Amantadine (Antiviral) (Monograph)
Drug class: Adamantanes
VA class: AM800
CAS number: 665-66-7
Introduction
Amantadine hydrochloride, an adamantane derivative, is a synthetic antiviral agent that is active against influenza A virus.
Uses for Amantadine (Antiviral)
Amantadine hydrochloride has been used for the symptomatic treatment and prophylaxis of signs and symptoms of infection caused by susceptible influenza A viruses.
For information on the use of amantadine in the treatment of parkinsonian syndrome and drug-induced extrapyramidal reactions, see Amantadine Hydrochloride 28:36.04.
Treatment of Seasonal Influenza A Virus Infections
Amantadine has been used for the treatment of uncomplicated respiratory tract illness caused by susceptible influenza A viruses in adults, adolescents, and children 1 year of age or older.
Beginning in the 2005–2006 influenza season, most influenza A (H3N2) strains circulating in the US were resistant to adamantanes (amantadine, rimantadine), and resistance to amantadine and rimantadine among seasonal influenza A (H3N2) isolates has remained high during subsequent influenza seasons. In addition, the influenza A (H1N1)pdm09 virus, previously referred to as the novel 2009 influenza A (H1N1) virus or swine-origin influenza A (H1N1) virus, that has circulated during recent influenza seasons is resistant to amantadine and rimantadine. Amantadine and rimantadine have little or no activity against influenza B.
The US Centers for Disease Control and Prevention (CDC) and other experts recommend that adamantanes (amantadine, rimantadine) not be used for the treatment of seasonal influenza in the US until susceptibility to these antiviral agents has been reestablished in circulating influenza A viruses.
Viral surveillance data available from local and state health departments and the CDC should be considered when selecting an antiviral for treatment of seasonal influenza. Strains of circulating influenza viruses and the antiviral susceptibility of these strains constantly evolve.
The CDC issues recommendations concerning the use of antiviral agents for the treatment of influenza, and these recommendations are updated as needed during each influenza season. Information regarding influenza surveillance and updated recommendations for the treatment of seasonal influenza are available from the CDC at [Web].
Clinical Experience
When amantadine has been used in otherwise healthy adults and children for symptomatic treatment of uncomplicated seasonal influenza caused by susceptible influenza A virus and administered within 24–48 hours after the onset of symptoms, the drug has decreased viral shedding and reduced the degree and duration of fever, headache, and respiratory symptoms with a more rapid return to routine daily activities and improvement in airway function. It is not known whether amantadine is effective for the symptomatic treatment of these infections in patients whose symptoms have been present for more than 48 hours since most controlled studies evaluating efficacy of the drug only included patients whose symptoms had been present for 48 hours or less.
While amantadine and rimantadine generally are comparably effective in the treatment of influenza A infection caused by susceptible strains, some evidence suggests that symptomatic improvement during the initial 24 hours of therapy with usual dosages of amantadine may be somewhat faster than that with rimantadine, probably because of pharmacokinetic differences between the drugs. In addition, although adverse effects of the drugs are similar, rimantadine may be associated with less frequent and/or severe nervous system effects.
There have been no well-controlled studies to date to determine the efficacy of amantadine treatment in preventing serious complications of influenza A virus infection (e.g., bacterial or viral pneumonia or exacerbation of chronic diseases). Most studies evaluating efficacy of amantadine for the treatment of influenza A infections have been performed in otherwise healthy adults and children with uncomplicated influenza; data are limited and inconclusive concerning efficacy of amantadine for treatment of influenza in individuals at high risk for serious influenza-related complications.
Prevention of Seasonal Influenza A Virus Infections
Amantadine has been used for prophylaxis against influenza infection caused by susceptible influenza A viruses in adults, adolescents, and children 1 year of age or older.
Annual vaccination with seasonal influenza virus vaccine, as recommended by the US Public Health Service Advisory Committee on Immunization Practices (ACIP), is the primary means of preventing seasonal influenza and its severe complications. Prophylaxis with an appropriate antiviral agent active against circulating influenza strains is considered an adjunct to vaccination for the control and prevention of influenza in certain individuals.
The CDC and other experts recommend that adamantanes (amantadine, rimantadine) not be used for prevention of influenza in the US until susceptibility to these antiviral agents has been reestablished in circulating influenza A viruses.
Viral surveillance data available from local and state health departments and the CDC should be considered when selecting an antiviral for the prophylaxis of influenza. The most appropriate antiviral for prevention of influenza is selected based on information regarding the likelihood that the influenza strain is susceptible and the known adverse effects of the drug. Strains of circulating influenza viruses and the antiviral susceptibility of these strains constantly evolve.
The CDC issues recommendations concerning the use of antiviral agents for prophylaxis of influenza, and these recommendations are updated as needed during each influenza season. Information regarding influenza surveillance and updated recommendations for prevention of seasonal influenza are available from CDC at [Web].
Clinical Experience
Results of numerous studies indicate that amantadine is about 60–90% effective in preventing influenza caused by susceptible strains of influenza A. Clinical studies indicate that amantadine is as effective as rimantadine or influenza vaccination in preventing influenza A illness. The protective effect of amantadine or rimantadine and influenza vaccination may be additive. In contrast to results of studies evaluating efficacy when antiviral prophylaxis is given for a season or part of a season, results of studies evaluating antiviral prophylaxis with amantadine or rimantadine after a known exposure have not been consistent. While postexposure prophylaxis with amantadine or rimantadine provided protection in families when the index case did not receive antiviral therapy, the drugs did not provide protection from influenza A infection in household contacts when amantadine or rimantadine was used to treat the index case, presumably because of spread of resistant virus within the household.
Avian Influenza A Virus Infections
Adamantane derivatives (amantadine, rimantadine) have been recommended as alternatives for the treatment or prophylaxis of avian influenza A virus infections† [off-label] in certain situations.
