Emtricitabine and Tenofovir Disoproxil Fumarate (Monograph)
Drug class: HIV Nucleoside and Nucleotide Reverse Transcriptase Inhibitors
VA class: AM800
Chemical name: 5-Fluoro-1-(2R, 5S)-[2-(hydroxymethyl)-1,3-oxathiolan-5-yl] cytosine
Molecular formula: C8H10FN3O3S C23H34N5O14P
CAS number: 143491-57-0
Emtricitabine and Tenofovir Disoproxil Fumarate is also contained as an ingredient in the following combinations:
Emtricitabine and Tenofovir Disoproxil Fumarate
Warning
- HBV Infection
-
Severe, acute exacerbations of HBV reported following discontinuance of emtricitabine and tenofovir disoproxil fumarate (emtricitabine/tenofovir DF; FTC/TDF) in patients infected with HBV.1
-
Monitor hepatic function closely with both clinical and laboratory follow-up for at least several months after FTC/TDF is discontinued in HBV-infected patients.1 If clinically appropriate, initiate HBV treatment.1
- HIV-1 Preexposure Prophylaxis (PrEP)
-
Prescribe FTC/TDF for HIV-1 PrEP only for individuals confirmed to be HIV-1-negative immediately prior to initiation of PrEP; confirm HIV-1-negative status periodically (at least every 3 months) during PrEP.1
-
Drug-resistant HIV-1 variants have been identified when FTC/TDF PrEP was used following undetected acute HIV-1 infection.1 Do not initiate FTC/TDF PrEP if signs or symptoms of acute HIV-1 infection are present, unless negative infection status is confirmed.1
Introduction
Antiretroviral; fixed combination of emtricitabine and tenofovir disoproxil fumarate (FTC/TDF).1 Emtricitabine (FTC) is an HIV nucleoside reverse transcriptase inhibitor (NRTI), and tenofovir disoproxil fumarate (TDF) is an HIV nucleotide reverse transcriptase inhibitor.1
Uses for Emtricitabine and Tenofovir Disoproxil Fumarate
Treatment of HIV Infection
Treatment of HIV-1 infection in adults and pediatric patients weighing ≥17 kg;1 200 201 202 must use in conjunction with other antiretrovirals.1 200 201 202
Dual NRTIs used in conjunction with an HIV integrase strand transfer inhibitor (INSTI), HIV nonnucleoside reverse transcriptase inhibitor (NNRTI), or HIV protease inhibitor (PI) in INSTI-, NNRTI-, or PI-based regimens.200 201 Fixed combinations used in certain patient groups to decrease pill burden and improve compliance.200 201
For initial treatment in HIV-infected adults and adolescents, experts state that FTC/TDF is a recommended dual NRTI option for use in most INSTI-, NNRTI-, and PI-based regimens.200
For initial treatment in antiretroviral-naive pediatric patients, experts state that FTC/TDF is an alternative dual NRTI option for use in children 2–12 years of age and a preferred dual NRTI option in adolescents ≥12 years of age with SMR 4 or 5.200 201
Also may be used as part of a combination antiretroviral regimen in previously treated patients;1 200 select antiretrovirals in new regimen for patients who are experiencing treatment failure based on antiretroviral treatment history and results from current and past resistance testing.200
Because both drugs have activity against both HIV and HBV, FTC/TDF is a preferred dual NRTI option for antiretroviral regimens in HIV-infected patients coinfected with HBV.200
Most appropriate antiretroviral regimen cannot be defined for every clinical scenario; select regimen based on information regarding antiretroviral potency, potential rate of resistance development, known toxicities, potential for pharmacokinetic interactions, and patient's virologic, immunologic, and clinical characteristics.200 201 202 Guidelines for the management of HIV infection, including specific recommendations for initial treatment in antiretroviral-naive patients and recommendations for changing antiretroviral regimens, are available at [Web].200 201 202
Preexposure Prophylaxis for Prevention of HIV-1 Infection (PrEP)
FTC/TDF used for PrEP in conjunction with safer sex practices to reduce the risk of sexually acquired HIV-1 in HIV-1-negative at-risk adults and adolescents weighing ≥35 kg.1 197 450 457 463
Adults and adolescents at risk include those with partner(s) known to be infected with HIV-1 or those engaging in sexual activity within a high prevalence area or social network and with ≥1 of the following factors: inconsistent or no condom use, past or current sexually transmitted infections, use of illicit drugs, alcohol dependence, or partner(s) of unknown HIV-1 status.1 197
PrEP with FTC/TDF not always effective in preventing acquisition of HIV-1 infection; must be used as part of a comprehensive prevention strategy that includes safer sex practices.1
Postexposure Prophylaxis following Occupational Exposure to HIV (PEP)
Postexposure prophylaxis of HIV infection following occupational exposure† [off-label] (PEP) in health-care personnel and others exposed via percutaneous injury (e.g., needlestick, cut with sharp object) or mucous membrane or nonintact skin (e.g., chapped, abraded, dermatitis) contact with blood, tissue, or other body fluids that might contain HIV.199 Used in conjunction with other antiretrovirals.199
