Tivozanib (Monograph)
Brand name: Fotivda
Drug class: Antineoplastic Agents
- Kinase Inhibitors
- Receptor Tyrosine Kinase Inhibitors
- Tyrosine Kinase Inhibitors
- VEGF Receptor Inhibitors
- VEGFR Inhibitors
- Vascular Endothelial Growth Factor Receptor Inhibitors
Chemical name: 1-[2-chloro-4-(6,7-dimethoxyquinolin-4-yl)oxyphenyl]-3-(5-methyl-1,2-oxazol-3-yl)urea;hydrate;hydrochloride
Molecular formula: C22H19ClN4O5•HCl•H2O
CAS number: 682745-41-1
Introduction
Antineoplastic agent; inhibitor of multiple kinases including vascular endothelial growth factor receptors (VEGFRs), stem cell factor receptor (c-kit), and platelet-derived growth factor receptor (PDGFR) β.
Uses for Tivozanib
Renal Cell Carcinoma (RCC)
Treatment of relapsed or refractory advanced RCC in adults who have received two or more prior systemic therapies.
Tivozanib Dosage and Administration
General
Pretreatment Screening
-
Blood pressure must be controlled prior to initiation of therapy.
-
Urinalysis to screen for proteinuria.
-
Thyroid function panel.
-
Verify pregnancy status of females of reproductive potential.
Patient Monitoring
-
Monitor blood pressure 2 weeks after initiation of therapy and then at least monthly thereafter.
-
Periodically monitor for signs or symptoms of cardiac failure.
-
Closely monitor patients who are at risk for or who have a history of cardiac ischemic or thromboembolic events (e.g., MI, stroke, arterial or venous thromboembolic events) for adverse cardiovascular effects.
-
Closely monitor patients who are at risk for or who have a history of hemorrhagic events for bleeding.
-
Periodically monitor for proteinuria (i.e., urinalysis).
-
Periodically monitor thyroid function.
Other General Considerations
-
Withhold therapy for ≥24 days prior to elective surgery. Do not administer for ≥2 weeks following major surgery and until adequate wound healing has occurred.
Administration
Oral Administration
Administer once daily without regard to food. Swallow capsules whole with a glass of water; do not open capsules.
If a dose is missed, take the dose at the next scheduled time. Do not take two doses at the same time.
Dosage
Dosage of tivozanib hydrochloride is expressed in terms of tivozanib.
Adults
RCC
Oral
1.34 mg once daily for 21 days on treatment followed by a 7-day rest period of each 28-day cycle. Continue therapy until disease progression or unacceptable toxicity occurs.
Dosage Modification for Toxicity
If adverse effects occur during tivozanib therapy, temporary interruption of therapy, dosage reduction, and/or permanent discontinuance of the drug may be necessary (see Table 1). If dosage modification is required, the dosage of tivozanib should be reduced to 0.89 mg for 21 days followed by a 7-day rest period (in 28-day cycles).
GI adverse effects (i.e., diarrhea, nausea, vomiting) should be managed with appropriate treatment prior to tivozanib dosage reduction or treatment interruption.
|
Adverse Reaction and Severity |
Modification |
|---|---|
|
Hypertension |
|
|
Grade 3 (despite optimal antihypertensive therapy) |
Withhold therapy; when hypertension improves to grade 2 or less, resume at reduced dosage |
|
Grade 4 |
Permanently discontinue therapy |
|
Cardiac Failure |
|
|
Grade 3 |
Withhold therapy; when toxicity resolves or improves to grade 0 or 1, resume at a reduced dosage or discontinue therapy depending on severity and persistence of the toxicity |
|
Grade 4 |
Permanently discontinue therapy |
|
Arterial Thromboembolic Event |
|
|
Any grade |
Permanently discontinue therapy |
|
Venous Thromboembolic Event |
|
|
Severe or life-threatening |
Permanently discontinue therapy |
|
Hemorrhagic Events |
|
|
Grade 3 or 4 |
Permanently discontinue therapy |
|
Proteinuria |
|
|
≥2 g proteinuria per 24 hours |
Withhold therapy; when proteinuria improves to ≤2 g per 24 hours, resume at a reduced dosage |
|
Nephrotic syndrome |
Permanently discontinue therapy |
|
Reversible Posterior Leukoencephalopathy Syndrome (RPLS) |
|
|
Any grade |
Permanently discontinue therapy |
|
Other Adverse Effects |
|
|
Grade 2 or 3 (persistent or intolerable) |
Withhold therapy; when toxicity resolves or improves to grade 0 or 1, resume at a reduced dosage |
|
Grade 4 |
Permanently discontinue therapy |
Special Populations
Hepatic Impairment
Moderate hepatic impairment (total bilirubin concentration >1.5–3 times the upper limit of normal [ULN] with any AST concentration): Reduce dosage to 0.89 mg orally once daily for 21 days followed by a 7-day rest period (in 28-day cycles).