The CDC and World Health Organization (WHO) recommend use of a neuraminidase inhibitor (oseltamivir, zanamivir) for the treatment or prophylaxis of avian influenza A infections. If neuraminidase inhibitors are unavailable, use of amantadine or rimantadine might be considered an alternative if local surveillance data indicate that the strain is known or likely to be susceptible. Avian influenza A (H5N1) and avian influenza A (H7N9) generally have been resistant to the adamantane derivatives.
Related/similar drugs
Ingrezza, diphenhydramine, Benadryl, Tamiflu, ropinirole, oseltamivir, pramipexole
Amantadine (Antiviral) Dosage and Administration
Administration
Amantadine hydrochloride is administered orally.
Adverse effects (e.g., CNS effects) may be minimized if the daily dosage is given in 2 equally divided doses. It has been suggested that if insomnia occurs, the last daily dose should be taken several hours before retiring.
Amantadine hydrochloride is commercially available as tablets or liquid-filled capsules containing 100 mg of the drug and as an oral solution containing 50 mg/5 mL.
Dosage
A reduced dosage of amantadine hydrochloride is recommended in geriatric adults 65 years of age or older and in patients with renal impairment. The usual dosage of amantadine hydrochloride also may need to be reduced in patients with congestive heart failure, peripheral edema, or orthostatic hypotension.
Adult Dosage
Treatment of Seasonal Influenza A Virus Infections
For the treatment of uncomplicated respiratory tract illness caused by susceptible influenza A viruses, the usual dosage of amantadine hydrochloride for adults younger than 65 years of age with normal renal function is 200 mg daily. This dosage can be given as a single daily dose or as 100 mg twice daily. The drug should be initiated as soon as possible, preferably within 24–48 hours after the onset of symptoms, and continued for 24–48 hours after symptoms disappear.
Prevention of Seasonal Influenza A Virus Infections
For prophylaxis of influenza caused by susceptible influenza A viruses, the usual dosage of amantadine hydrochloride for adults younger than 65 years of age with normal renal function is 200 mg daily. This dosage can be given as a single daily dose or as 100 mg twice daily.
Some clinicians suggest that a dosage of 100 mg daily can be used as an alternative regimen for the prophylaxis of influenza A infection. Although limited evidence suggests that a 100-mg daily dosage may be effective for prophylaxis in healthy adults who are not at risk for influenza-related complications and is associated with fewer adverse effects, the relative efficacy of 100- versus 200-mg daily dosages for prophylaxis of influenza virus A infection has not been determined. The manufacturer states that the 100-mg daily dosage is recommended for individuals who have CNS or other toxicities while receiving the 200-mg daily dosage.
Amantadine prophylaxis should be continued for at least 10 days following a known exposure. If used as an adjunct to influenza vaccination, the drug usually is administered for 2–4 weeks after the vaccine is given to provide prophylaxis until a protective antibody response develops. (See Drug Interactions: Influenza Virus Vaccines.)
Geriatric Dosage
Treatment or Prevention of Seasonal Influenza A Virus Infections
The usual dosage of amantadine hydrochloride for the treatment or prophylaxis of influenza infection caused by susceptible influenza A viruses in geriatric adults 65 years of age or older without recognized renal disease is 100 mg once daily.
Since renal function normally declines with age and amantadine-induced adverse effects have been reported more frequently in geriatric patients, some clinicians state that 100 mg daily should be the maximum dosage of amantadine hydrochloride for adults 65 years of age or older, and that dosage may need to be further reduced in some geriatric patients.
Pediatric Dosage
Treatment or Prevention of Seasonal Influenza A Virus Infections
The dosage of amantadine hydrochloride recommended by the manufacturer for the treatment or prophylaxis of uncomplicated influenza caused by susceptible influenza A viruses in children 9–12 years of age is 100 mg twice daily. The American Academy of Pediatrics (AAP) states that children 10 years of age or older should receive a dosage of 100 mg twice daily if they weigh 40 kg or more or a dosage of 5 mg/kg daily given in 2 divided doses if they weigh less than 40 kg. While the manufacturer states that a dosage of 100 mg once daily has not been evaluated in children and there are no data demonstrating whether this dosage is as effective or safer than the 200 mg daily dosage in this age group, the AAP suggests that a dosage of 100 mg daily is an acceptable alternative dosage for prophylaxis of influenza A illness in children who weigh more than 20 kg.
For children 1–9 years of age, the manufacturer recommends that amantadine hydrochloride be given in a dosage of 4.4–8.8 mg/kg daily (up to 150 mg daily) for the treatment or prophylaxis of influenza caused by susceptible influenza A. The AAP recommends that children 1–9 years of age receive 5 mg/kg (up to 150 mg) daily given in 2 divided doses.
Dosage in Renal Impairment
When amantadine hydrochloride is used in patients with renal impairment, reduced dosage is recommended in those with creatinine clearances of 50 mL/minute or less.
The manufacturers recommends that patients with creatinine clearances of 30–50 mL/minute per 1.73 m2 receive 200 mg of amantadine hydrochloride on the first day, followed by 100 mg once daily thereafter and those with creatinine clearances of 15–29 mL/minute per 1.73 m2 receive 200 mg on the first day, followed by 100 mg once every other day thereafter. The manufacturers recommend that patients with creatinine clearances less than 15 mL/minute per 1.73 m2 and hemodialysis patients receive 200 mg of amantadine every 7 days.
Because dosage adjustment based on creatinine clearance may provide only an approximation of the optimal dosage of amantadine hydrochloride for a given patient, such patients should be observed carefully so that adverse reactions can be recognized promptly and either the dose can be reduced further or the drug can be discontinued as necessary. Hemodialysis contributes minimally to clearance of amantadine.