USPHS recommends 3-drug regimen of raltegravir in conjunction with FTC and TDF as the preferred regimen for PEP following occupational exposures to HIV.199 Several alternative regimens that include an INSTI, NNRTI, or PI and 2 NRTIs (dual NRTIs) also recommended.199 Preferred dual NRTI option for PEP regimens is FTC and TDF (may be given as FTC/TDF fixed combination);199 alternative dual NRTI options are TDF and lamivudine, lamivudine and zidovudine (may be given as lamivudine/zidovudine; Combivir), or zidovudine and emtricitabine.199
Management of occupational exposures to HIV is complex and evolving;199 consult infectious disease specialist, clinician with expertise in administration of antiretroviral agents, and/or National Clinicians’ Postexposure Prophylaxis Hotline (PEPline at 888-448-4911) whenever possible.199 Do not delay initiation of PEP while waiting for expert consultation.199
Postexposure Prophylaxis following Nonoccupational Exposure to HIV (nPEP)
Postexposure prophylaxis of HIV infection following nonoccupational exposure† [off-label] (nPEP) in individuals exposed to blood, genital secretions, or other potentially infectious body fluids that might contain HIV when the exposure represents a substantial risk for HIV transmission.198 Used in conjunction with other antiretrovirals.198
When nPEP indicated in adults and adolescents ≥13 years of age with normal renal function, CDC states preferred regimen is either raltegravir or dolutegravir used in conjunction with FTC/TDF;198 alternative regimen recommended in these patients is ritonavir-boosted darunavir used in conjunction with FTC/TDF.198
Consult infectious disease specialist, clinician with expertise in administration of antiretroviral agents, and/or the National Clinicians’ Postexposure Prophylaxis Hotline (PEPline at 888-448-4911) if nPEP indicated in certain exposed individuals (e.g., pregnant women, children, those with medical conditions such as renal impairment) or if considering a regimen not included in CDC guidelines, source virus is known or likely to be resistant to antiretrovirals, or healthcare provider is inexperienced in prescribing antiretrovirals.198 Do not delay initiation of nPEP while waiting for expert consultation.198
Emtricitabine and Tenofovir Disoproxil Fumarate Dosage and Administration
General
Pretreatment Screening
-
Prior to or when initiating FTC/TDF, test patients for HBV infection.1
-
Prior to initiation of FTC/TDF, assess Scr, estimated Clcr, urine glucose, and urine protein in all patients; in patients with chronic kidney disease, also assess serum phosphorus.1
-
Immediately prior to initiating FTC/TDF for HIV-1 PrEP, screen for HIV-1 infection.1 If recent (<1 month) exposures to HIV-1 are suspected or clinical symptoms consistent with acute HIV-1 infection are present, use a test approved or cleared by the FDA as an aid in the diagnosis of acute or primary HIV-1 infection.1
Patient Monitoring
-
Monitor hepatic function closely with clinical and laboratory follow-up for at least several months after discontinuance of FTC/TDF in patients infected with HBV.1
-
On a clinically appropriate schedule, assess Scr, estimated Clcr, urine glucose, and urine protein in all patients; in patients with chronic kidney disease, also assess serum phosphorus.1
-
In patients receiving FTC/TDF for PrEP, screen for HIV-1 infection at least once every 3 months and upon diagnosis of any other sexually transmitted infections.1
-
Consider bone mineral density (BMD) monitoring in adult and pediatric patients who have a history of pathologic bone fracture or other risk factors for osteoporosis or bone loss.1
Administration
Oral Administration
Administer fixed combination of FTC/TDF orally once daily without regard to food.1
Use in conjunction with other antiretrovirals for treatment of HIV-1;1 use alone as a complete regimen for PrEP for prevention of sexually transmitted HIV-1.1 197
Dosage
FTC/TDF tablets contain emtricitabine and tenofovir DF; dosage of tenofovir DF expressed in terms of tenofovir DF.1
Pediatric Patients
Treatment of HIV Infection
Oral
Children weighing ≥35 kg: 1 tablet containing FTC 200 mg and TDF 300 mg once daily.1
Children weighing 17 to <35 kg: Base dosage on weight and use a low-strength fixed-combination tablet.1 (See Table 1.) Monitor weight periodically and adjust dosage of FTC/TDF accordingly.1
|
Weight (kg) |
Dosage of Emtricitabine/Tenofovir DF given Once Daily |
|---|---|
|
17 to <22 kg |
1 tablet (emtricitabine 100 mg and tenofovir DF 150 mg) |
|
22 to <28 kg |
1 tablet (emtricitabine 133 mg and tenofovir DF 200 mg) |
|
28 to <35 kg |
1 tablet (emtricitabine 167 mg and tenofovir DF 250 mg) |
|
≥35 kg |
1 tablet (emtricitabine 200 mg and tenofovir DF 300 mg) |
Preexposure Prophylaxis for Prevention of HIV-1 Infection (PrEP)
HIV-1-negative Adolescents at Risk
OralAdolescents weighing ≥35 kg: 1 tablet containing FTC 200 mg and TDF 300 mg once daily.1
Adults
Treatment of HIV Infection
Oral
1 tablet containing FTC 200 mg and TDF 300 mg once daily.1
Preexposure Prophylaxis for Prevention of HIV-1 Infection (PrEP)
HIV-1-negative Adults at Risk