Mild hepatic impairment (total bilirubin concentration ≤ULN with AST >ULN or total bilirubin >1–1.5 times ULN with any AST concentration): No dosage adjustment necessary.
Renal Impairment
The manufacturer makes no specific dosage recommendations.
Geriatric Patients
The manufacturer makes no specific dosage recommendations.
Related/similar drugs
Keytruda, Avastin, pembrolizumab, bevacizumab, nivolumab, Afinitor
Cautions for Tivozanib
Contraindications
-
None.
Warnings/Precautions
Cardiovascular Effects
Adverse cardiovascular effects (i.e., hypertension, cardiac failure, cardiac ischemic events) reported.
Assess and adequately control BP prior to initiating tivozanib therapy, 2 weeks after initiation of therapy, and then at least monthly thereafter. If hypertension occurs, initiate anti-hypertensive therapy as appropriate. If adverse cardiovascular effects occur, temporary interruption of therapy, dosage reduction, or discontinuation of therapy may be necessary.
Closely monitor patients who are at risk for cardiac ischemic events such as myocardial infarction or stroke (including those with a history of such events) for cardiac ischemic events during therapy.
Hypertension or Hypertensive Crisis
Hypertension occurs frequently. Median time to onset of hypertension is 2 weeks. Hypertensive crisis also reported. Safety in patients with a systolic blood pressure >150 mm Hg or diastolic blood pressure >100 mm Hg not studied.
Overdosage of tivozanib can cause severe hypertension and hypertensive crisis that may result in death. There is no specific treatment or antidote for overdosage of tivozanib. If overdosage is suspected, temporarily withhold therapy and closely monitor for hypertension and hypertensive crisis and other potential adverse reactions. Promptly manage signs or symptoms of hypertension and provide other supportive care as clinically indicated.
Cardiac Failure
Serious or fatal cardiac failure reported. Safety in patients with a history of symptomatic cardiac failure within 6 months of treatment initiation not studied.
Cardiac Ischemic Events
Serious or fatal cardiac ischemic events reported. Safety in patients with a history of myocardial infarction or unstable angina within 6 months of treatment initiation not studied.
Thromboembolic Events
Serious or fatal arterial and venous thromboembolic events reported. Safety in patients with a history of arterial thromboembolic event within 6 months of treatment initiation not studied.
Closely monitor patients who are at risk for arterial or venous thromboembolism (including those with a history of such events) during therapy with the drug. If an arterial thromboembolic event occurs, permanently discontinue therapy. If a severe or life-threatening venous thromboembolic event occurs, permanently discontinue therapy.
Hemorrhagic Events
Serious or fatal hemorrhagic events reported. Safety in patients with a history of significant bleeding within 6 months of treatment initiation not studied.
Closely monitor patients who are at risk for hemorrhagic events (including those with a history of hemorrhagic events) during therapy with the drug. If a severe or life-threatening hemorrhagic event occurs, permanently discontinue therapy.
Proteinuria
Proteinuria, sometimes resulting in acute kidney injury, reported. Acute kidney injury may occur either concurrently with proteinuria or later during the course of treatment.
Monitor for proteinuria prior to initiation of and periodically during therapy. Depending on the severity of proteinuria, temporary interruption of therapy, dosage reduction, or discontinuation of therapy may be necessary. Permanently discontinue therapy if nephrotic syndrome develops.
Thyroid Dysfunction
Thyroid dysfunction (hypothyroidism or hyperthyroidism) reported.
Assess thyroid function prior to initiation of and periodically during therapy. If hypothyroidism or hyperthyroidism occurs, initiate appropriate treatment to maintain a euthyroid state. Thyroid function tests must be within normal values prior to initiation of therapy.
Wound Healing Complications
VEGFR inhibitors may impair wound healing. Safety of resuming tivozanib treatment following resolution of wound healing complications not studied.
