quiNINE (Monograph)
Brand name: Qualaquin
Drug class: Antimalarials
VA class: AP101
Chemical name: (8S,9R)-6′-Methoxycinchonan-9-ol
Molecular formula: C20H24N2O2
CAS number: 60-93-5
Warning
-
Serious and life-threatening hematologic reactions, including thrombocytopenia and hemolytic uremic syndrome/thrombotic thrombocytopenic purpura (HUS/TTP), may occur if quinine used for treatment or prevention of nocturnal leg cramps† [off-label].
-
Chronic renal impairment associated with TTP reported.
-
Known risks associated with use of quinine, in the absence of evidence of safety and efficacy of the drug for treatment or prevention of nocturnal leg cramps† [off-label], outweigh any potential benefits for this unlabeled indication. (See Use for Treatment or Prevention of Nocturnal Leg Cramps under Cautions.)
Introduction
Antimalarial; alkaloid obtained from bark of the cinchona tree.
Uses for quiNINE
Treatment of Uncomplicated Malaria
Treatment of uncomplicated malaria caused by Plasmodium falciparum. Also used for treatment of uncomplicated malaria caused by chloroquine-resistant P. vivax† [off-label] and treatment of uncomplicated malaria when plasmodial species not identified† [off-label].
Designated an orphan drug by FDA for treatment of malaria. Since malaria is a life-threatening infection, FDA states that potential benefits of the drug outweigh associated risks and justify its use for treatment of malaria.
For treatment of uncomplicated malaria caused by chloroquine-resistant P. falciparum or treatment of uncomplicated malaria when plasmodial species not identified, CDC recommends fixed combination of atovaquone and proguanil (atovaquone/proguanil), fixed combination of artemether and lumefantrine (artemether/lumefantrine), or regimen of quinine in conjunction with doxycycline, tetracycline, or clindamycin. If quinine regimen used, concomitant doxycycline or tetracycline generally preferred instead of concomitant clindamycin since more efficacy data exist regarding antimalarial regimens that include tetracyclines.
For treatment of uncomplicated malaria caused by chloroquine-susceptible P. falciparum, P. malariae, or P. knowlesi or treatment of uncomplicated malaria when plasmodial species not identified and infection acquired in areas where chloroquine resistance not reported, CDC recommends chloroquine (or hydroxychloroquine). Alternatively, CDC states that any of the regimens recommended for treatment of uncomplicated chloroquine-resistant P. falciparum malaria may be used if preferred, more readily available, or more convenient.
For treatment of uncomplicated malaria caused by chloroquine-resistant P. vivax† [off-label], CDC recommends regimen of quinine and doxycycline (or tetracycline) given in conjunction with primaquine, atovaquone/proguanil given in conjunction with primaquine, or mefloquine given in conjunction with primaquine. Because quinine, doxycycline (or tetracycline), atovaquone/proguanil, and mefloquine active only against asexual erythrocytic forms of Plasmodium (not exoerythrocytic stages), 14-day regimen of primaquine indicated to prevent delayed primary attacks or relapse and provide a radical cure whenever any of these drugs used for treatment of P. vivax or P. ovale malaria.
Pediatric patients with uncomplicated malaria generally can receive same treatment regimens recommended for adults using age- and weight-appropriate drugs and dosages. For treatment of uncomplicated chloroquine-resistant P. falciparum in children <8 years of age, atovaquone/proguanil or artemether/lumefantrine usually recommended; mefloquine can be considered if no other options available. If a quinine regimen used in children <8 years of age, CDC states a 7-day regimen of quinine alone can be used (regardless of where infection was acquired) or quinine can be given in conjunction with clindamycin, since children <8 years of age generally should not receive tetracyclines. In rare instances, doxycycline or tetracycline can be used in conjunction with quinine in children <8 years of age if other treatment options not available or not tolerated and if potential benefits of including a tetracycline outweigh risks. For treatment of chloroquine-resistant P. vivax malaria in children <8 years of age, CDC recommends mefloquine given in conjunction with primaquine. Alternatively, if mefloquine not available or not tolerated and if potential benefits outweigh risks, atovaquone/proguanil or artemether/lumefantrine can be used for treatment of chloroquine-resistant P. vivax in this age group.
Pregnant women with uncomplicated malaria caused by P. malariae, P. vivax, P. ovale, or chloroquine-susceptible P. falciparum should receive prompt treatment with chloroquine (or hydroxychloroquine). CDC recommends that pregnant women with uncomplicated malaria caused by chloroquine-resistant P. falciparum receive prompt treatment with mefloquine or a regimen of quinine and clindamycin; mefloquine recommended for those with uncomplicated malaria caused by chloroquine-resistant P. vivax. Although tetracyclines generally contraindicated in pregnant women, in rare circumstances when other treatment options not available or not tolerated and if potential benefits outweigh risks, CDC states that regimen of quinine and doxycycline (or tetracycline) may be used. (See Pregnancy under Cautions.) Alternatively, atovaquone/proguanil or artemether/lumefantrine can be considered for treatment of uncomplicated malaria caused by chloroquine-resistant P. falciparum in pregnant women when other treatment options not available or not tolerated and if potential benefits outweigh risks. Pregnant women with P. vivax or P. ovale malaria should receive chloroquine prophylaxis for the duration of the pregnancy and receive primaquine after delivery to provide a radical cure.
Assistance with diagnosis or treatment of malaria available from CDC Malaria Hotline at 770-488-7788 or 855-856-4713 from 9:00 a.m. to 5:00 p.m. Eastern Standard Time or CDC Emergency Operation Center at 770-488-7100 after hours and on weekends and holidays.
Treatment of Severe Malaria
Used in conjunction with doxycycline, tetracycline, or clindamycin for follow-up treatment of severe or complicated malaria†.
Severe malaria usually caused by P. falciparum and requires initial aggressive treatment with a parenteral antimalarial regimen initiated as soon as possible after diagnosis.