Oral1 tablet containing FTC 200 mg and TDF 300 mg once daily.1
Postexposure Prophylaxis following Occupational Exposure to HIV (PEP)† [off-label]
Oral
1 tablet containing FTC 200 mg and TDF 300 mg once daily.199 Use in conjunction with a recommended INSTI, NNRTI, or PI.199
Initiate PEP as soon as possible following occupational exposure to HIV (preferably within hours); continue for 4 weeks, if tolerated.199
Postexposure Prophylaxis following Nonoccupational Exposure to HIV (nPEP)† [off-label]
Oral
1 tablet containing FTC 200 mg and TDF 300 mg once daily.198 Use in conjunction with a preferred or alternative INSTI, NNRTI, or PI.198
Initiate nPEP as soon as possible (within 72 hours) following nonoccupational exposure that represents a substantial risk for HIV transmission and continue for 28 days.198
nPEP not recommended if exposed individual seeks care >72 hours after exposure.198
Special Populations
Hepatic Impairment
Treatment of HIV Infection
FTC not substantially metabolized by liver enzymes; not specifically studied, but clinically important changes in metabolism not expected in patients with hepatic impairment.1
No change in tenofovir pharmacokinetics were observed in patients with moderate to severe hepatic impairment receiving a 300-mg dose of TDF.1
FTC/TDF: Not studied in hepatic impairment.1
Renal Impairment
Treatment of HIV Infection
Adults with Clcr 50–80 mL/minute: Use usual dosage.1
Adults with Clcr 30–49 mL/minute: Reduce dosage to 1 tablet (FTC 200 mg and TDF 300 mg) once every 48 hours; monitor clinical response and renal function since dosage not evaluated clinically.1
Adults with Clcr <30 mL/minute (including hemodialysis patients): Do not use.1
Pediatric patients with renal impairment: Data insufficient to make dosage recommendations.1
Preexposure Prophylaxis for Prevention of HIV-1 Infection (PrEP)
Adults with Clcr ≥60 mL/minute: Use usual dosage.1
Adults with Clcr <60 mL/minute: Do not use.1
If Clcr decreases during use for PrEP, evaluate potential causes and reassess potential risks and benefits of continued use.1
Pediatric patients with renal impairment: Data insufficient to make dosage recommendations.1
Geriatric Patients
Specific dosage recommendations not available.1
Cautions for Emtricitabine and Tenofovir Disoproxil Fumarate
Contraindications
-
Do not use for PrEP of HIV-1 infection in individuals with unknown or positive HIV-1 status.1
Warnings/Precautions
Warnings
Individuals with HBV Infection
Test all patients for presence of HBV before initiating FTC/TDF.1
Severe acute exacerbations of HBV reported following discontinuance of FTC/TDF in HBV-infected patients.1 HBV exacerbations have been associated with hepatic decompensation and hepatic failure.1
Offer HBV vaccination to HBV-uninfected individuals.1
Closely monitor hepatic function with both clinical and laboratory follow-up for at least several months after FTC/TDF is discontinued in HBV-infected patients.1 If clinically appropriate, initiate HBV treatment.1
FTC/TDF is not indicated for treatment of chronic HBV infection.1
Precautions Related to HIV-1 Preexposure Prophylaxis
Use FTC/TDF for HIV-1 PrEP only in adults or adolescents (≥35 kg) who are HIV-1-negative.1 Confirm a negative HIV-1 test immediately prior to initiating PrEP and screen for HIV-1 infection at least once every 3 months and upon diagnosis of any other sexually transmitted infection during PrEP.1
Drug-resistant HIV-1 variants have been identified when FTC/TDF PrEP was used following undetected acute HIV-1 infection.1 Do not initiate PrEP if signs or symptoms of acute HIV-1 infection are present, unless negative infection status is confirmed.1
Some HIV-1 tests only detect anti-HIV antibodies and may not identify HIV-1 during the acute stage of infection.1 Prior to initiating PrEP, evaluate HIV-negative individuals for current or recent signs or symptoms consistent with acute viral infections (e.g., fever, fatigue, myalgia, rash) and ask about any potential exposure events within the last month (e.g., unprotected sex, condom broke during sex with a partner of unknown HIV-1 status or unknown viremic status, a recent sexually transmitted infection).1
If recent (<1 month) exposures to HIV-1 are suspected or clinical symptoms consistent with acute HIV-1 infection are present, use a test approved or cleared by the FDA as an aid in the diagnosis of acute or primary HIV-1 infection.1
Time from initiation of FTC/TDF for HIV-1 PrEP to maximal protection against HIV-1 infection unknown.1
Counsel uninfected individuals to strictly adhere to recommended FTC/TDF dosage schedule.1 Effectiveness in reducing risk of acquiring HIV-1 is strongly correlated with adherence.1 Some individuals (e.g., adolescents) may benefit from more frequent visits and counseling to support adherence.1
Adverse effects similar to those reported in HIV-infected patients receiving the drugs for treatment of HIV-1 infection.1
Other Warnings/Precautions
Renal Impairment
Renal impairment, including cases of acute renal failure and Fanconi syndrome (renal tubular injury with severe hypophosphatemia), reported with use of TDF.1