Cautions for Amantadine (Antiviral)
Amantadine hydrochloride generally is well tolerated, although serious adverse effects have been reported rarely. The incidence of adverse effects associated with amantadine therapy appears to be dose related. The adverse effects reported most frequently with amantadine are similar to those observed with rimantadine and include adverse CNS and GI effects; however, amantadine is associated with more frequent and/or more severe nervous system effects than rimantadine, including in geriatric adults.
Adverse effects associated with amantadine usually are mild and are reversible upon discontinuance of the drug. In some patients, adverse effects subside after the first week of therapy with the drug.
Nervous System Effects
Dizziness (lightheadedness), insomnia, nervousness, anxiety, and impaired concentration are among the most frequent adverse effects of amantadine and have been reported in up to 5–10% of individuals receiving the usual dosage of the drug (200 mg daily). However, limited data suggest that the incidence of adverse CNS effects may be lower in adults receiving a lower dosage of the drug. These adverse effects are usually mild, but may be more disturbing for geriatric patients than for younger patients.
Adverse CNS effects are more common with usual dosages of amantadine than usual dosages of rimantadine, probably in part because of differences in pharmacokinetics of the drugs In a 6-week study of daily 200-mg prophylactic doses of amantadine or rimantadine in healthy adults, about 13 or 6% of patients receiving the respective drug discontinued therapy because of adverse CNS effects versus about 4% of those receiving placebo.
Irritability, depression, ataxia, confusion, somnolence, abnormal dreams, agitation, fatigue, headache, and hallucinations have been reported in 1–5% and psychosis, abnormal thinking, amnesia, hyperkinesia, euphoria, weakness, and slurred speech have been reported in 1% or less of patients receiving amantadine. In addition, forgetfulness, a sense of drunkenness or detachment, drowsiness, coma, stupor, delirium, hypokinesia, hypertonia, delusions, aggressive behavior, paranoid reaction, manic reaction, involuntary muscle contractions, gait abnormalities, paresthesia, EEG changes, tremor, and, rarely, lingual facial dyskinesia or seizures have been reported.
Patients at Risk for CNS Effects
Patients with a history of seizure disorders may be at risk of an increased frequency of seizures during amantadine therapy. The more serious CNS effects (e.g., marked behavioral changes, delirium, agitation, hallucinations, seizures) of amantadine or rimantadine have been associated with high plasma concentrations of the drugs and have been observed most often among patients with renal impairment, seizure disorders, or certain psychiatric disorders and among geriatric patients who received prophylactic 200-mg doses daily. Clinical studies and experience indicate that lower dosages of amantadine in at-risk patients reduces the incidence and severity of these serious adverse effects.
Suicide Risk
Suicide attempts (resulting in death in some patients) have been reported rarely in patients receiving amantadine, many of whom received short courses of the drug for influenza treatment of prophylaxis. The manufacturer states that the incidence and pathophysiology of these suicide attempts are not known. Suicide ideation or attempts have been reported in patients with or without a prior history of psychiatric disorders. Amantadine can exacerbate mental status in patients with a history of psychiatric disorders or substance abuse. Patients with suicidal tendencies may exhibit abnormal mental states including disorientation, confusion, depression, personality changes, agitation, aggressive behavior, hallucinations, paranoia, other psychotic reactions, somnolence, or insomnia.
Because of the possibility of serious adverse effects, amantadine should be administered with caution to patients receiving drugs with CNS activity and in those in whom potential risks outweigh benefits of therapy with the drug. Since intentional overdosage with amantadine has been reported in some patients, the least amount of drug feasible should be prescribed.
Neuroleptic Malignant Syndrome
Possible neuroleptic malignant syndrome (NMS) has been reported in patients receiving amantadine and was associated with dosage reduction or withdrawal of the drug. NMS is potentially fatal and requires immediate initiation of intensive symptomatic and supportive care. Patients should be observed closely when the dosage of amantadine is reduced or the drug is discontinued; this precaution is especially important in patients receiving concomitant therapy with an antipsychotic agent. .
Livedo Reticularis
Livedo reticularis is a frequent adverse effect in patients receiving amantadine for the treatment of parkinsonian syndrome, and the possibility should be considered in patients receiving the drug for prolonged periods in the prevention of influenza A. Livedo reticularis occurs mainly in the legs and diminishes when the legs are elevated.
Livedo reticularis has been reported in 1–5% of patients, generally appears within 1 month to 1 year following initiation of amantadine therapy, and subsides within a few weeks to several months after discontinuance of the drug. In one study, livedo reticularis tended to fade or change into brown spots with prolonged amantadine therapy. It has been suggested that, in many instances, this adverse effect is actually an accentuation of a preexisting, minor livedo reticularis and may result from abnormal capillary permeability associated with peripheral vasoconstriction accompanied by lowered skin temperature and decreased peripheral blood flow, and/or amantadine's depletion of catecholamines in peripheral nerve endings.
Peripheral edema may precede or accompany livedo reticularis and may require dosage reduction or discontinuance of amantadine. The edema does not appear to be associated with an increase in total body water or sodium retention; it may result from increased vascular permeability in cutaneous tissues.
GI Effects
Nausea is one of the most frequent adverse effects of amantadine and has been reported in 5–10% of patients receiving the usual dosage of the drug. Anorexia, constipation, diarrhea, and dry mouth have been reported in 1–5% and vomiting has been reported in up to 1% of patients receiving amantadine. Dysphagia also has been reported.
Cardiovascular Effects
Orthostatic hypotension and peripheral edema have been reported in 1–5% and congestive heart failure and hypertension in up to 1% of patients receiving amantadine. Cardiac arrest, arrhythmias including malignant arrhythmias, and tachycardia have occurred in patients receiving amantadine.