For treatment of severe malaria in adults and children, CDC recommends an initial regimen of IV quinidine in conjunction with doxycycline, tetracycline, or clindamycin (administered orally or IV as tolerated). After parasitemia reduced to <1% and oral therapy tolerated, IV quinidine can be discontinued and oral quinine initiated to complete 7 or 3 days of total quinidine and quinine therapy as determined by geographic origin of infecting parasite (7 days if malaria was acquired in Southeast Asia or 3 days if acquired elsewhere).
If IV quinidine unavailable or cannot be used for initial treatment because of adverse effects or contraindications, parenteral artesunate may be available from CDC under an investigational new drug (IND) protocol for emergency initial treatment of severe malaria.
Assistance with diagnosis or treatment of malaria and assistance obtaining quinidine or artesunate for treatment of severe malaria is available by contacting CDC Malaria Hotline at 770-488-7788 or 855-856-4713 from 9:00 a.m. to 5:00 p.m. Eastern Standard Time or CDC Emergency Operation Center at 770-488-7100 after hours and on weekends and holidays.
Presumptive Self-treatment of Malaria
Regimen of quinine in conjunction with doxycycline has been recommended by some clinicians for presumptive self-treatment of malaria† in travelers.
Not approved by FDA for presumptive self-treatment of malaria in travelers and not recommended by CDC for such treatment.
For presumptive self-treatment of malaria in travelers, CDC and other experts recommend atovaquone/proguanil or artemether/lumefantrine.
Prevention of Malaria
Not approved by FDA for prevention (prophylaxis) of malaria and not included in current CDC recommendations for prevention of malaria.
CDC and other clinicians recommend other antimalarials (e.g., chloroquine [or hydroxychloroquine], atovaquone/proguanil, doxycycline, mefloquine) for prevention of malaria caused by susceptible plasmodia.
Information on risk of malaria in specific countries and mosquito avoidance measures and recommendations regarding whether prevention of malaria indicated and choice of antimalarials for prevention are available from CDC at [Web] and [Web].
Babesiosis
Treatment of babesiosis† caused by Babesia microti.
IDSA states that all patients with active babesiosis (i.e., symptoms of viral-like infection and identification of babesial parasites in blood smears or by polymerase chain reaction [PCR] amplification of babesial DNA) should receive anti-infective treatment because of the risk of complications; however, symptomatic patients whose serum contains antibody to babesia but whose blood lacks identifiable babesial parasites on smear or babesial DNA by PCR should not receive treatment. Treatment not recommended initially for asymptomatic individuals, regardless of results of serologic examination, blood smears, or PCR, but should be considered if parasitemia persists for >3 months.
When anti-infective treatment of babesiosis indicated, IDSA and other clinicians recommend a regimen of quinine and clindamycin or a regimen of atovaquone and azithromycin.
The quinine and clindamycin regimen may be preferred for severe babesiosis. However, there is some evidence that, in patients with mild or moderate illness, the atovaquone and azithromycin regimen may be as effective and better tolerated than the quinine and clindamycin regimen. Consider use of exchange transfusions, especially in severely ill patients with high levels of parasitemia (≥10%), significant hemolysis, or compromised renal, hepatic, or pulmonary function.
B. microti is transmitted by Ixodes scapularis ticks, which also may be simultaneously infected with and transmit Borrelia burgdorferi (causative agent of Lyme disease) and Anaplasma phagocytophilum (causative agent of human granulocytotropic anaplasmosis [HGA, formerly known as human granulocytic ehrlichiosis]). Consider possibility of coinfection with B. burgdorferi and/or A. phagocytophilum in patients who have severe or persistent symptoms despite appropriate anti-infective treatment for babesiosis.
Nocturnal Recumbency Leg Muscle Cramps
Not approved by FDA for the treatment or prevention of nocturnal leg cramps†. Should not be used in the management of this or related conditions (e.g. restless legs syndrome†).
Although quinine has been used in the past for the prevention and treatment of nocturnal recumbency leg muscle cramps† (night cramps), there are no adequate and well-controlled studies evaluating efficacy and safety for this use.
Quinine has a narrow margin of safety and may cause unpredictable serious and life-threatening hypersensitivity reactions, QT interval prolongation, serious cardiac arrhythmias (including torsades de pointes), serious hematologic reactions (including thrombocytopenia and HUS/TTP), and other serious adverse events (e.g., blindness, deafness) requiring medical intervention and hospitalization. Fatalities associated with use of the drug have been reported. (See Cautions.) The known risks associated with the use of quinine, in the absence of evidence of safety and efficacy of the drug for the treatment or prevention of nocturnal leg cramps†, outweigh any potential benefits for this benign, self-limiting condition.
FDA has determined that quinine preparations (including preparations containing any quinine salt alone or in fixed combination with vitamin E) are not generally recognized as safe and effective for treatment or prevention of nocturnal leg muscle cramps. Promotion of quinine for self-medication of nocturnal leg cramps has been prohibited in the US since February 1995 because of safety concerns. In addition, FDA ordered that marketing of all unapproved quinine preparations be discontinued as of December 11, 2006. (See Preparations.)
quiNINE Dosage and Administration
Administration
Quinine is administered orally as quinine sulfate.
Although quinine has been administered by slow IV infusion as quinine dihydrochloride, a parenteral preparation of the drug no longer available for use in the US, either commercially or from CDC. When parenteral antimalarial therapy indicated, use IV quinidine gluconate.
Oral Administration
Administer orally.
Take with food to minimize possible GI irritation.
Dosage
Available as quinine sulfate; dosage expressed in terms of the salt.
The only FDA-approved preparations of quinine currently commercially available in US are capsules containing 324 mg of quinine sulfate (Qualaquin, generic); the drug was previously available in US as capsules containing 325 mg. This difference in quinine preparations may result in minor disparities between some published dosage recommendations that were based on the previously available 325-mg capsules and dosage recommendations for the currently available 324-mg capsules.
Pediatric Patients
Malaria
Treatment of Uncomplicated Malaria Caused by Chloroquine-resistant P. falciparum or Unidentified Plasmodial Species
OralChildren ≥8 years of age†: 10 mg/kg 3 times daily for 7 or 3 days as determined by geographic origin of infecting parasite (7 days if malaria acquired in Southeast Asia or 3 days if acquired elsewhere). Use in conjunction with a 7-day regimen of oral doxycycline, tetracycline, or clindamycin.