Assess Scr, estimated Clcr, urine glucose, and urine protein prior to initiating FTC/TDF and monitor during treatment in all patients as clinically appropriate.1 In patients with chronic kidney disease, also assess serum phosphorus.1
In individuals at risk for renal dysfunction, evaluate renal function if possible manifestations of proximal renal tubulopathy (e.g., persistent or worsening bone pain, pain in extremities, fractures, muscular pain or weakness) occur.1
When used for treatment of HIV-1 infection, dosing interval adjustment of FTC/TDF and close monitoring of renal function are recommended in patients with estimated Clcr 30–49 mL/minute.1 No safety or efficacy data available in patients with renal impairment who received FTC/TDF using these dosing guidelines; assess potential benefit of FTC/TDF therapy against potential risk of renal toxicity.1 Use of FTC/TDF for treatment of HIV-1 infection not recommended in patients with estimated Clcr <30 mL/min or patients requiring hemodialysis.1
Use of FTC/TDF for PrEP not recommended in patients with estimated Clcr <60 mL/minute.1 If a decrease in estimated Clcr is observed while using FTC/TDF for HIV-1 PrEP, evaluate potential causes and reassess potential risks and benefits of continued use.1
Avoid FTC/TDF in patients with concurrent or recent use of a nephrotoxic agent (e.g., high-dose or multiple nonsteroidal anti-inflammatory agents [NSAIAs]).1 Cases of acute renal failure after initiation of high-dose or multiple NSAIAs reported in HIV-infected patients with risk factors for renal dysfunction who appeared stable on TDF; some patients required hospitalization and renal replacement therapy.1 Consider alternatives to NSAIAs, if needed, in patients at risk for renal dysfunction.1
Immune Reconstitution Syndrome
Immune reconstitution syndrome reported in HIV-infected patients receiving multiple-drug antiretroviral therapy, including FTC/TDF.1
During initial treatment, HIV-infected patients who respond to antiretroviral therapy may develop an inflammatory response to indolent or residual opportunistic infections (e.g., Mycobacterium avium complex [MAC], M. tuberculosis, cytomegalovirus [CMV], Pneumocystis jirovecii [formerly P. carinii]);1 this may necessitate further evaluation and treatment.1
Autoimmune disorders (e.g., Graves' disease, polymyositis, Guillain-Barré syndrome, autoimmune hepatitis) also reported in the setting of immune reconstitution;1 time to onset is more variable and can occur many months after initiation of antiretroviral therapy.1
Bone Loss and Mineralization Defects
Decreases in BMD from baseline, increases in several biochemical markers of bone metabolism, and increased serum parathyroid hormone levels and 1,25-vitamin D levels reported during clinical trials of TDF.1 Effects of tenofovir-associated changes in BMD on long-term bone health and future fracture risk unknown.1
In clinical trials in HIV-1 infected subjects 2 years of age to <18 years of age, bone effects in pediatric and adolescent subjects receiving TDF were similar to those observed in adult subjects, suggesting increased bone turnover.1 Total body BMD gain was less in the TDF-treated HIV-1 infected pediatric subjects compared with control groups.1 Similar trends observed in adolescent subjects 12 years of age to <18 years of age treated for chronic HBV infection.1 Skeletal growth (height) appeared unaffected in pediatric trials.1
Osteomalacia associated with proximal renal tubulopathy, which manifested as bone pain or pain in extremities and may contribute to fractures, reported in patients receiving TDF.1 Arthralgia and muscle pain or weakness also reported in patients with proximal renal tubulopathy.1 Consider hypophosphatemia and osteomalacia secondary to proximal renal tubulopathy in patients at risk for renal dysfunction who present with persistent or worsening bone or muscle symptoms while receiving preparations containing TDF.1
Consider BMD monitoring in adult and pediatric patients who have a history of pathologic bone fracture or other risk factors for osteoporosis or bone loss.1 Although effect of calcium and vitamin D supplementation not studied, such supplementation may be beneficial.1 If bone abnormalities are suspected, obtain appropriate consultation.1
Lactic Acidosis and Severe Hepatomegaly with Steatosis
Lactic acidosis and severe hepatomegaly with steatosis (sometimes fatal) reported in patients receiving HIV NRTIs, including FTC and TDF, alone or in combination with other antiretroviral agents.1
Interrupt FTC/TDF treatment in any patient who develops clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity (signs of hepatotoxicity may include hepatomegaly and steatosis even in the absence of marked increases in serum aminotransferase concentrations).1
Interactions
Concomitant use with certain drugs may result in known or potentially clinically important drug interactions, some of which may increase plasma concentrations of concomitant drugs leading to clinically important adverse reactions.1 (See Interactions.)