Withhold tivozanib at least 24 days prior to elective surgery. Following major surgery, do not resume tivozanib therapy for at least 2 weeks and until adequate wound healing occurs.
Reversible Posterior Leukoencephalopathy Syndrome (RPLS)
RPLS may occur.
Consider possible RPLS in patients presenting with seizures, headache, visual disturbances, confusion, or altered mental function. Magnetic resonance imaging (MRI) is necessary to confirm diagnosis. Permanently discontinue tivozanib in patients who develop RPLS.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm.
Avoid pregnancy during therapy. Verify pregnancy status prior to initiation of tivozanib in females of reproductive potential. Females of reproductive potential and men who are partners of such females should use an effective method of contraception during therapy and for one month after the last dose.
Sensitivity Reactions to Tartrazine
Contains tartrazine (FD&C Yellow No. 5), which can cause allergic reactions, including bronchial asthma, in certain susceptible patients, especially those who are sensitive to aspirin.
Specific Populations
Pregnancy
May cause fetal harm.
Avoid pregnancy during therapy. Verify pregnancy status in females of reproductive potential prior to initiation of therapy.
Lactation
Not known whether tivozanib is distributed into human milk or if the drug has any effect on milk production or the nursing infant. Women should not breast-feed while receiving the drug and for 1 month after the drug is discontinued.
Females and Males of Reproductive Potential
May impair fertility in females and males of reproductive potential.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Geriatric Use
No clinically important differences in efficacy were observed between geriatric patients and younger adults.
Hepatic Impairment
Mild hepatic impairment (total bilirubin concentration ≤ULN with AST concentration >ULN or total bilirubin >1–1.5 times ULN with any AST concentration) did not substantially affect pharmacokinetics of tivozanib; no dosage adjustment necessary.
Moderate hepatic impairment (total bilirubin concentration >1.5–3 times ULN with any AST concentration) increased AUC of tivozanib compared to individuals with normal hepatic function; reduce dosage of tivozanib to 0.89 mg orally once daily for 21 days on treatment followed by a 7-day rest period (in 28-day cycles).
Pharmacokinetics not studied in patients with severe hepatic impairment (total bilirubin concentration >3–10 times the ULN with any AST).
Renal Impairment
Mild to severe renal impairment (creatinine clearance of 15–89 mL/minute) did not appear to substantially affect pharmacokinetics of tivozanib; no dosage adjustment is necessary.
Pharmacokinetics not studied in patients with end-stage renal disease.
Common Adverse Effects
The most common (≥20%) adverse reactions were fatigue, hypertension, diarrhea, decreased appetite, nausea, dysphonia, hypothyroidism, cough, and stomatitis.
The most common grade 3 or 4 laboratory abnormalities (≥5%) were sodium decreased, lipase increased, lymphocytes decreased, and phosphate decreased.
Drug Interactions
Metabolized primarily by CYP3A4. Does not inhibit CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6 or 3A4 or uridine diphosphate-glucuronosyltransferase (UGT) enzymes at clinically relevant concentrations. Does not induce CYP isoenzymes 1A, 2B6, 2C9, 2C19, or 3A at clinically relevant concentrations.
Tivozanib inhibits breast cancer resistance protein (BCRP). Does not inhibit P-glycoprotein (P-gp), organic cation transporter (OCT) 1, OCT2, organic anion transporter (OAT)1, OAT3, organic anion transporting polypeptide (OATP) 1B1, OATP1B3, bile salt export pump (BSEP), multidrug and toxin extrusion (MATE)1, or MATE2-K.
Drugs Affecting or Affected by Hepatic Microsomal Enzymes
Strong CYP3A inducers: May result in decreased tivozanib plasma concentrations and reduced anti-tumor activity. Avoid concomitant use.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Ketoconazole |
No clinically significant effect on tivozanib pharmacokinetics. |
|
|
Rifampin |
Decreased AUC of tivozanib by 52%. |
Avoid concomitant use. |
Tivozanib Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentration and systemic exposure to tivozanib are dose-proportional over the dosage range of 0.89–1.78 mg once daily.
Steady state achieved in approximately 14 days; median time to peak plasma concentrations is 10 hours (range: 3–24 hours).
Food
No clinically significant differences in peak plasma concentration or systemic exposure of tivozanib following concomitant administration with a high-fat meal.
Distribution
Extent
Not known whether tivozanib distributed into breast milk.
Plasma Protein Binding
≥99% bound to plasma proteins; binding is independent of tivozanib concentration.