Ocular Effects
Visual disturbance (e.g., punctate subepithelial or other corneal opacity), corneal edema, decreased visual acuity, ocular photosensitivity, or optic nerve palsy have been reported in up to 1% of patients receiving amantadine. Keratitis or mydriasis has occurred in patients receiving the drug. One patient experienced a sudden loss of visual acuity in both eyes, which gradually returned to normal several weeks after amantadine was discontinued.
Melanoma
Epidemiologic studies indicate that patients with parkinsonian syndrome have a twofold to sixfold higher risk of developing melanoma than the general population. It is unclear whether this increased risk is due to parkinsonian syndrome or other factors (e.g., drugs used to treat Parkinson's disease).
Patients receiving amantadine for any indication should be monitored for melanomas frequently and on a regular basis. Ideally, periodic skin examinations should be performed by appropriately qualified individuals (e.g., dermatologists).
Impulse Control and Compulsive Behaviors
Postmarketing reports suggest that patients receiving drugs that increase central dopaminergic tone and generally are used for the treatment of parkinsonian syndrome, including amantadine, can experience intense urges (e.g., urge to gamble, increased sexual urges, intense urge to spend money uncontrollably, other intense urges) and may be unable to control these urges. These urges stopped in some cases when dosage was reduced or the drug discontinued.
Because patients may not recognize these behaviors as abnormal, clinicians should ask patients and/or their caregivers whether new or increased gambling urges, sexual urges, uncontrolled spending, or other urges have developed during amantadine treatment and should advise them of the importance of reporting such urges. If a patient develops such urges while receiving amantadine, consideration should be given to reducing the dosage or discontinuing the drug.
Sensitivity and Dermatologic Effects
Allergic reactions, including anaphylactic reaction, rash, eczematoid dermatitis, photosensitization, pruritus, and diaphoresis, have occurred rarely in amantadine-treated patients.
Hematologic Effects
Hematologic effects reported in less than 0.1% of patients receiving amantadine include leukopenia, neutropenia, and leukocytosis.
Genitourinary Effects
Urinary retention and decreased libido have occurred in up to 1% of patients receiving amantadine.
Respiratory Effects
Dyspnea has been reported in up to 1% of amantadine-treated patients. Adverse respiratory effects reported rarely in amantadine-treated patients include acute respiratory failure, pulmonary edema, and tachypnea.
Other Adverse Effects
Fever or dry nose has occurred in patients receiving amantadine. Increased concentrations of creatine kinase (CK, creatine phosphokinase, CPK), BUN, serum creatinine, alkaline phosphatase, lactate dehydrogenase (LDH), bilirubin, γ-glutamyltransferase (GGT, γ-glutamyltranspeptidase, GGTP), ALT (SGPT), and AST (SGOT) have occurred in patients receiving amantadine.
Precautions and Contraindications
Amantadine is contraindicated in patients with known hypersensitivity to adamantine or any ingredient in the formulation.
Patients with a history of epilepsy or other seizure disorders should be observed closely for possible increased seizure activity during amantadine therapy.
Amantadine should be administered with caution in patients with liver disease or a history of recurrent eczematoid dermatitis, uncontrolled psychosis or severe psychoneurosis, and in those receiving drugs with CNS activity. Because of possible CNS effects or visual disturbances, patients receiving amantadine should be warned that the drug may impair their ability to perform hazardous activities requiring mental alertness or physical coordination such as operating machinery or driving a motor vehicle.
Because amantadine may cause mydriasis, the drug should not be used in patients with untreated angle-closure glaucoma.
Because possible neuroleptic malignant syndrome was reported in patients receiving amantadine and was associated with a dosage reduction or withdrawal of the drug, patients, especially those receiving antipsychotic agents, should be observed closely when the dosage of amantadine is reduced or the drug is discontinued.
Because viral surveillance data indicate that the majority of seasonal influenza A (H3N2) and influenza A (H1N1)pdm09 viruses circulating during recent influenza seasons have been resistant to adamantanes (amantadine, rimantadine), the US Centers for Disease Control and Prevention (CDC) and other experts state that amantadine and rimantadine should not be used for the treatment or prevention of influenza in the US until susceptibility to these antiviral agents has been reestablished in circulating influenza A viruses.
Serious bacterial infections may begin with influenza-like symptoms or may coexist with or occur as complications of influenza. There is no evidence that amantadine prevents such complications.
Deaths due to drug accumulation (overdosage) have been reported in patients with renal impairment who received amantadine in dosages that were higher than recommended for their degree of renal impairment. Amantadine should be used with caution and dosage of the drug adjusted as needed in patients with renal impairment, congestive heart failure, peripheral edema, or orthostatic hypotension. Dosage of the drug should be reduced in geriatric patients 65 years of age or older. (See Dosage and Administration: Dosage in Renal Impairment.)
Pediatric Precautions
Safety and efficacy of amantadine have not been established in neonates or children younger than 1 year of age.
Geriatric Precautions
Geriatric adults may have decreased renal function and because individuals with renal impairment may be at increased risk of amantadine-induced toxicity, the dosage of amantadine hydrochloride for adults in this age group should not exceed 100 mg daily. This dosage may need to be reduced further in some geriatric patients. (See Adult Dosage in Dosage and Administration: Dosage.)
Mutagenicity and Carcinogenicity
Amantadine was not mutagenic in the Ames microbial test using Salmonella typhimurium or a mammalian mutagen assay using Chinese hamster ovary cells when the tests were performed with or without metabolic activation. In addition, there was no evidence of chromosome damage in an in vitro test using freshly derived and stimulated human peripheral blood lymphocytes (with or without metabolic activation) or an in vivo mouse bone marrow micronucleus test (140–550 mg/kg; estimated human equivalent dosage of 11.7–45.8 mg/kg based on body surface area conversion).
Long-term animal studies have not been performed to evaluate the carcinogenic potential of amantadine.