Consider potential for drug interactions prior to and during FTC/TDF therapy; review concomitant drugs during FTC/TDF therapy and monitor for adverse effects.1
Use of Fixed Combinations
Consider cautions, precautions, contraindications, and interactions associated with each component of FTC/TDF.1 Consider cautionary information applicable to specific populations (e.g., pregnant or nursing women, individuals with hepatic or renal impairment, geriatric patients) for each drug in the fixed combination.1
FTC/TDF is used in conjunction with other antiretrovirals for the treatment of HIV-1 infection.1 FTC/TDF is used alone without any other antiretrovirals for PrEP for prevention of HIV-1 infection.1 197
Specific Populations
Pregnancy
Antiretroviral Pregnancy Registry (APR) at 800-258-4263 or [Web].1 202
Available data from APR show an incidence of major birth defects with first-trimester exposure of 2.3 or 2.1% for FTC or TDF, respectively, compared with a background rate for major birth defects of 2.7% in a US reference population of the Metropolitan Atlanta Congenital Defects Program.1
Experts state that FTC/TDF is a preferred dual NRTI option for use in conjunction with an HIV INSTI or HIV PI for initial treatment of HIV-1 infection in antiretroviral-naive pregnant women, and is a preferred dual NRTI option in pregnant women coinfected with HBV.202 These experts state that FTC/TDF in conjunction with an HIV NNRTI is an alternative regimen for initial treatment of HIV-1 infection in antiretroviral-naive pregnant women.202
Experts state that the dual NRTI option of FTC/TDF used in conjunction with lopinavir/ritonavir, dolutegravir, raltegravir, or darunavir/ritonavir is among preferred regimens for treatment of HIV type 2 (HIV-2) infection† [off-label] in pregnant women.202
In HIV-1-negative women at risk of acquiring HIV-1, consider methods to prevent HIV-1, including initiating or continuing FTC/TDF PrEP, taking into account the potential increased risk of HIV-1 infection during pregnancy and the increased risk of mother-to-child transmission during acute HIV-1 infection.1
Lactation
FTC/TDF distributed into human milk in low concentrations.1
Not known whether FTC/TDF affects human milk production or affects the breast-fed infant.1
Instruct HIV-infected women not to breast-feed because of risk of HIV transmission (in HIV-negative infants), risk of development of viral resistance (in HIV-positive infants), and risk of adverse effects in the infant.1 202
In HIV-uninfected women, consider developmental and health benefits of breast-feeding and mother’s clinical need for FTC/TDF for HIV-1 PrEP along with any potential adverse effects on breast-fed child from FTC/TDF and risk of HIV-1 acquisition due to nonadherence and subsequent mother to child transmission.1 Advise women not to breast-feed if acute HIV-1 infection is suspected because of the risk of HIV-1 transmission to the infant.1
Pediatric Use
Safety and efficacy for treatment of HIV-1 infection not established in pediatric patients weighing <17 kg;1 safety and efficacy for HIV-1 PrEP not established in pediatric patients weighing <35 kg.1
Adverse effects reported in children 3 months to <18 years of age receiving FTC in clinical studies similar to those in adults, with exception of higher frequency of anemia and hyperpigmentation.1 Adverse effects reported in children 2 to <18 years of age receiving TDF in clinical studies have been similar to those in adults.1
Adverse effects reported in adolescents 15–18 years of age receiving FTC/TDF in clinical trials for HIV-1 PrEP similar to those in adults.1
In clinical trials in HIV-1 infected subjects 2 years of age to <18 years of age, similar bone effects observed in pediatric and adolescent subjects receiving TDF compared with adult subjects, suggesting increased bone turnover.1 Total BMD gain decreased in TDF-treated HIV-1 infected pediatric subjects compared with control groups.1 Similar trends observed in adolescent subjects 12 years of age to <18 years of age treated for chronic HBV infection.1 Skeletal growth (height) appeared unaffected in all pediatric trials.1
Consider BMD monitoring in pediatric patients with history of pathologic bone fracture or other risk factors for osteoporosis or bone loss.1 Although effects of calcium and vitamin D supplementation not studied, such supplementation may be beneficial.1 If bone abnormalities are suspected, obtain appropriate consultation.1
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether they respond differently than younger adults.1
Hepatic Impairment
Not studied in patients with hepatic impairment.1
Renal Impairment
Assess Scr, estimated Clcr, urine glucose, and urine protein prior to initiating FTC/TDF and routinely monitor during treatment in all patients as clinically appropriate.1 In patients with chronic kidney disease, also assess serum phosphorus at baseline and during treatment as clinically appropriate.1
Do not use for treatment of HIV-1 in patients with Clcr <30 mL/minute or patients with end-stage renal disease requiring dialysis.1 Dosage adjustments necessary when used for treatment of HIV-1 infection in those with Clcr 30–49 mL/minute.1 Do not use for PrEP in HIV-1 uninfected adults with Clcr <60 mL.1 If Clcr decreases during FTC/TDF PrEP, evaluate potential causes and reassess potential risks and benefits of continued use.1
Common Adverse Effects