Elimination
Metabolism
Metabolized primarily by CYP3A4.
Elimination Route
Eliminated primarily in feces (79%; 26% as unchanged drug) and urine (12%).
Half-life
111 hours.
Stability
Storage
Oral
Capsules
20–25°C (excursions permitted between 15–30°C).
Actions
-
Inhibits the phosphorylation of VEGFR-1, VEGFR-2, and VEGFR-3 and inhibits other kinases such as c-kit and PDGFR β.
-
Inhibits angiogenesis, vascular permeability, and tumor growth of various tumor cell types (including human renal cell carcinoma) in mice and rats bearing tumor xenografts.
Advice to Patients
-
Advise the patient to read the FDA-approved patient labeling.
-
Inform patients that hypertension or hypertensive crisis may occur during tivozanib hydrochloride treatment. Advise patients to undergo routine blood pressure monitoring and to contact their healthcare provider if blood pressure is elevated. Advise patients to immediately contact their healthcare provider if they experience signs or symptoms of hypertension.
-
Advise patients to immediately contact their healthcare provider if they develop symptoms of cardiac failure.
-
Inform patients that arterial thromboembolic events (including fatal outcomes) may occur during tivozanib hydrochloride treatment. Advise patients to immediately contact their healthcare provider if new onset of chest discomfort, sudden weakness, or another event suggestive of a thrombotic event occurs.
-
Advise patients to immediately contact their healthcare provider if they develop symptoms of dyspnea or localized limb edema.
-
Advise patients to immediately contact their healthcare provider if they develop symptoms of dyspnea or localized limb edema.
-
Instruct patients to contact their healthcare provider to seek immediate medical attention for signs or symptoms of unusual bleeding or hemorrhage.
-
Inform patients that tivozanib hydrochloride may impair wound healing. Advise patients that temporary interruption of tivozanib hydrochloride is recommended prior to elective surgery. Advise patients to contact their healthcare provider before any planned surgeries, including dental surgery.
-
Inform patients that RPLS may occur during tivozanib hydrochloride treatment. Advise patients to immediately contact their healthcare provider in the event of seizures, headaches, visual disturbances, confusion or difficulty thinking.
-
Instruct patients to contact their healthcare provider immediately if they inadvertently take too much tivozanib hydrochloride.
-
Advise females of reproductive potential of the potential risk to a fetus. Advise patients to inform their healthcare provider of a known or suspected pregnancy.
-
Advise females of reproductive potential to use effective contraception during treatment with tivozanib hydrochloride and for one month after the last dose.
-
Advise male patients with female partners of reproductive potential to use effective contraception during treatment with tivozanib hydrochloride and for one month after the last dose.
-
Advise women not to breastfeed during treatment with tivozanib hydrochloride and for one month after the last dose.
-
Advise males and females of reproductive potential that tivozanib hydrochloride can impair fertility.
-
Tivozanib hydrochloride 0.89 mg (of tivozanib) capsule contains FD&C Yellow No. 5 (tartrazine) as an imprint ink which may cause allergic-type reactions (including bronchial asthma) in certain susceptible patients. Although the overall incidence of FD&C Yellow No. 5 (tartrazine) sensitivity in the general population is low, it is frequently seen in patients who also have aspirin hypersensitivity.
-
Advise patients that other adverse reactions with tivozanib hydrochloride treatment may include diarrhea, vomiting, dysphonia (hoarseness of voice), fatigue, asthenia and stomatitis (sores in the mouth), and cough.
-
Instruct patient if a dose of tivozanib hydrochloride is missed, the next dose should be taken at the regularly scheduled time. Do not take two doses in the same day.
-
Advise patients to inform their healthcare provider of all concomitant medications, vitamins, or dietary and herbal supplements.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Tivozanib hydrochloride can only be obtained through designated specialty pharmacies and distributors. Contact manufacturer for specific ordering and availability information.
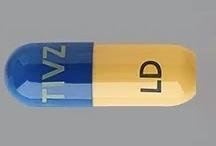
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsule |
0.89 mg (of tivozanib) |
Fotivda |
Aveo Pharmaceuticals |
|
1.34 mg (of tivozanib) |
Fotivda |
Aveo Pharmaceuticals |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions March 30, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about tivozanib
- Check interactions
- Compare alternatives
- Side effects
- Dosage information
- During pregnancy
- Drug class: VEGF/VEGFR inhibitors
- En español