Children <8 years of age†: If quinine regimen used, CDC states quinine monotherapy may be given for 7 days or quinine can be given in conjunction with clindamycin for the usually recommended duration. In rare circumstances, a regimen of quinine and doxycycline or tetracycline can be considered. (See Treatment of Uncomplicated Malaria under Uses.)
Do not exceed usual adult dosage.
Treatment of Uncomplicated Malaria Caused by Chloroquine-resistant P. vivax†
OralChildren ≥8 years of age†: 10 mg/kg 3 times daily for 7 or 3 days as determined by geographic origin of infecting parasite (7 days if malaria acquired in Southeast Asia or 3 days if acquired elsewhere). Do not exceed usual adult dosage.
Use in conjunction with 7-day regimen of oral doxycycline or tetracycline. A 14-day regimen of primaquine also indicated to provide a radical cure and prevent delayed attacks or relapse of P. vivax malaria.
Treatment of Severe Malaria†
Oral10 mg/kg 3 times daily to complete 7 or 3 days of total IV quinidine and oral quinine therapy as determined by geographic origin of infecting parasite (7 days if malaria acquired in Southeast Asia or 3 days if acquired elsewhere). Do not exceed usual adult dosage.
IV quinidine gluconate must be used initially; after ≥24 hours and after parasitemia reduced to <1% and oral therapy tolerated, oral quinine may be substituted.
Use quinidine/quinine regimen in conjunction with 7-day regimen of doxycycline, tetracycline, or clindamycin (administered IV or orally as tolerated).
Presumptive Self-treatment of Malaria†
Oral10 mg/kg 3 times daily for 7 or 3 days as determined by geographic origin of infecting parasite (7 days if malaria acquired in Southeast Asia or 3 days if acquired elsewhere) given in conjunction with a 7-day regimen of oral doxycycline.
Not included in current CDC recommendations for presumptive self-treatment of malaria in travelers.
Babesiosis†
Oral
IDSA recommends 8 mg/kg (up to 650 mg) every 8 hours in conjunction with clindamycin (7–10 mg/kg [up to 600 mg] IV or orally every 6–8 hours) given for 7–10 days.
Other clinicians recommend 30 mg/kg daily in 3 divided doses given for 7–10 days in conjunction with oral clindamycin (20–40 mg/kg daily in 3 divided doses for 7–10 days).
For mild to moderate babesiosis, clinical improvement should be evident within 48 hours after initiation of treatment and symptoms should resolve completely within 3 months. Low-grade parasitemia may persist in some patients for months after completion of treatment. Regardless of presence or absence of symptoms, IDSA suggests that retreatment be considered if babesial parasites or amplifiable babesial DNA detected in blood ≥3 months after initial treatment.
Adults
Malaria
Treatment of Uncomplicated Malaria Caused by Chloroquine-resistant P. falciparum or Unidentified Plasmodial Species
OralManufacturers recommend 648 mg every 8 hours for 7 days for P. falciparum malaria. Manufacturers caution that shorter regimens (3 days) have been used, but data regarding these regimens limited and they may be less effective than a 7-day regimen.
CDC and other clinicians recommend 650 mg (two 324-mg capsules) every 8 hours for 7 or 3 days as determined by geographic origin of infecting parasite (7 days if malaria acquired in Southeast Asia or 3 days if acquired elsewhere). Use in conjunction with 7-day regimen of oral doxycycline, tetracycline, or clindamycin.
Pregnant women: CDC recommends 650 mg (two 324-mg capsules) every 8 hours for 7 or 3 days as determined by geographic origin of infecting parasite (7 days if malaria acquired in Southeast Asia or 3 days if acquired elsewhere). Use in conjunction with 7-day regimen of oral clindamycin. Alternatively, if benefits outweigh risks, used in conjunction with oral doxycycline or tetracycline.
Treatment of Uncomplicated Malaria Caused by Chloroquine-resistant P. vivax†
Oral650 mg (two 324-mg capsules) every 8 hours for 7 or 3 days as determined by geographic origin of infecting parasite (7 days if malaria acquired in Southeast Asia or 3 days if acquired elsewhere). Use in conjunction with 7-day regimen of oral doxycycline or tetracycline. A 14-day regimen of primaquine also indicated to provide a radical cure and prevent delayed attacks or relapse of P. vivax malaria.
Pregnant women: CDC recommends 650 mg (two 324-mg capsules) every 8 hours for 7 days (regardless of where infection was acquired). Used alone or, if benefits outweigh risks, used in conjunction with oral doxycycline or tetracycline. Then, give chloroquine (300 mg [500 mg of chloroquine phosphate] once weekly) as prophylaxis for the duration of the pregnancy until primaquine can be given after delivery to provide a radical cure and prevent relapse.
Treatment of Severe Malaria†
Oral650 mg (two 324-mg capsules) every 8 hours to complete 7 or 3 days of total IV quinidine and oral quinine therapy as determined by geographic origin of infecting parasite (7 days if malaria acquired in Southeast Asia or 3 days if acquired elsewhere).
IV quinidine gluconate must be used initially; after ≥24 hours and after parasitemia reduced to <1% and oral therapy tolerated, oral quinine may be substituted.
Use quinidine/quinine regimen in conjunction with 7-day regimen of doxycycline, tetracycline, or clindamycin (administered IV or orally as tolerated).
Presumptive Self-treatment of Malaria†
Oral650 mg every 8 hours given for 7 or 3 days (7 days if malaria acquired in Southeast Asia or 3 days if acquired elsewhere) in conjunction with a 7-day regimen of oral doxycycline.
Not included in current CDC recommendations for presumptive self-treatment of malaria in travelers.
Babesiosis†
Oral
IDSA and other clinicians recommend 650 mg every 6–8 hours in conjunction with clindamycin (300–600 mg IV every 6 hours or 600 mg orally every 8 hours) given for 7–10 days.