HIV-infected patients (≥10% of patients): Nausea, fatigue, headache, dizziness, depression, insomnia, abnormal dreams, rash.1
PrEP (≥2% of patients): Headache, abdominal pain, decrease in weight.1
Drug Interactions
No pharmacokinetic interactions have been reported between the components of the fixed combination (i.e., FTC, TDF).1 Administration of FTC 200 mg once daily with TDF 300 mg once daily for 7 days in healthy subjects had no effect on the pharmacokinetics of tenofovir; an increase in FTC minimum concentration of 20% and no change in FTC peak concentration or AUC were observed.1
The following drug interactions are based on studies using FTC or TDF alone or the fixed combination of FTC/TDF or are predicted to occur.1 Consider interactions associated with each drug in the fixed combination.1
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
FTC is not a substrate of CYP isoenzymes and does not inhibit CYP1A2, 2A6, 2B6, 2C9, 2C19, 2D6, or 3A4.218
Tenofovir is not a substrate of CYP isoenzymes; in in vitro studies does not inhibit CYP isoenzymes 3A4, 2D6, 2C9, or 2E1, but may have a slight inhibitory effect on CYP1A.221
Based on in vitro studies and clinical pharmacokinetic drug-drug interaction trials, pharmacokinetic interactions between FTC/TDF and drugs affecting or metabolized by hepatic microsomal enzymes unlikely.1
Drugs Affecting or Affected by P-glycoprotein Transport
TDF is a substrate of P-glycoprotein (P-gp).1 When used concomitantly with an inhibitor of P-gp, increase in tenofovir absorption may occur.1
Drugs Affecting or Affected by Breast Cancer Resistance Protein
TDF is a substrate of breast cancer resistance protein (BCRP).1 When used concomitantly with an inhibitor of BCRP, increase in tenofovir absorption may occur.1
Drugs Affecting Renal Function
FTC and TDF are principally excreted by the kidneys by a combination of glomerular filtration and active tubular secretion.1
No drug-drug interactions due to competition for renal excretion have been observed; however, potential pharmacokinetic interactions if FTC/TDF used concomitantly with drugs that reduce renal function or compete for active tubular secretion (e.g., acyclovir, adefovir dipivoxil, aminoglycosides [e.g., gentamicin], cidofovir, ganciclovir, valacyclovir, valganciclovir, high-dose or multiple nonsteroidal anti-inflammatory agents [NSAIAs]); may result in increased concentrations of FTC, TDF, and/or the concomitant drug and increased risk of adverse effects.1 Avoid concomitant use of FTC/TDF and nephrotoxic drugs.1
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Abacavir |
No evidence of antagonism between FTC or TDF and abacavir1 No effect of FTC/TDF on pharmacokinetics of abacavir1 |
|
|
Adefovir dipivoxil |
Potential increase in concentrations of FTC/TDF and/or adefovir1 |
Avoid concomitant use of FTC/TDF with nephrotoxic drugs1 |
|
Aminoglycosides |
Potential increase in concentrations of FTC/TDF and/or aminoglycoside1 |
Avoid concomitant use of FTC/TDF with nephrotoxic drugs1 |
|
Amprenavir |
No antagonism observed between FTC or TDF and amprenavir1 |
|
|
Atazanavir |
No in vitro evidence of antagonistic antiretroviral effects between FTC and atazanavir203 Pharmacokinetic interaction: TDF decreases atazanavir concentrations; atazanavir also may increase tenofovir concentrations1 |
When used concomitantly with FTC/TDF, use atazanavir (300 mg) given with ritonavir (100 mg);1 monitor patients receiving FTC/TDF concomitantly with ritonavir-boosted atazanavir for tenofovir-associated adverse reactions1 Discontinue FTC/TDF in patients who develop tenofovir-associated adverse reactions1 |
|
Darunavir/ritonavir |
Pharmacokinetic interaction: Ritonavir-boosted darunavir increases tenofovir concentrations1 |
Monitor patients receiving FTC/TDF concomitantly with ritonavir-boosted darunavir for tenofovir-associated adverse reactions; discontinue FTC/TDF in patients who develop tenofovir-associated adverse reactions1 |
|
Delavirdine |
No evidence of antagonism between FTC or TDF and delavirdine1 |
|
|
Didanosine |
Pharmacokinetic interaction: TDF increases didanosine concentrations; may result in didanosine toxicity (e.g., pancreatitis, neuropathy)1 No evidence of antagonism between TDF and didanosine1 |
Closely monitor patients receiving FTC/TDF and didanosine concomitantly for didanosine-associated adverse reactions1 Patients weighing >60 kg: Reduce didanosine dosage to 250 mg when it is used concomitantly with FTC/TDF1 Patients (adult or pediatric) weighing <60 kg: Data not available to recommend an adjusted dosage for didanosine in patients receiving FTC/TDF1 When used concomitantly, FTC/TDF and delayed-release didanosine capsules (Videx EC) may be taken under fasted conditions or with a light meal (<400 kcal, 20% fat)1 Discontinue didanosine in patients who develop didanosine-associated adverse reactions1 |
|
Efavirenz |
No evidence of antagonism between FTC or TDF and efavirenz1 No clinically important pharmacokinetic interactions between TDF and efavirenz1 |
|
|
Elbasvir and grazoprevir |
Fixed combination of elbasvir and grazoprevir (elbasvir/grazoprevir): Clinically important pharmacokinetic interactions with emtricitabine not expected177 |
|
|
Entecavir |
Pharmacokinetic interaction unlikely1 |
|
|
Etravirine |
No in vitro evidence of antagonistic antiretroviral effects between FTC and etravirine214 |
|
|
Indinavir |