Pregnancy, Fertility, and Lactation
Pregnancy
There are no adequate and well-controlled studies using amantadine in pregnant women, and the drug should be used during pregnancy only when the potential benefits outweigh the possible risks to the fetus.
Amantadine hydrochloride has been reported to be embryotoxic/teratogenic in rats when administered in dosages of 50 and 100 mg/kg daily (1.5 and 3 times, respectively, the maximum recommended human dosage on a mg/m2 basis), but not when administered in a dosage of 37 mg/kg daily (the maximum recommended human dosage on a mg/m2 basis). One woman with a movement disorder similar to parkinsonian syndrome who may have been treated with amantadine hydrochloride (100 mg daily) during the first trimester of pregnancy delivered a child with a complex cardiovascular lesion (single ventricle and pulmonary atresia) which may have been caused by the drug. Fallot and tibial hemimelia (normal karyotype) were reported in an infant exposed to oral amantadine hydrochloride during the first trimester of pregnancy (100 mg daily for 7 days during week 6 and 7 of gestation).
Fertility
In a rat reproduction study involving 3 litters, fertility was slightly impaired when amantadine hydrochloride was administered to both males and females in a dosage of 32 mg/kg daily (the maximum recommended human dosage on a mg/m2 basis). Fertility was not affected when the drug was given in a dosage of 10 mg/kg daily (0.3 times the maximum recommended human dosage on a mg/m2 basis); intermediate doses were not tested.
In one instance, failure was reported during human in vitro fertilization (IVF) when the sperm donor ingested amantadine 2 weeks before and during the IVF cycle.
Lactation
Amantadine should not be used in nursing women. The drug is distributed into human milk.
Drug Interactions
Drugs with Anticholinergic Activity
Administration of amantadine in patients receiving drugs with anticholinergic activity may result in increased adverse anticholinergic and CNS effects. When amantadine is administered to patients already near the limit of tolerance for anticholinergic agents, atropinism with nocturnal confusion and hallucinations may gradually develop. It has been suggested that the dosage of the anticholinergic agent be reduced prior to the initiation of amantadine therapy or that the dose of either drug be reduced if atropine-like adverse effects appear.
While concomitant administration of amantadine and thioridazine has been reported to worsen tremor in geriatric patients with parkinsonian syndrome, it is not known whether a similar effect would occur with other phenothiazines.
Alcohol
Because of the potential for CNS effects (e.g., dizziness, confusion, lightheadedness, orthostatic hypotension), excess use of alcohol should be avoided in patients receiving amantadine.
Antihistamines
Concomitant use of amantadine and antihistamines that affect the CNS (e.g., those exhibiting anticholinergic activity) may increase the incidence of adverse CNS reactions.
Antipsychotic Agents
Because of the risk of neuroleptic malignant syndrome (NMS), patients receiving amantadine and an antipsychotic agent should be observed closely when amantadine dosage is reduced or the drug is discontinued. (See Neuroleptic Malignant Syndrome under Cautions: Nervous System Effects.)
CNS Stimulants
To avoid the possibility of additive CNS stimulant effects, amantadine should be administered with caution to patients receiving CNS stimulants.
Co-trimoxazole
Toxic delirium has occurred following initiation of co-trimoxazole in at least one patient who had been stabilized on amantadine; rapid resolution occurred following discontinuance of the drugs.
Hydrochlorothiazide
Concomitant use of amantadine hydrochloride (100 mg 3 times daily) and a fixed-combination preparation containing triamterene and hydrochlorothiazide (co-triamterzide) in a 61-year-old man with parkinsonian syndrome resulted in increased plasma concentrations of amantadine; however, it is not known which component of the combination preparation may have been responsible for the interaction or whether related drugs would produce a similar effect.
Influenza Virus Vaccines
Amantadine hydrochloride does not interfere with the antibody response to influenza virus vaccine inactivated (IIV) and the vaccine may be administered concomitantly with or at any time before or after amantadine.
Safety and efficacy of concomitant use of influenza vaccine live intranasal (LAIV) and amantadine have not been studied. Because influenza antiviral agents reduce replication of influenza viruses and may inhibit the vaccine virus, LAIV should not be administered until at least 48 hours after amantadine is discontinued and amantadine should not be administered until at least 2 weeks after administration of LAIV, unless medically indicated. If amantadine is administered within 2 weeks after LAIV, the US Public Health Service Advisory Committee on Immunization Practices (ACIP) recommends that the LAIV dose be repeated 48 hours or more after the last dose of the antiviral agent. Alternatively, individuals who received amantadine 2 days before to 14 days after LAIV may be revaccinated with either IIV or influenza vaccine recombinant (RIV).
Quinidine or Quinine
Concomitant use of quinidine or quinine with amantadine reduces renal clearance of amantadine by about 30%.
Thioridazine
Concomitant use of amantadine and thioridazine has been reported to worsen the tremor in geriatric patients with Parkinson's disease; however, it is not known if other phenothiazines produce a similar response.
Urine-Acidifying Agents
Concomitant use of urine-acidifying agents may increase elimination of amantadine.
Acute Toxicity
Manifestations
Fatalities have been reported following overdosage of amantadine. The lowest reported acute lethal dose of the drug has been 1 g.
Acute overdosage of amantadine has resulted in cardiac dysfunction (e.g., arrhythmia, tachycardia, hypertension); pulmonary edema and respiratory distress (including adult respiratory distress syndrome [ARDS]); renal dysfunction (e.g., increased BUN, decreased creatinine clearance, renal insufficiency); or CNS toxicity (e.g., insomnia, anxiety, aggressive behavior, hypertonia, hyperkinesia, tremor, confusion, disorientation, depersonalization, fear, delirium, hallucinations, psychotic reactions, lethargy, somnolence, coma). Hyperthermia also has occurred with amantadine overdosage. In addition, seizures may be exacerbated in patients with a history of a seizure disorder.