For mild to moderate babesiosis, clinical improvement should be evident within 48 hours after initiation of treatment and symptoms should resolve completely within 3 months. Low-grade parasitemia may persist in some patients for months after completion of treatment. Regardless of presence or absence of symptoms, IDSA suggests that retreatment be considered if babesial parasites or amplifiable babesial DNA detected in blood ≥3 months after initial treatment.
Prescribing Limits
Pediatric Patients
Treatment of Uncomplicated or Severe Malaria
Oral
Do not exceed usual adult dosage.
Babesiosis
Oral
Maximum 650 mg per dose.
Special Populations
Hepatic Impairment
Treatment of Uncomplicated Malaria
Mild to moderate hepatic impairment (Child-Pugh class A or B): Dosage adjustment not necessary; monitor closely for adverse effects.
Severe hepatic impairment (Child-Pugh class C): Do not use. (See Hepatic Impairment under Cautions.)
Renal Impairment
Treatment of Uncomplicated Malaria
Severe chronic renal failure: 648-mg loading dose followed 12 hours later by maintenance doses of 324 mg given every 12 hours; dosage based on computer models.
Mild or moderate renal impairment: Safety and pharmacokinetics not determined to date.
Geriatric Adults
Treatment of Uncomplicated Malaria
Dosage adjustment not necessary.
Cautions for quiNINE
Contraindications
-
Hypersensitivity to quinine.
-
History of potential hypersensitivity reactions associated with previous quinine use, including (but not limited to) thrombocytopenia, TTP, idiopathic thrombocytopenic purpura (ITP), HUS, or blackwater fever (acute intravascular hemolysis, hemoglobinuria, and hemoglobinemia). (See Hypersensitivity Reactions under Cautions.)
-
Hypersensitivity to mefloquine or quinidine. (See Hypersensitivity Reactions under Cautions.)
-
Prolonged QT interval. (See QT Prolongation and Other Cardiovascular Effects under Cautions.)
-
Glucose-6-phosphate dehydrogenase (G-6-PD) deficiency. (See G-6-PD Deficiency under Cautions.)
-
Myasthenia gravis. (See Myasthenia Gravis under Cautions.)
-
Optic neuritis.
Warnings/Precautions
Warnings
Use for Treatment or Prevention of Nocturnal Leg Cramps†
Quinine has a narrow margin of safety and may cause unpredictable serious and life-threatening hypersensitivity reactions, QT interval prolongation, serious cardiac arrhythmias (including torsades de pointes), serious hematologic reactions (including thrombocytopenia and HUS/TTP), and other serious adverse events (e.g., blindness, deafness) requiring medical intervention and hospitalization. Fatalities reported.
Quinine not approved by FDA for treatment or prevention of nocturnal leg cramps†, and should not be used in the management of this or related conditions (e.g., restless legs syndrome†). The known risks associated with use of quinine, in the absence of evidence of safety and efficacy of the drug for treatment or prevention of nocturnal leg cramps†, outweigh any potential benefits for this benign, self-limiting condition.
FDA has determined that quinine preparations (including preparations containing any quinine salt alone or in fixed combination with vitamin E) are not generally recognized as safe and effective for treatment or prevention of nocturnal leg muscle cramps†. Promotion of quinine for self-medication of nocturnal leg cramps† has been prohibited in the US since February 1995 because of safety concerns.
Because of serious safety concerns, FDA initiated several regulatory actions in December 2006 to remove unapproved quinine preparations from the US market. Despite these efforts, quinine still being prescribed for uses other than malaria, and FDA continues to receive reports of serious adverse effects associated with the drug.
From April 2005 to October 2008, the FDA Adverse Event Reporting System (AERS) received 38 reports of serious adverse events associated with quinine (e.g., hematologic events, cardiovascular events, GI symptoms, hearing loss, rash, electrolyte imbalance, drug interactions). The majority of these reports (66%) involved patients who used quinine for unlabeled indications (prevention or treatment of leg cramps or restless leg syndrome†), and most (63%) involved serious or potentially fatal hematologic events. (See Hematologic Effects under Cautions.)
Hematologic Effects
Serious, life-threatening, and sometimes fatal hematologic reactions, including thrombocytopenia and HUS/TTP, have been reported in patients receiving quinine, especially those using the drug for unlabeled indications (prevention or treatment of leg cramps or restless leg syndrome†). Subsequent development of chronic renal impairment has occurred in patients with quinine-associated TTP.
In 24 reported cases of serious hematologic reactions, median time to onset was approximately 2 weeks after initiation of quinine. Most recovered when the drug was discontinued and other therapeutic interventions initiated, but there were 2 fatalities (one related to TTP and the other related to hemolysis).
If thrombocytopenia occurs, discontinue quinine since continued therapy puts patient at risk for fatal hemorrhage. Thrombocytopenia usually resolves within 1 week after quinine discontinued. Quinine-induced thrombocytopenia is immune-mediated and re-exposure to quinine from any source may result in a more rapid and more severe course of thrombocytopenia compared to original episode.
QT Prolongation and Other Cardiovascular Effects
QT interval prolongation has been a consistent finding in studies evaluating ECG changes in individuals receiving oral or parenteral quinine and has occurred independent of age, clinical status, or disease severity. Maximal increases in QT interval correlate with peak plasma quinine concentrations.
Concentration-dependent prolongation of PR and QRS intervals also reported in patients receiving oral quinine. Patients with underlying structural heart disease and preexisting conduction system abnormalities, geriatric patients with sick sinus syndrome, patients with atrial fibrillation with slow ventricular response, patients with myocardial ischemia, and patients receiving drugs known to prolong the PR interval (e.g., verapamil) or QRS interval (e.g., flecainide, quinidine) are at particular risk.
Potentially fatal cardiac arrhythmias, including torsades de pointes and ventricular fibrillation, reported. At least 1 case of fatal ventricular arrhythmia reported in a geriatric patient with preexisting prolonged QT interval who received IV quinine sulfate for treatment of P. falciparum malaria.
