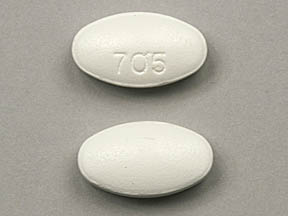
norfloxacin
Generic name: norfloxacin (oral) [ nor-FLOX-a-sin ]
Brand name: Noroxin
Drug class: Quinolones and fluoroquinolones
What is norfloxacin?
Norfloxacin is an antibiotic in a group of drugs called fluoroquinolones (flor-o-KWIN-o-lones). Norfloxacin fights bacteria in the body.
Norfloxacin is used to treat different bacterial infections of the prostate or urinary tract (bladder and kidneys). Norfloxacin is also used to treat gonorrhea.
Norfloxacin may also be used for purposes not listed in this medication guide.
What is the most important information I should know about norfloxacin?
You should not use this medication if you have ever had swelling or tearing of a tendon caused by taking norfloxacin or similar antibiotics.
You may not be able to use norfloxacin if you have a muscle disorder. Tell your doctor if you have a history of myasthenia gravis.
Norfloxacin may cause swelling or tearing of a tendon (the fiber that connects bones to muscles in the body), especially in the Achilles' tendon of the heel. This effect may be more likely to occur if you are over 60, if you take steroid medication, or if you have had a kidney, heart, or lung transplant.
Stop taking norfloxacin and call your doctor at once if you have sudden pain, swelling, bruising, tenderness, stiffness, or movement problems in any of your joints. Rest the joint until you receive medical care or instructions.
What should I discuss with my healthcare provider before taking norfloxacin?
You should not use this medication if you are allergic to norfloxacin, or if:
-
you have ever had swelling or tearing of a tendon caused by taking norfloxacin or similar antibiotics; or
-
you are allergic to other fluoroquinolones (ciprofloxacin, gemifloxacin, levofloxacin, moxifloxacin, ofloxacin, and others).
You may not be able to use norfloxacin if you have a muscle disorder. Tell your doctor if you have a history of myasthenia gravis.
To make sure norfloxacin is safe for you, tell your doctor if you have:
-
a heart rhythm disorder, especially if you take medication to treat it;
-
slow heartbeats, or a personal or family history of Long QT syndrome;
-
tendon problems, arthritis or other joint problems;
-
a muscle or nerve disorder;
-
kidney or liver disease;
-
seizures or epilepsy;
-
a history of head injury or brain tumor;
-
a history of allergic reaction to an antibiotic;
-
diabetes (especially if you take oral diabetes medication);
-
low levels of potassium in your blood (hypokalemia); or
-
if you use a blood thinner (warfarin, Coumadin) and have "INR" or prothrombin time tests.
Norfloxacin may cause swelling or tearing of a tendon (the fiber that connects bones to muscles in the body), especially in the Achilles' tendon of the heel. This can happen during treatment or up to several months after you stop taking norfloxacin. Tendon problems may be more likely to occur if you are over 60, if you take steroid medication, or if you have had a kidney, heart, or lung transplant.
FDA pregnancy category C. It is not known whether norfloxacin will harm an unborn baby. Tell your doctor if you are pregnant or plan to become pregnant while using this medication.
It is not known whether norfloxacin passes into breast milk or if it could harm a nursing baby. You should not breast-feed while using this medicine.
How should I take norfloxacin?
Norfloxacin is usually taken every 12 hours. Follow all directions on your prescription label. Do not take this medicine in larger or smaller amounts or for longer than recommended.
Take this medicine with a full glass of water (8 ounces). Drink several extra glasses of fluid each day while you are taking norfloxacin.
Take norfloxacin on an empty stomach 1 hour before or 2 hours after eating a meal, drinking milk, or eating a dairy product such as yogurt.
Use this medication for the full prescribed length of time. Your symptoms may improve before the infection is completely cleared. Skipping doses may also increase your risk of further infection that is resistant to antibiotics. Norfloxacin will not treat a viral infection such as the common cold or flu.
If you are being treated for gonorrhea, your doctor may also have you tested for syphilis, another sexually transmitted disease.
Do not share this medication with another person (especially a child), even if they have the same symptoms you have.
Store at room temperature away from moisture and heat.
What happens if I miss a dose?
Take the missed dose as soon as you remember. Skip the missed dose if it is almost time for your next scheduled dose. Do not take extra medicine to make up the missed dose.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while taking norfloxacin?
You may be taking certain other medicines that should not be taken at the same time as norfloxacin. Avoid taking the following medicines within 2 hours before or after you take norfloxacin. These other medicines can make norfloxacin much less effective when taken at the same time:
-
antacids that contain magnesium or aluminum (such as Maalox, Mylanta, or Rolaids), or the ulcer medicine sucralfate (Carafate);
-
didanosine (Videx) powder or chewable tablets;
-
vitamin or mineral supplements that contain iron or zinc.
Do not take norfloxacin with dairy products such as milk or yogurt. They could make the medication less effective.
Avoid caffeine while you are taking norfloxacin, because the medication can make the effects of caffeine stronger.
Avoid exposure to sunlight or tanning beds. Norfloxacin can make you sunburn more easily. Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors. Call your doctor if you have severe burning, redness, itching, rash, or swelling after being in the sun.
Antibiotic medicines can cause diarrhea, which may be a sign of a new infection. If you have diarrhea that is watery or bloody, stop taking norfloxacin and call your doctor. Do not use anti-diarrhea medicine unless your doctor tells you to.
Norfloxacin may impair your thinking or reactions. Be careful if you drive or do anything that requires you to be alert.