In a patient who ingested 2.8 g of amantadine hydrochloride, manifestations of amantadine overdosage included slightly dilated pupils that contracted minimally to light; urinary retention; mild, mixed acid-base disturbances; and an acute toxic psychosis manifested as disorientation, visual hallucinations, and aggressive behavior. A patient who ingested 2.5 g became comatose and developed cardiopulmonary arrest several hours after the ingestion. Although the arrest was treated successfully, during the arrest and subsequent 48 hours, ventricular tachyarrhythmias manifested as atypical ventricular tachycardia (torsades de pointes) and ventricular fibrillation occurred; therapy with adrenergic agents, particularly dopamine, appeared to exacerbate the ventricular tachyarrhythmias. The patient subsequently died of aspiration pneumonia and respiratory distress.
Treatment
There is no specific antidote for amantadine overdosage. If overdosage of amantadine is recent, prompt gastric lavage or induction of emesis is indicated. General supportive measures (including establishment of adequate respiratory exchange by maintenance of an airway, control of respiration and oxygen administration) should be instituted and cardiovascular status, blood pressure, pulse, respiration, temperature, serum electrolytes, urinary output, and urine pH should be monitored. Electrocardiographic monitoring may be necessary since malignant tachyarrhythmias can occur following amantadine overdosage. Fluids should be forced and, if necessary, given IV. Acidifying agents may be administered to increase the rate of amantadine excretion; only minimal amounts of amantadine are removed by hemodialysis. If there is no record of recent voiding, catheterization should be done.
The patient should be observed for hyperactivity and seizures; if required, sedatives and anticonvulsant therapy should be administered. Slow IV administration of physostigmine 1- and 2-mg doses at 1- to 2-hour intervals in one adult and 0.5-mg doses at 5- to 10-minute intervals (to a maximum of 2 mg/hour) in a child has been effective in the management of CNS toxicity caused by amantadine. However, the risk of physostigmine in the management of overdosage should be considered. Chlorpromazine was useful for the treatment of toxic psychosis in one patient. The patient also should be observed for the possible development of arrhythmias and hypotension; if required, appropriate antiarrhythmic and antihypotensive therapy should be administered. Caution should be employed when using adrenergic agents to maintain blood pressure and heart rate, since these agents may further predispose the patient to the development of serious ventricular tachyarrhythmias.
Mechanism of Action
The exact mechanism of the antiviral activity of amantadine has not been fully elucidated
Amantadine, like rimantadine, inhibits viral replication by interfering with the influenza A virus M2 protein, an integral membrane protein. The M2 protein of influenza A functions as a ion channel and is important in at least 2 aspects of virus replication, disassembly of the infecting virus particle and regulation of the ionic environment of the transport pathway. By interfering with the ion channel function of the M2 protein, amantadine inhibits 2 stages in the replicative cycle of influenza A. Early in the virus replicative cycle, amantadine inhibits uncoating of the virus particle, presumably by inhibiting the acid-mediated dissociation of the virion nucleic acid and proteins, which prevents nuclear transport of viral genome material. Amantadine also prevents viral maturation in some strains of influenza A (e.g., H7 strains) by promoting pH-induced conformational changes in influenza A hemagglutinin during its intracellular transport late in the replicative cycle. Adsorption of the virus to and penetration into cells do not appear to be affected by amantadine. In addition, amantadine does not interfere with the synthesis of viral components (e.g., RNA-directed RNA polymerase activity).
Amantadine treatment of established influenza A infection does not appear to interfere with antibody response to the infection; however, some reduction in local immune responses has been observed in some patients. Because prophylactic use of amantadine can prevent influenza illness and to a lesser extent subclinical infection, some individuals who take amantadine can still develop immune responses that may protect them when they are exposed to the same or antigenically related viruses following discontinuance of amantadine prophylaxis. Amantadine does not interfere with the immunogenicity of influenza virus vaccine inactivated.
Amantadine-mediated increases in lysosomal pH may inhibit virus-induced membrane fusion in enveloped RNA viruses that are susceptible to higher concentrations of amantadine than those required to inhibit influenza A.
Spectrum
Amantadine shares the antiviral spectrum of activity of rimantadine. Cell culture studies have shown that low concentrations of amantadine (i.e., less than 1 mcg/mL) produce an inhibitory action against susceptible influenza A, including susceptible strains of H1N1, H2N2, and H3N2.
Prior to the 2005–2006 influenza season, most influenza A (H3N2) strains circulating in the US were susceptible to adamantanes (amantadine, rimantadine). In addition, amantadine and rimantadine were active against most seasonal influenza A (H1N1) viruses circulating in the US during the 2008–2009 and 2009–2010 influenza seasons. However, seasonal influenza A (H3N2) and influenza A (H1N1)pdm09 viruses circulating during recent influenza seasons have been resistant to these drugs. (See Resistance.)
Although some strains of avian influenza A (H5N1) may be susceptible to amantadine in vitro, most avian influenza A virus strains tested (including H5N1 and H7N9) are resistant to adamantanes (amantadine, rimantadine).
In tissue culture systems, the 50% inhibitory concentration of amantadine for susceptible influenza A viruses ranges from 100 ng/mL to 25 mcg/mL depending on the assay protocol, size of the virus inoculum, influenza A strain, and the cell type used. By plaque inhibition, the 50% inhibitory concentration of rimantadine or amantadine for susceptible influenza A viruses ranges from 0.01 to less than 1 mcg/mL. The precise relationship between in vitro susceptibility of influenza A virus to amantadine and clinical response to therapy with the drug has not been determined. Results of several in vitro studies indicate that amantadine is less active on a weight basis than rimantadine.