Do not use in patients with known prolonged QT interval. Avoid use in patients with clinical conditions known to prolong the QT interval (e.g., uncorrected hypokalemia, bradycardia, certain cardiac conditions).
Use caution in patients with atrial fibrillation or atrial flutter. A paradoxical increase in ventricular response rate may occur with quinine, similar to that observed with quinidine. Monitor closely if digoxin used to prevent a rapid ventricular response. (See Digoxin under Interactions.)
Do not use concomitantly with other drugs known to cause QT interval prolongation, including class IA antiarrhythmic agents (e.g., quinidine, procainamide, disopyramide) and class III antiarrhythmic agents (e.g., amiodarone, sotalol, dofetilide). (See Drugs That Prolong the QT Interval under Interactions.)
Avoid use with drugs that are CYP3A4 substrates and are known to cause QT prolongation (e.g., cisapride [available in the US only under a limited-use protocol], pimozide, halofantrine [not commercially available in the US], quinidine). (See Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes under Interactions.)
G-6-PD Deficiency
Potential for hemolysis and hemolytic anemia if used in patients with G-6-PD deficiency. Discontinue immediately if evidence of hemolysis occurs.
Do not use in patients with G-6-PD deficiency.
Myasthenia Gravis
Has neuromuscular blocking activity and may exacerbate muscle weakness if used in patients with myasthenia gravis.
Do not use in patients with myasthenia gravis.
Sensitivity Reactions
Hypersensitivity Reactions
Serious hypersensitivity reactions, including anaphylactic shock, anaphylactoid reactions, urticaria, serious rashes (e.g., Stevens-Johnson syndrome, toxic epidermal necrolysis), angioedema, facial edema, bronchospasm, and pruritus, reported.
Other serious adverse reactions also reported and may be due to hypersensitivity, including thrombocytopenia, HUS/TTP, ITP, blackwater fever, disseminated intravascular coagulation, leukopenia, neutropenia, granulomatous hepatitis, and acute interstitial nephritis. (See Hematologic Effects under Cautions.)
Cross-sensitivity to quinine has been documented in individuals hypersensitive to mefloquine or quinidine.
Discontinue quinine if there are signs or symptoms of hypersensitivity (rash, hives, severe itching, severe flushing, trouble breathing).
Photosensitivity Reactions
Photosensitivity reported.
General Precautions
Cinchonism
A cluster of symptoms referred to as “cinchonism” occurs in practically all patients receiving quinine. Most manifestations of cinchonism are reversible and resolve following discontinuance of quinine.
Manifestations of mild cinchonism include headache, vasodilation and sweating, nausea, tinnitus, hearing impairment, vertigo or dizziness, blurred vision, and disturbance in color perception. More severe cinchonism manifests as vomiting, diarrhea, abdominal pain, deafness, blindness, and disturbances in cardiac rhythm or conduction.
Hypoglycemia
Quinine stimulates release of insulin from the pancreas, and quinine-induced hypoglycemia has been reported.
Clinically important hypoglycemia may occur, especially in pregnant women.
Male Fertility
Decreased sperm motility and increased percentage of sperm with abnormal morphology reported from a study in 5 men receiving quinine (600 mg 3 times daily for 1 week). Testicular toxicity (e.g., atrophy or degeneration of seminiferous tubules, decreased sperm count and motility, decreased testosterone concentrations in serum and testes) reported in animals.
Specific Populations
Pregnancy
Category C.
Manufacturers states quinine should be used during pregnancy only if potential benefits justify potential risks to the fetus.
CDC recommends quinine and clindamycin as a regimen of choice for treatment of uncomplicated chloroquine-resistant P. falciparum malaria in pregnant women. (See Treatment of Uncomplicated Malaria under Uses.)
Crosses the placenta. Although quinine concentrations may be measurable in the fetus and cord blood of women who received the drug near the time of delivery (see Distribution under Pharmacokinetics), such concentrations may not be therapeutic for the fetus. If congenital malaria suspected, evaluate infant after delivery and treat with antimalarial agents if appropriate.
Deafness and optic nerve hypoplasia reported rarely in children exposed in utero when the mother received high-dose quinine therapy during pregnancy.
Although published data of >1000 pregnancies exposed to quinine (majority of exposures occurred after first trimester) have not shown an increase in teratogenic effects over background rates in the general population, there are few well-controlled studies to date evaluating the drug in pregnant women.
In animal studies evaluating sub-Q or IM quinine, teratogenic or fetotoxic effects (e.g., death in utero, degenerated auditory nerve and spiral ganglion, CNS anomalies, hemorrhage, mitochondrial changes in cochlea) demonstrated in some species.
Hypoglycemia, due to increased pancreatic secretion of insulin, has been associated with quinine use, especially in pregnant women.
No evidence to date that quinine causes uterine contractions at dosages recommended for the treatment of malaria; doses several fold higher than those used to treat malaria may stimulate the pregnant uterus.
Lactation
Distributed into milk.
Only limited information available regarding safety of quinine in breast-fed infants. Although quinine generally considered compatible with breast-feeding, assess the risks and benefits to the infant and mother and use with caution in nursing women.
Plasma quinine concentrations may not be therapeutic in infants of nursing mothers receiving quinine. If malaria suspected in the infant, provide appropriate evaluation and treatment.
Pediatric Use
Safety and efficacy not established in children <16 years of age.
Quinine is included in CDC recommendations for treatment of uncomplicated malaria in pediatric patients†. (See Treatment of Uncomplicated Malaria under Uses.) The drug also is used for follow-up after an initial parenteral antimalarial regimen in children with severe malaria†. (See Treatment of Severe Malaria under Uses.)
Geriatric Use
Clinical studies did not include sufficient numbers of individuals ≥65 years of age to determine whether they respond differently than younger adults. Other reported clinical experience has not identified differences in responses between geriatric adults and younger patients.
Closely monitor geriatric patients for adverse effects.
Hepatic Impairment
If used in adults with mild to moderate hepatic impairment (Child-Pugh class A or B), monitor closely for adverse effects associated with quinine.
Do not use in patients with severe hepatic impairment (Child-Pugh class C); oral clearance is decreased, volume of distribution increased, and half-life of the drug prolonged relative to individuals with normal hepatic function.