Norfloxacin side effects
Get emergency medical help if you have any of these signs of an allergic reaction: hives, or the first sign of a skin rash; fast heartbeat, difficult breathing; swelling of your face, lips, tongue, or throat.
Norfloxacin may cause swelling or tearing of (rupture) a tendon. Norfloxacin can also have serious effects on your nerves, and may cause permanent nerve damage. Stop taking this medicine and call your doctor at once if you have:
-
signs of tendon rupture--sudden pain, swelling, bruising, tenderness, stiffness, movement problems, or a snapping or popping sound in any of your joints (rest the joint until you receive medical care or instructions); or
-
nerve symptoms--numbness, tingling, burning pain, or being more sensitive to temperature, light touch, or the sense of your body position.
Stop using norfloxacin and call your doctor at once if you have:
-
headache with chest pain and severe dizziness, fainting, fast or pounding heartbeats;
-
dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes);
-
muscle weakness or trouble breathing;
-
diarrhea that is watery or bloody;
-
sudden weakness or ill feeling, fever, chills, sore throat, mouth sores, easy bruising or bleeding;
-
depression, confusion, hallucinations, paranoia, tremors, feeling restless or anxious, unusual thoughts or behavior, insomnia, nightmares;
-
seizure (convulsions); or
-
increased pressure inside the skull-- severe headaches, ringing in your ears, dizziness, nausea, vision problems, pain behind your eyes.
Common side effects may include:
-
nausea, heartburn, stomach cramps, mild diarrhea;
-
vaginal itching or discharge;
-
mild dizziness; or
-
mild headache.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
Norfloxacin dosing information
Usual Adult Dose for Urinary Tract Infection:
Uncomplicated:
Due to Escherichia coli, Klebsiella pneumoniae, or Proteus mirabilis: 400 mg orally every 12 hours for 3 days
Due to other organisms: 400 mg orally every 12 hours for 7 to 10 days
Complicated: 400 mg orally every 12 hours for 10 to 21 days
Usual Adult Dose for Cystitis:
Due to E coli, K pneumoniae, or P mirabilis: 400 mg orally every 12 hours for 3 days
Due to other organisms: 400 mg orally every 12 hours for 7 to 10 days
Usual Adult Dose for Prostatitis:
Acute or chronic: 400 mg orally every 12 hours for 28 days
Usual Adult Dose for Gonococcal Infection -- Uncomplicated:
800 mg orally one time
Due to high rates of resistance, the Centers for Disease Control and Prevention do not recommend fluoroquinolones for treatment of gonococcal infections in the United States. Ceftriaxone or oral cefixime is recommended as first-line treatment of gonorrhea in the United States. Antimicrobial susceptibility patterns should be monitored.
Doxycycline therapy for 7 days (if not pregnant) or single-dose azithromycin is also recommended for possible coexisting chlamydial infection.
The patient's sexual partner(s) should also be evaluated/treated.
Usual Adult Dose for Campylobacter Gastroenteritis:
(Not approved by FDA)
400 mg orally every 12 hours for 3 days
Immunocompromised patients may require therapy for 7 to 14 days.
Usual Adult Dose for Epididymitis -- Non-Specific:
(Not approved by FDA)
Nonsexually transmitted: 400 mg orally every 12 hours for 14 days
Usual Adult Dose for Pyelonephritis:
(Not approved by FDA)
Mild infections: 400 mg orally every 12 hours for 14 days
Usual Adult Dose for Salmonella Enteric Fever:
(Not approved by FDA)
400 mg orally every 12 hours for 7 to 14 days
Usual Adult Dose for Salmonella Gastroenteritis:
(Not approved by FDA)
400 mg orally every 12 hours for 5 days; however, most cases are self-limiting and prudent withholding of antibiotic therapy does not appear to slow recovery
Immunocompromised patients may require therapy for 14 days.
Usual Adult Dose for Shigellosis:
(Not approved by FDA)
400 mg orally every 12 hours for 5 days
Immunocompromised patients may require therapy for 7 to 10 days.
Usual Adult Dose for Traveler's Diarrhea:
(Not approved by FDA)
400 mg orally every 12 hours for 3 days; however, most cases are self-limiting and prudent withholding of antibiotic therapy does not appear to slow recovery
Immunocompromised patients may require therapy for 7 to 14 days.
What other drugs will affect norfloxacin?
Tell your doctor about all medicines you use, and those you start or stop using during your treatment with norfloxacin, especially:
-
cisapride, cyclosporine, erythromycin, nitrofurantoin, probenecid, ropinirole, tacrine, theophylline, tizanidine;
-
a diuretic or "water pill";
-
heart rhythm medication--amiodarone, disopyramide, dofetilide, dronedarone, procainamide, quinidine, sotalol, and others;
-
medicine to treat depression or mental illness--amitriptylline, clomipramine, clozapine, desipramine, duloxetine, iloperidone, imipramine, nortriptyline, thioridazine, ziprasidone, and others; or
-
NSAIDs (nonsteroidal anti-inflammatory drugs)--aspirin, ibuprofen (Advil, Motrin), naproxen (Aleve), celecoxib, diclofenac, indomethacin, meloxicam, and others.
This list is not complete. Other drugs may interact with norfloxacin, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed in this medication guide.
More about norfloxacin
- Check interactions
- Compare alternatives
- Reviews (5)
- Side effects
- Dosage information
- During pregnancy
- Drug class: quinolones and fluoroquinolones
- Breastfeeding
Patient resources
Other brands
Related treatment guides
Further information
Remember, keep this and all other medicines out of the reach of children, never share your medicines with others, and use this medication only for the indication prescribed.
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Copyright 1996-2024 Cerner Multum, Inc. Version: 12.02. Revision Date: 2014-04-13, 8:21:55 PM.