No clinically important pharmacokinetic interactions between FTC and indinavir1 No antagonism observed between TDF and indinavir1 |
|
|
Lamivudine |
No potential benefit of concomitant use with FTC1 |
Do not use concomitantly200 |
|
Ledipasvir/sofosbuvir |
Pharmacokinetic interaction: Increased tenofovir concentrations1 |
Monitor patients receiving FTC/TDF concomitantly with ledipasvir/sofosbuvir without an HIV-1 protease inhibitor/ritonavir or HIV-1 protease inhibitor/cobicistat combination for adverse reactions associated with tenofovir1 Patients receiving FTC/TDF concomitantly with ledipasvir/sofosbuvir and an HIV-1 protease inhibitor/ritonavir or an HIV-1 protease inhibitor/cobicistat combination: Consider alternative HCV or antiretroviral therapy, as safety of increased tenofovir concentrations in this setting not established; if coadministration necessary, monitor for adverse reactions associated with tenofovir1 |
|
Lopinavir/ritonavir |
Pharmacokinetic interaction: Increased tenofovir concentrations1 |
Monitor patients receiving FTC/TDF concomitantly with lopinavir/ritonavir for tenofovir-associated adverse reactions; discontinue FTC/TDF in patients who develop tenofovir-associated adverse reactions1 |
|
Maraviroc |
No in vitro evidence of antagonistic antiretroviral effects between FTC and maraviroc224 |
|
|
Methadone |
No clinically important pharmacokinetic interactions expected between TDF and methadone1 |
|
|
Nelfinavir |
No antagonism observed between FTC or TDF and nelfinavir1 No clinically important pharmacokinetic interactions between TDF and nelfinavir1 |
|
|
Nevirapine |
No evidence of antagonism between FTC or TDF and nevirapine1 |
|
|
NSAIAs |
Potential increase in concentrations of FTC/TDF and/or NSAIA, especially with high-dose or multiple NSAIA use1 |
Consider alternatives to NSAIAs, if needed, in patients at risk for renal dysfunction1 |
|
Nucleoside and nucleotide antiviral agents (acyclovir, cidofovir, ganciclovir, valacyclovir, valganciclovir) |
Potential for increased concentrations of FTC/TDF and/or antiviral agent due to competition for active tubular secretion and/or reduced renal function1 Famciclovir: No clinically important pharmacokinetic interactions between FTC and famciclovir1 Ribavirin: No clinically important pharmacokinetic interactions between TDF and ribavirin1 |
Avoid concomitant use of FTC/TDF with nephrotoxic drugs1 |
|
Oral contraceptives |
No clinically important pharmacokinetic interactions expected between TDF and oral contraceptives1 |
|
|
Rilpivirine |
Pharmacokinetic interactions unlikely226 No in vitro evidence of antagonistic antiretroviral effects between FTC and rilpivirine226 |
|
|
Ritonavir |
No antagonism observed between FTC or TDF and ritonavir1 |
|
|
Saquinavir |
No antagonism observed between FTC or TDF and saquinavir1 |
|
|
Saquinavir/ritonavir |
Pharmacokinetic interaction: Potential for increased tenofovir and/or saquinavir concentrations; not expected to be clinically important1 |
Dosage adjustments not required1 |
|
Simeprevir |
Clinically important interactions with FTC not expected187 |
|
|
Sofosbuvir |
Clinically important interactions with FTC or TDF not expected1 188 |
|
|
Sofosbuvir/velpatasvir |
Pharmacokinetic interaction: increased tenofovir concentrations1 |
Monitor for tenofovir-associated adverse effects1 |
|
Sofosbuvir/velpatasvir/voxilaprevir |
Pharmacokinetic interaction: increased tenofovir concentrations1 |
Monitor for tenofovir-associated adverse effects1 |
|
Stavudine |
No clinically important pharmacokinetic interaction between FTC and stavudine1 No antagonism observed between FTC or TDF and stavudine1 |
|
|
Tacrolimus |
Clinically important interactions between tacrolimus and FTC/TDF unlikely1 |
|
|
Tipranavir |
In vitro evidence of additive antiretroviral effects between FTC and tipranavir observed211 |
|
|
Tipranavir/ritonavir |
Potential pharmacokinetic interaction; variable effects on tenofovir and tipranavir pharmacokinetics observed1 |
|
|
Zidovudine |
No antagonism observed between FTC or TDF and zidovudine1 No clinically important pharmacokinetic interactions between FTC and zidovudine1 |
Emtricitabine and Tenofovir Disoproxil Fumarate Pharmacokinetics
Absorption
Bioavailability
FTC: 92%.1
TDF: 25%.1
Food
Food does not have a clinically important effect on FTC or tenofovir absorption.1
Administration of FTC/TDF with a high-fat meal (784 kcal, 49 g fat) or a light meal (373 kcal, 8 g fat) delayed time to peak tenofovir concentration by approximately 0.75 hours and increased tenofovir AUC and peak plasma concentration by 35 and 15%, respectively, compared with administration in the fasting state;1 FTC exposure was not affected by administration with either a high fat or light meal.1
Plasma Concentrations
Fixed-combination tablet containing FTC 200 mg and TDF 300 mg (FTC/TDF) is bioequivalent to a 200-mg capsule of FTC and 300-mg tablet of TDF.1
Peak plasma concentrations of FTC and tenofovir occur 1–2 hours and 1 hour, respectively, after oral administration.1
Distribution
Extent
FTC: Distributed into saliva33 and into vaginal tissue and cervicovaginal fluid following oral administration.30 31 36 Crosses human placenta.202
FTC/TDF: Distributed into human milk in low concentrations.1 34
Plasma Protein Binding
FTC: <4 %; independent of concentration over range of 0.02–200 mcg/mL.1
Tenofovir: <0.7%; independent of concentration over range of 0.01–25 mcg/mL.1