Renal Impairment
Reduced dosage recommended when used for treatment of acute uncomplicated malaria in adults with severe chronic renal failure. (See Renal Impairment under Dosage and Administration.) The effects of mild or moderate renal impairment on safety and pharmacokinetics not determined to date.
Common Adverse Effects
Mild cinchonism, manifested as headache, vasodilation and sweating, nausea, tinnitus, hearing impairment, vertigo or dizziness, blurred vision, and disturbance in color perception, occurs in most patients. More severe cinchonism, manifested as vomiting, diarrhea, abdominal pain, deafness, blindness, and disturbances in cardiac rhythm or conduction, also reported.
Drug Interactions
Metabolized principally by CYP3A4; may also be metabolized by other CYP enzymes, including 1A2, 2C8, 2C9, 2C19, 2D6, and 2E1.
Drugs That Prolong the QT Interval
Because quinine prolongs the QT interval, an additive effect on the QT interval might occur if the drug is administered with other drugs that prolong the QT interval. Concomitant use of quinine and other drugs known to cause QT prolongation, including class IA antiarrhythmic agents (e.g., quinidine, procainamide, disopyramide) and class III antiarrhythmic agents (e.g., amiodarone, sotalol, dofetilide), not recommended.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
In vivo and in vitro drug interaction studies suggest quinine may inhibit metabolism of drugs that are substrates of CYP3A4 and 2D6.
Avoid use with drugs that are CYP3A4 substrates and are known to cause QT prolongation (e.g., cisapride [available in the US only under a limited-use protocol], pimozide, halofantrine [not commercially available in the US], quinidine).
Quinine has been shown to decrease metabolism of desipramine in some patients (see Desipramine under Interactions) and may decrease metabolism of some other drugs that are CYP2D6 substrates (e.g., debrisoquine [not commercially available in the US], dextromethorphan, flecainide, methoxyphenamine [not commercially available in the US], metoprolol, paroxetine). If used concomitantly with a CYP2D6 substrate, monitor closely for adverse effects associated with the CYP2D6 substrate.
Drugs Affecting or Affected by P-glycoprotein Transport
Quinine is a substrate for and an inhibitor of P-glycoprotein, and has the potential to affect transport of drugs that are P-glycoprotein substrates.
Specific Drugs and Laboratory Tests
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids (aluminum-and/or magnesium-containing) |
Delayed or decreased absorption of quinine |
Avoid concomitant use |
|
Antiarrhythmic agents (amiodarone, disopyramide, dofetilide, quinidine, procainamide, sotalol) |
Possible additive effect on QT interval |
Concomitant use not recommended |
|
Anticoagulants (heparin) |
Possible interference with the anticoagulant effects of heparin |
|
|
Anticoagulants (oral) (e.g., warfarin) |
Quinine may potentiate the anticoagulant effects of warfarin and other oral anticoagulants by depressing hepatic synthesis of vitamin K-dependent coagulation factors |
Closely monitor PT, PTT, or INR as indicated |
|
Anticonvulsants |
Carbamazepine or phenobarbital: Increased peak plasma concentrations and AUC of the anticonvulsant; possible decreased plasma quinine concentrations Phenytoin: No effect on pharmacokinetics of the anticonvulsant; possible decreased plasma quinine concentrations |
Carbamazepine or phenobarbital: If concomitant use with quinine cannot be avoided, frequently monitor serum concentrations of the anticonvulsant and monitor closely for anticonvulsant adverse effects |
|
Cholestyramine |
No effect on quinine pharmacokinetics |
|
|
Cigarette smoking |
Decreased quinine AUC and peak plasma concentration when used in malaria patients who were heavy smokers; greater effect on quinine pharmacokinetics reported when the drug was given to healthy adults who were heavy smokers Smoking does not appear to influence the therapeutic outcome in malaria patients treated with quinine |
Manufacturer of quinine suggests that reduced clearance of quinine in patients with acute malaria (see Elimination under Pharmacokinetics) may diminish the metabolic induction effect of smoking on quinine pharmacokinetics Manufacturer states that increased quinine dosage not necessary when treating acute malaria in heavy cigarette smokers |
|
Desipramine |
Decreased metabolism of desipramine in patients who are extensive CYP2D6 metabolizers; no effect in patients who are poor CYP2D6 metabolizers |
Monitor closely for adverse effects if quinine used concomitantly with desipramine |
|
Digoxin |
Increased digoxin AUC and decreased biliary clearance of digoxin |
Closely monitor digoxin plasma concentrations; adjust digoxin dosage as necessary |
|
Grapefruit juice |
No evidence of effect on quinine pharmacokinetics |
Quinine may be taken with grapefruit juice |
|
Histamine H2-receptor antagonists (cimetidine, ranitidine) |
Cimetidine: Decreased quinine clearance and prolonged quinine half-life Ranitidine: No effect on quinine pharmacokinetics |
Cimetidine: Monitor closely for adverse effects associated with quinine; if a pharmacokinetic interaction suspected, assess patient’s clinical status and adjust quinine dosage as needed or substitute a different histamine H2-receptor antagonist (e.g., ranitidine) Ranitidine: May be preferred when a histamine H2-receptor antagonist indicated in a patient receiving quinine |
|
HMG-CoA reductase inhibitors |
Atorvastatin: Possible increased plasma atorvastatin concentrations and increased risk of myopathy or rhabdomyolysis; rhabdomyolysis with acute renal failure secondary to myoglobinuria reported rarely |
Carefully weigh benefits and risks if considering concomitant use of quinine and atorvastatin or other HMG-CoA reductase inhibitors that are CYP3A4 substrates (e.g., simvastatin, lovastatin) If used concomitantly, consider lower starting and maintenance dosages of the HMG-CoA reductase inhibitor and monitor closely for signs or symptoms of muscle pain, tenderness, or weakness, especially during initial therapy Discontinue the HMG-CoA reductase inhibitor if CPK concentrations are markedly elevated or if myopathy (defined as muscle aches or weakness in conjunction with CPK concentrations >10 times the ULN) diagnosed or suspected |
|
Isoniazid |
No clinically important effect on pharmacokinetics of quinine |
Quinine dosage adjustment not required |