Genetic studies indicate that the amino acid sequence in the transmembrane portion of the M2 protein of influenza A virus influences susceptibility of the virus to amantadine and rimantadine. Single amino acid changes in a critical transmembrane region of the M2 protein are associated with antiviral resistance to the drugs, providing further evidence of the importance of this domain in the protein as a target site for antiviral activity. There is some evidence that susceptibility of certain strains (e.g., H7) may be influenced by gene coding for the viral hemagglutinin.
Amantadine has little or no activity against influenza B at concentrations that inhibit influenza A. At very high concentrations (10–50 mcg/mL), the drug exhibits some in vitro activity against influenza B and other enveloped viruses (e.g., influenza C, parainfluenzae, respiratory syncytial virus), but this activity is considered clinically irrelevant because of the relatively high, potentially toxic doses that would be required.
Resistance
Influenza A viruses resistant to adamantanes (amantadine, rimantadine) can occur spontaneously or emerge rapidly during treatment with the drugs.
In vitro, resistance to amantadine can be produced at a relatively high frequency in strains of influenza A virus exposed to low concentrations of the drug. Influenza A virus strains with an in vitro EC50 (concentration of the drug required to produce a 50% reduction of antigenic material) exceeding 1 mcg/mL generally are considered resistant to amantadine. Naturally occurring amantadine-resistant strains of influenza A virus reportedly occur in vitro with a frequency of 1 in 104 to 1 in 103; however, such strains have been isolated in up to about 33% of individuals who have received amantadine or rimantadine therapy for influenza A infection, and resistant strains also have been isolated from individuals living at home or in an institution where other residents are taking or recently have taken one of these antivirals. Amantadine-resistant strains of influenza A can emerge within 2–3 days of initiating treatment with the drug. Individuals with influenza A infection who are receiving amantadine or rimantadine antiviral treatment may shed strains of the virus that are susceptible to the drugs early in the course of treatment; however, they also can shed resistant strains after 2–7 days of therapy. Immunocompromised patients may shed resistant strains for prolonged periods.
The mechanism(s) of resistance to amantadine has not been fully elucidated, but resistance to the drug appears to result from point mutations in the viral RNA segment 7 encoding the M2 protein that leads to amino acid alterations at residue 31 or nearby positions in the transmembrane portion of the M2 protein of the virus.
Although the frequency with which resistant strains emerge and the extent of their transmission have not been elucidated fully, limited evidence suggests that following treatment with amantadine in immunocompetent patients infected with initially susceptible strains of influenza A, 10–30% will shed amantadine-resistant virus. Limited information is available on the emergence of drug-resistant influenza A virus in immunocompromised patients receiving amantadine or rimantadine; isolates recovered from immunocompromised patients (adult bone marrow transplant recipients, adults with leukemia) who shed virus for longer than 3 days have been screened for antiviral susceptibility. While initial viral isolates were susceptible to amantadine or rimantadine, subsequent isolates from almost all of the patients were resistant.
Results of a study that screened circulating influenza A viruses obtained from various countries between 1994 and 2005 indicated a substantial increase in the percentage of amantadine- and rimantadine-resistant influenza A (H3N2) isolates in the US and Asia (China, Hong Kong, Taiwan, South Korea). In Asia, the incidence of such resistance was 1.1% in both 1995 and 2000 and increased to 24.3% in 2003 and 27% in 2004. In the US, the incidence of such resistance was 0.3% in 1995, 1.6% in 2000, and 1.9% in 2004; however, about 15% of influenza A (H3N2) strains obtained in the US from October 2004 to March 2005 were resistant to amantadine and rimantadine. Most strains of seasonal influenza A (H3N2) circulating in the US during the 2005–2006 influenza season contained the amino acid alteration associated with resistance to amantadine and rimantadine. Data from subsequent influenza seasons indicate that the incidence of resistance to adamantanes among influenza A (H3N2) isolates remains high.
Although amantadine and rimantadine were active against most seasonal influenza A (H1N1) viruses circulating in the US during the 2008–2009 and 2009–2010 influenza seasons, the influenza A (H1N1)pdm09 virus circulating during recent influenza seasons is resistant to the drugs.
Complete cross-resistance occurs between the adamantanes; influenza A viruses resistant to amantadine are resistant to rimantadine and vice versa.
Amantadine (Antiviral) Pharmacokinetics
Absorption
Amantadine hydrochloride is well absorbed from the GI tract. Mean peak blood amantadine concentrations of 0.3 mcg/mL have been reported to occur 1–4 hours after an oral dose of amantadine hydrochloride 2.5 mg/kg. Following oral administration of a single 100-mg capsule of amantadine hydrochloride, mean peak plasma concentrations of 0.22 mcg/mL occurred within 3.3 hours. Following oral administration of a single 100-mg dose of amantadine hydrochloride as the oral solution, peak plasma concentrations averaged 0.24 mcg/mL and were achieved within 2–4 hours. Peak plasma concentrations averaged 0.47 mcg/mL in individuals receiving amantadine hydrochloride oral solution 100 mg twice daily for 15 days. Following oral administration of amantadine hydrochloride 200 mg as a tablet in fasting adults 19–27 years of age or fasting geriatric individuals 60–70 years of age, peak plasma concentrations averaged 0.51 or 0.8 mcg/mL, respectively. While peak plasma concentrations are directly related to amantadine hydrochloride dose up to a dosage of 200 mg daily, dosages exceeding 200 mg daily may result in a greater than proportional increase in peak plasma concentration. In a small number of patients who received 300 mg of amantadine hydrochloride daily (200 mg in the morning and 100 mg in the afternoon), steady-state blood concentrations of 0.68–1.01 mcg/mL were reached after 4–5 days of therapy. In healthy young adults receiving 25, 100, or 150 mg twice daily, steady-state trough plasma concentrations averaged 0.11, 0.3, or 0.59 mcg/mL, respectively.
