marked increase in tolvaptan exposure (effects similar to those of ketoconazole) expected |
Concomitant use contraindicated; insufficient experience available to determine dosage adjustment necessary to allow safe concomitant use |
|
Nelfinavir |
Marked increase in tolvaptan exposure (effects similar to those of ketoconazole) expected |
Concomitant use contraindicated; insufficient experience available to determine dosage adjustment necessary to allow safe concomitant use |
|
Ritonavir |
Marked increase in tolvaptan exposure (effects similar to those of ketoconazole) expected |
Concomitant use contraindicated; insufficient experience available to determine dosage adjustment necessary to allow safe concomitant use |
|
St. John’s wort (Hypericum perforatum) |
Decreased plasma tolvaptan concentrations (effects similar to those of rifampin) expected |
Avoid concomitant use If used concomitantly, expected clinical effects of tolvaptan may not be observed at recommended dosage; monitor patient response and adjust dosage accordingly |
|
Saquinavir |
Marked increase in tolvaptan exposure (effects similar to those of ketoconazole) expected |
Concomitant use contraindicated; insufficient experience available to determine dosage adjustment necessary to allow safe concomitant use |
|
Telithromycin |
Marked increase in tolvaptan exposure (effects similar to those of ketoconazole) expected |
Concomitant use contraindicated; insufficient experience available to determine dosage adjustment necessary to allow safe concomitant use |
|
Verapamil |
Substantial increase in exposure to tolvaptan expected |
Avoid concomitant use |
|
Warfarin |
No apparent clinically important effects on pharmacokinetics of warfarin |
Tolvaptan Pharmacokinetics
Absorption
Bioavailability
Absolute bioavailability unknown; at least 40% of dose absorbed as tolvaptan or metabolites.
Peak plasma concentrations observed 2–4 hours following a dose.
AUC increases proportionally with dose; however, at doses ≥60 mg, peak plasma concentrations increase less than proportionally with dose.
Onset
Onset of aquaretic and sodium-increasing effects occurs within 2–4 hours following a single 60-mg dose in healthy individuals.
Peak effects (increases in serum sodium concentrations and urinary excretion rate of about 6 mEq/L and 9 mL/minute, respectively) observed 4–8 hours following a 60-mg dose.
Duration
About 60% of peak effect on serum sodium concentrations sustained at 24 hours following a dose; however, urinary excretion rate no longer elevated at this time.
Food
Food does not affect bioavailability.
Special Populations
Increasing age does not affect plasma tolvaptan concentrations.
Exposure to drug similar in individuals with Clcr of 10–79 mL/minute and in those with normal renal function. In patients with Clcr of 10–124 mL/minute, AUC and peak plasma concentration increased less than twofold in patients with severe renal impairment compared with controls; peak increase in serum sodium concentration was 5–6 mEq/L regardless of renal function, but onset and offset of effect on sodium concentration slower in patients with severe renal impairment. (See Renal Impairment under Cautions.)
Moderate or severe hepatic impairment does not have clinically important effects on exposure to drug.
Patients with CHF do not have a clinically important increase in exposure to drug.
Distribution
Extent
Distributed into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
99%.
Special Populations
Moderate or severe hepatic impairment increases volume of distribution; not considered clinically important.
CHF increases volume of distribution; not considered clinically important.
Elimination
Metabolism
Mainly, if not exclusively, metabolized in the liver by CYP3A. Substrate of the P-glycoprotein transport system. Metabolites have little or no V2-receptor antagonist activity.
Elimination Route
Following administration of radiolabeled tolvaptan, approximately 40 and 59% of radioactivity recovered in urine and feces, respectively; <1% of tolvaptan dose is excreted unchanged in urine, about 19% is excreted unchanged in feces, and about 80% is metabolized. Tolvaptan eliminated entirely (about 99%) by nonrenal mechanisms.
Half-life
Terminal-phase half-life is approximately 12 hours.
Special Populations
In patients with hyponatremia of any origin, clearance of drug is reduced.
Moderate or severe hepatic impairment decreases clearance; not considered clinically important.
CHF decreases clearance; not considered clinically important.
Stability
Storage
Oral
Tablets
25°C (may be exposed to 15–30°C).
Actions
-
Selective arginine vasopressin (antidiuretic hormone) V2 receptor antagonist.
-
Affinity for V2 receptors 29 times that for V1A receptors.
-
Does not appear to have any affinity for V1B receptors.
-
Antagonizes effects of vasopressin at V2 receptors of distal nephron, resulting in increased free water clearance, decreased urine osmolality, and increased serum sodium concentrations.
-
Urinary sodium and potassium excretion and plasma potassium concentrations not substantially altered; plasma concentrations of endogenous arginine vasopressin may increase.
-
Does not appear to have a clinically important effect on the QTc interval.
Advice to Patients
-
Importance of reviewing the medication guide with every patient. Importance of instructing patients to read the medication guide before initiating therapy and each time the prescription is refilled.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements, as well as any concomitant illnesses. Importance of informing clinicians if receiving drugs that are moderate or potent inhibitors of CYP3A or inhibitors of the P-glycoprotein transport system (see Interactions).
-
Potential for too rapid an increase in serum sodium concentration, which may result in serious neurologic sequelae. Importance of informing clinicians if any signs or symptoms suggestive of osmotic demyelination syndrome (e.g., difficulty speaking or swallowing, drowsiness, confusion, mood changes, weakness or involuntary movements in the extremities, seizures) occur. Importance of patients not stopping or restarting tolvaptan therapy on their own initiative.
-
Potential for hepatic injury, including life-threatening hepatic failure. Importance of not taking tolvaptan for >30 days and of informing clinicians if any signs or symptoms suggestive of hepatic injury (e.g., loss of appetite, nausea, vomiting, fever, feeling unwell, unusual tiredness, pruritus, jaundice, unusual darkening of urine, upper right abdominal pain or discomfort) occur.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Necessity of advising women to avoid breast-feeding during tolvaptan therapy.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
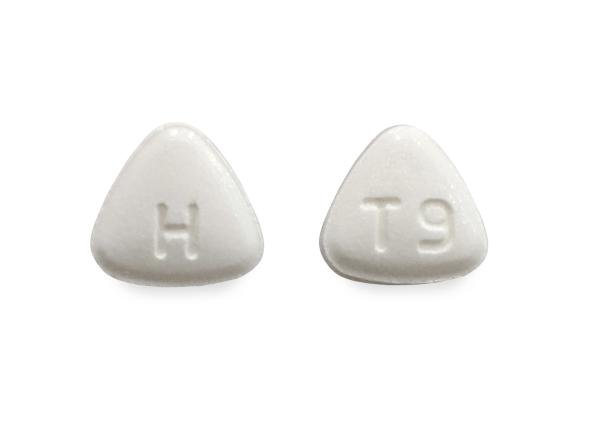
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
15 mg |
Samsca |
Otsuka |
|
30 mg |
Samsca |
Otsuka |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions May 21, 2018. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
More about tolvaptan
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: vasopressin antagonists
- En español