|
Ketoconazole |
Increased quinine AUC and decreased quinine clearance |
Quinine dosage adjustment not required; monitor closely for adverse effects associated with quinine |
|
Macrolides |
Possible increased plasma quinine concentrations; although causal relationship not established, fatal torsades de pointes reported in a geriatric patient who was receiving concomitant therapy with quinine, erythromycin, and dopamine |
Avoid concomitant use |
|
Mefloquine |
Potential additive cardiac effects; ECG abnormalities, including QT interval prolongation, may occur; increased risk for torsades de pointes or other serious ventricular arrhythmias Possible increased risk of seizures |
Do not use concomitantly; use sequentially with caution Because mefloquine has long serum half-life (up to 4 weeks), use caution if initiating quinine for treatment of malaria in patients who were receiving mefloquine for prophylaxis If quinine used for initial treatment of severe malaria, do not initiate mefloquine for follow-up treatment until ≥12 hours after last quinine dose |
|
Midazolam |
Does not affect metabolism of midazolam |
|
|
Neuromuscular blocking agents |
Pancuronium: Potentiated neuromuscular blockade (e.g., respiratory depression, apnea) reported Succinylcholine or tubocurarine (not commercially available in the US): Possibility of potentiated neuromuscular blockade |
Avoid use of neuromuscular blocking agents in patients receiving quinine |
|
Nevirapine |
Concomitant use decreases AUC, peak plasma concentration, and elimination half-life of quinine and increases AUC and peak plasma concentration of 3-hydroxyquinine, the major metabolite of quinine |
Adjustment of quinine dosage may be necessary in patients receiving nevirapine |
|
Oral contraceptives |
Quinine pharmacokinetics not affected by concomitant oral contraceptive therapy (progestin alone or estrogen in combination with progestin) |
|
|
Rifampin |
Decreased quinine AUC and plasma concentrations; quinine treatment failure may occur |
Avoid concomitant use |
|
Ritonavir |
Concomitant use increases quinine peak plasma concentration, AUC, and half-life; no clinically important effects on ritonavir pharmacokinetics |
Avoid concomitant use; if used concomitantly, quinine dosage may need to be reduced |
|
Tests, urinary corticosteroids or catecholamines |
Quinine causes falsely elevated results when a modification of the Reddy-Jenkins-Thorn procedure is used for urinary 17-hydroxycorticosteroids or when the Zimmermann method is used for urinary 17-ketogenic steroids; no effect on modified Porter-Silber method Quinine interferes with the Sobel and Henry modification of the trihydroxyindole method for determining urinary catecholamines, resulting in falsely increased concentrations |
|
|
Tetracyclines |
Increased quinine plasma concentrations |
Closely monitor for adverse effects associated with quinine |
|
Theophylline or aminophylline |
Possible decreased plasma theophylline concentrations and reduced effects of theophylline or aminophylline Possible increased plasma quinine concentrations |
Monitor plasma theophylline concentrations frequently Quinine dosage adjustment not needed; closely monitor for quinine adverse effects |
|
Urinary alkalizers |
Agents that increase urinary pH (e.g., acetazolamide, sodium bicarbonate) may increase plasma quinine concentrations |
quiNINE Pharmacokinetics
Absorption
Bioavailability
Oral bioavailability is 76–88% in healthy adults. Quinine exposure higher in patients with malaria than in healthy adults, possibly because malaria may cause impaired hepatic function, which results in decreased quinine total body clearance and volume of distribution.
In adults with uncomplicated P. falciparum malaria, mean AUC and peak plasma concentrations higher and time to peak concentration longer than that reported in healthy adults. Following a single oral dose, mean time to peak serum concentrations is 5.9 hours in adults with uncomplicated P. falciparum malaria compared with 2.8 hours in healthy adults.
Food
When a single 324-mg dose of oral quinine sulfate capsules was administered with a high-fat meal in healthy adults, the time to peak concentrations was prolonged to approximately 4 hours; however, mean peak plasma concentration and AUC from 0–24 hours were similar to those achieved following oral administration of the drug under fasted conditions.
Special Populations
Pharmacokinetics in children 1.5–12 years of age with uncomplicated P. falciparum malaria appear to be similar to that observed in adults with uncomplicated malaria. Following a single dose of 10 mg/kg of oral quinine sulfate in healthy children or children 1.5–12 years of age with uncomplicated P. falciparum malaria, mean time to peak quinine concentration was longer (4 versus 2 hours) and mean peak plasma concentration was higher (7.5 versus 3.4 mcg/mL) in children with uncomplicated P. falciparum malaria than in healthy children.
Following a single 600-mg dose of oral quinine sulfate, mean AUC in healthy geriatric adults 65–78 years of age is approximately 38% higher than in younger adults 20–35 years of age; mean time to peak quinine concentrations and mean peak plasma concentrations are similar in both age groups.
Following a single 600-mg dose of oral quinine sulfate in adults with severe chronic renal failure not receiving any form of dialysis (mean serum creatinine 9.6 mg/dL), median AUC and mean peak plasma concentration increased by 195 and 79%, respectively, compared with adults with normal renal function. Effect of mild or moderate renal impairment on pharmacokinetics of quinine sulfate not determined to date.
Following a single 600-mg oral dose of quinine sulfate in otherwise healthy adults with moderate hepatic impairment (Child-Pugh class B), mean AUC increased 55% compared with healthy adults with normal hepatic function; mean peak plasma concentrations similar in both groups. Quinine absorption prolonged in adults with hepatitis. Pharmacokinetic data not available to date for patients with severe hepatic impairment (Child-Pugh class C).
Distribution
Extent
Volume of distribution lower in patients with malaria than in healthy individuals or patients convalescing from malaria. Volume of distribution decreases with increasing severity of malarial infection.
Intra-erythrocytic quinine concentrations are approximately 30–50% of plasma concentrations. Small amounts distributed into bile and saliva.