Plasma amantadine concentrations in geriatric patients receiving the drug in a dosage of 100 mg daily reportedly approximate those attained in younger adults receiving the drug in a dosage of 200 mg daily; it is not known whether this occurs because of normal decline in renal function or other age-related factors In one study, 3 patients with severe renal impairment showed symptoms of toxicity and elevated steady-state blood concentrations (2.5–4.4 mcg/mL) following 200 mg of amantadine hydrochloride daily. One metabolite, acetylamantadine, has been detected in plasma in less than 50% of individuals receiving a single amantadine hydrochloride 200-mg dose. In those individuals with detectable plasma acetylamantadine, concentration of the metabolite represented up to 80% of the concurrent amantadine concentration.
Distribution
Distribution of amantadine hydrochloride into body tissues and fluids has not been fully characterized.
In animals, amantadine is distributed into heart, lung, liver, kidney, and spleen. In a study in mice, lung tissue concentrations of amantadine were much higher than blood concentrations.
Following oral administration, amantadine is distributed into nasal secretions in concentrations that are lower than plasma concentrations. Following oral administration of a single 200-mg dose of amantadine hydrochloride in healthy young and geriatric adults, amantadine concentrations in nasal secretions or plasma averaged 0.15 mcg/g or 0.58 mcg/mL at 1 hour, 0.28 mcg/g or 51 mcg/mL at 4 hours, and 0.39 mcg/g or 0.45 mcg/mL at 8 hours. A substantial proportion of amantadine appears to distribute into erythrocytes, with an erythrocyte to plasma ratio of 2.7 reported in men with normal renal function and 1.4 in men with substantial renal impairment. In one patient, the CSF concentration of amantadine was approximately one-half the blood concentration. Amantadine distributes into human breast milk.
The volume of distribution following IV administration of amantadine reportedly is 3–8 L/kg in healthy individuals. Amantadine is about 67% bound to plasma proteins over a concentration range of 0.1–2 mcg/mL.
Elimination
The elimination half-life of amantadine has been variously reported as 9–37 hours, with an average of 24 hours or less. Clearance of amantadine is reduced, plasma concentrations of the drug are increased, and elimination half-life may be prolonged in healthy geriatric adults compared with healthy young adults. A half-life of 29 hours (range: 20–41 hours) has been reported in geriatric men 60–76 years of age. In addition, the half-life of amantadine is prolonged at least twofold to threefold in patients with impaired renal function (i.e., creatinine clearance less than 40 mL/minute per 1.73 m2). In one study, the half-life ranged from 18.5–81.3 hours in patients with creatinine clearances of 13.7–43.1 mL/minute per 1.73 m2 and averaged 8.3 days (range: 7–10.3 days) in patients undergoing chronic hemodialysis.
While amantadine principally is excreted unchanged in urine by glomerular filtration and tubular secretion, at least 8 metabolites have been identified in urine. Amantadine undergoes N-acetylation, and about 5–15% of an absorbed dose is excreted in urine as acetylamantadine. Whether this metabolic pathway is affected by acetylator phenotype remains to be determined. The clinical importance of amantadine metabolites is unknown. Acidification of urine increases the rate of amantadine excretion, and administration of urine-acidifying drugs may increase amantadine elimination from the body. Amantadine is only minimally removed by hemodialysis.
Chemistry and Stability
Chemistry
Amantadine hydrochloride is a synthetic adamantane-derivative (a symmetric tricyclic amine) antiviral agent. Amantadine is structurally related to rimantadine, differing only in the side chain of the 10 carbon ring. While the structure-activity relationship of the adamantanes remains to be determined, the octanol/water coefficient for amantadine is substantially lower than that for rimantadine.
Amantadine hydrochloride occurs as a white or practically white, crystalline powder which has a bitter taste and has solubilities of approximately 400 mg/mL in water and 200 mg/mL in alcohol at 25°C. Amantadine hydrochloride has a pKa of 9.
Stability
Commercially available amantadine hydrochloride tablets, liquid-filled capsules, and oral solution should be stored in tight containers at 20–25°C, but may be exposed to temperatures ranging from 15–30°C.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
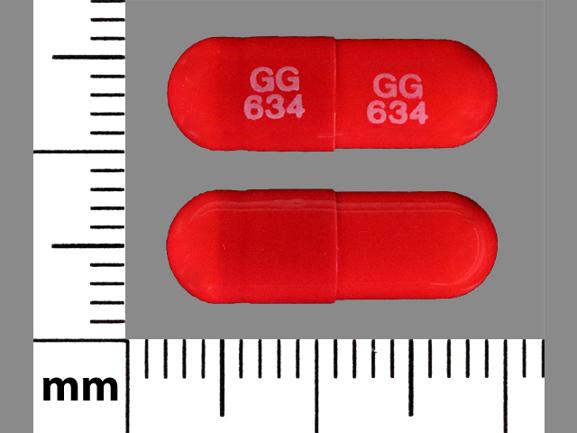
Capsules, liquid-filled |
100 mg* |
Amantadine Hydrochloride Capsules |
|
|
Solution |
50 mg/5 mL* |
Amantadine Hydrochloride Oral Solution |
||
|
Tablets |
100 mg* |
Amantadine Hydrochloride Tablets |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions April 25, 2014. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Frequently asked questions
- What is the difference between Osmolex ER and Gocovri?
- What is Gocovri used to treat?
- Why should you not discontinue amantadine?
- How long does it take for amantadine to start working?
- Why was amantadine discontinued for flu?
- What symptoms does amantadine treat?
- What is Gocovri (amantadine) and how does it work?
More about amantadine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (52)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: adamantane antivirals
- Breastfeeding
- En español
Patient resources
- Amantadine drug information
- Amantadine Extended-Release Tablets
- Amantadine Extended-Release Capsules
Professional resources
- Amantadine prescribing information
- Amantadine Oral Solution USP (FDA)
- Amantadine Syrup (FDA)
- Amantadine Tablets (FDA)