Penetrates relatively poorly into CSF in patients with cerebral malaria; CSF quinine concentrations reported to be 2–7% of concurrent plasma concentrations.
Readily crosses the placenta. In a small number of women who delivered live infants 1–6 days after starting quinine therapy, placental cord plasma quinine concentrations were 1–4.6 mg/L (mean: 2.4 mg/L) and mean ratio of cord plasma to maternal plasma quinine concentrations was 0.32. Such placental cord concentrations may not result in therapeutic fetal plasma quinine concentrations.
Distributed into milk.
Plasma Protein Binding
Approximately 69–92% in healthy adults.
During active malarial infection, protein binding increased to 78–95%, which correlates with increases in α-1-acid glycoprotein that occur during malarial infection. In one study, quinine was approximately 93% bound to plasma proteins in patients with cerebral malaria and approximately 90% bound in patients with uncomplicated malaria or in patients convalescing from the disease.
Elimination
Metabolism
Metabolized almost exclusively via hepatic oxidative (CYP) pathways into 4 primary metabolites (3-hydroxyquinine, 2′-quinone, O-desmethylquinine, and 10,11-dihydroxydihydroquinine) and 6 secondary metabolites resulting from further biotransformation of the primary metabolites.
The major metabolite, 3-hydroxyquinine, is less active than parent drug.
In vitro studies indicate quinine is metabolized principally by CYP3A4 and may also be metabolized by other CYP enzymes, including 1A2, 2C8, 2C9, 2C19, 2D6, and 2E1.
Elimination Route
Approximately 20% of a dose excreted unchanged in urine. Reabsorption of quinine is increased when urine is alkaline; rate of renal excretion of the drug is doubled when urine is acidic compared with when urine is alkaline.
Negligible to minimal amounts removed by hemodialysis or hemofiltration.
Half-life
Adults: 8–21 hours in those with malaria and 7–12 hours in those who are healthy or convalescing from the disease.
Children 1–12 years of age: 11–12 hours in those with malaria and 6 hours in those convalescing from the disease.
Geriatric adults: Mean elimination half-life after single dose is increased to 18.4 hours. At steady-state, mean elimination half-life is 24 hours in geriatric adults compared with 20 hours in younger adults. Although renal clearance of quinine is similar in geriatric and younger adults, geriatric adults excrete a larger proportion of the dose in urine as unchanged drug compared with younger adults.
Special Populations
Plasma concentrations are higher and plasma half-life may be prolonged in patients with malaria.
Adults with hepatitis: Elimination half-life and apparent volume of distribution are increased, but weight-adjusted clearance not altered.
Otherwise healthy individuals with mild hepatic impairment (Child-Pugh class A): Quinine pharmacokinetics and exposure to 3-hydroxyquinine are similar to that in healthy individuals with normal hepatic function.
Individuals with severe hepatic impairment (Child-Pugh class C): Oral clearance of quinine and formation of 3-hydroxyquinine decreased; volume of distribution and plasma elimination half-life increased.
Adults with severe chronic renal failure: Mean plasma half-life prolonged to 26 hours. Effects of mild and moderate renal impairment on pharmacokinetics and safety not determined to date.
Stability
Storage
Oral
Capsules
20–25°C in tight, light-resistant container. Drug darkens on exposure to light.
Actions and Spectrum
-
An alkaloid obtained from the bark of the cinchona tree; the levorotatory isomer of quinidine.
-
Has several effects on skeletal muscle. Increases the refractory period of muscle by a direct action on muscle fiber so that the response to tetanic stimulation is diminished; has a curare-like effect and decreases the excitability of the motor endplate so that responses to repetitive nerve stimulation or acetylcholine are reduced; and affects the distribution of calcium within muscle fiber.
-
Has cardiovascular effects similar to those of quinidine.
-
Exact mechanism of antimalarial activity not determined. Inhibits nucleic acid synthesis, protein synthesis, and glycolysis in P. falciparum and can bind with hemazoin in parasitized erythrocytes.
-
A blood schizonticidal agent active against the asexual erythrocytic forms of P. falciparum, P. malariae, P. ovale, and P. vivax. Not gametocidal against P. falciparum. Inactive against sporozoites or pre-erythrocytic or exoerythrocytic forms of plasmodia.
-
P. falciparum malaria clinically resistant to quinine has been reported in some areas of South America, Southeast Asia, and Bangladesh. Strains of P. falciparum with decreased susceptibility to quinine also can be selected in vivo.
-
Cross-resistance has been reported between mefloquine and quinine. Although cross-resistance has been demonstrated rarely between quinine and 4-aminoquinoline derivatives, quinine may be active against some strains of P. falciparum resistant to chloroquine.
Advice to Patients
-
Importance of taking the drug exactly as prescribed. Advise patients not to double the next dose if a dose is missed; if >4 hours has elapsed since the missed dose, patient should not take the missed dose and should take the next dose as previously scheduled.
-
Importance of taking with food to minimize possible GI irritation.
-
Importance of immediately contacting a clinician if malarial symptoms worsen or do not improve within 2 days of initiating quinine therapy or if fever recurs following completion of antimalarial therapy.
-
Importance of immediately contacting a clinician if symptoms of hypersensitivity (e.g., rash, hives, severe itching, severe flushing, facial swelling, difficulty breathing), bleeding (e.g., easy bruising, severe nose bleed, bleeding gums, blood in urine or stool, unusual purple, brown, or red skin spots indicating bleeding under the skin), or heart problems (e.g., chest pain, rapid heartbeat, irregular heart rhythm, weakness, sweating, nervousness) occur.
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
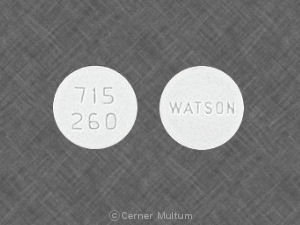
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
324 mg |
Qualaquin |
AR Scientific |
|
Quinine Sulfate Capsules |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions March 5, 2014. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about quinine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (20)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: antimalarial quinolines
- Breastfeeding
- En español