Elimination
Metabolism
FTC: Intracellularly, phosphorylated and converted by cellular enzymes to the active metabolite, emtricitabine 5′-triphosphate.1 Metabolites include 3′-sulfoxide diastereomers and their glucuronic acid conjugate.1
TDF: Undergoes diester hydrolysis in vivo to tenofovir and is subsequently metabolized to the active metabolite (tenofovir diphosphate).1 Does not undergo hepatic metabolism.221
Elimination Route
FTC: Excreted in urine (86%; 13% as metabolites).1 Eliminated by glomerular filtration and active tubular secretion.1 Removed by hemodialysis; not known whether removed by peritoneal dialysis.1
Tenofovir: Eliminated by glomerular filtration and active tubular secretion; following an IV dose, 70–80% eliminated in urine as unchanged drug.1 Removed by hemodialysis.1
Half-life
FTC: 10 hours.1
Tenofovir: 17 hours.1
Special Populations
FTC/TDF concentrations increased in patients with renal impairment.1 Modify dosing interval in HIV-infected adults with estimated Clcr of 30–49 mL/minute.1 FTC/TDF not recommended in individuals with estimated Clcr <30 mL/minute or in individuals with end-stage renal disease requiring dialysis.1 Data insufficient to make dosage recommendations for pediatric patients with renal impairment.1
FTC: Hemodialysis treatment removes approximately 30% of dose of FTC over a 3-hour dialysis period starting within 1.5 hours of FTC dosing (blood flow rate of 400 mL/minute and a dialysate flow rate of 600 mL/minute).1 Not known whether FTC can be removed by peritoneal dialysis.1
Tenofovir: Efficiently removed by hemodialysis with an extraction coefficient of approximately 54%.1 Following a single 300-mg dose of TDF, a 4-hour hemodialysis session removed approximately 10% of the administered dose.1
FTC: Pharmacokinetics not studied in patients with hepatic impairment; clinically important changes in emtricitabine metabolism not expected.1
Tenofovir: No change in pharmacokinetics observed in patients with moderate to severe hepatic impairment receiving a 300-mg dose of TDF.1
FTC/TDF: Not studied in patients with hepatic impairment.1
Stability
Storage
Oral
Tablets
25°C (excursions permitted to 15–30°C).1 Store in original container; keep tightly closed.1
Actions and Spectrum
-
Fixed combination containing FTC, an HIV NRTI antiretroviral, and TDF, an HIV nucleotide reverse transcriptase inhibitor.1
-
FTC inactive until converted intracellularly to an active 5′-triphosphate metabolite.1
-
TDF inactive until it undergoes diester hydrolysis in vivo to tenofovir and is subsequently metabolized to the active metabolite (tenofovir diphosphate).1
-
FTC and TDF are active in vitro against HIV-1 and HIV-2.1 218 221 Also have some activity against HBV.5 7 200
-
Inhibits replication of HIV by interfering with viral RNA-directed DNA polymerase (reverse transcriptase).1
-
HIV-1 with reduced susceptibility to FTC and TDF have been produced in vitro and have emerged during therapy with the drug.1
-
HIV resistant to FTC or TDF may be cross-resistant to some other NRTIs (e.g., lamivudine, abacavir, didanosine).1
Advice to Patients
-
Importance of advising patients to read the FDA-approved patient labeling (medication guide).1
-
Critical nature of compliance with HIV therapy and importance of remaining under the care of a clinician.1 Importance of taking as prescribed; do not alter or discontinue antiretroviral regimen without consulting clinician.1 Importance of advising patients that missing doses may result in development of resistance.1
-
Importance of using emtricitabine/tenofovir DF (FTC/TDF) in conjunction with other antiretrovirals for treatment of HIV-1 infection—not for monotherapy.1
-
Advise patients receiving FTC/TDF in conjunction with other antiretrovirals for treatment of HIV-1 infection that early initiation of antiretroviral therapy and sustained decreases in plasma HIV RNA have been associated with reduced risk of progression to acquired immunodeficiency syndrome (AIDS) and death.200 Advise patients that effective antiretroviral regimens can decrease HIV concentrations in blood and genital secretions and strict adherence to such regimens in conjunction with risk-reduction measures may decrease, but cannot absolutely eliminate, the risk of secondary transmission of HIV to others.200 Importance of continuing to practice safer sex (e.g., using latex or polyurethane condoms to minimize sexual contact with body fluids) and reducing high-risk behaviors (e.g., reusing or sharing needles).200
-
Advise HIV-negative individuals taking FTC/TDF for HIV-1 PrEP of the importance of confirming that they are HIV-1-negative before starting PrEP, importance of regular HIV-1 testing (at least every 3 months or more frequently for some individuals [e.g., adolescents]) during PrEP, importance of strictly adhering to recommended dosage schedule and not missing any doses, and importance of using a complete prevention strategy that also includes other measures (e.g., consistent condom use, testing [self and partners] for other sexually transmitted infections such as syphilis, chlamydia, and gonorrhea that may facilitate HIV-1 transmission).1 Advise uninfected individuals that PrEP does not protect all individuals from acquiring HIV-1 and to report any symptoms of acute HIV-1 infection (e.g., fever, headache, fatigue, arthralgia, vomiting, myalgia, diarrhea, pharyngitis, rash, night sweats, cervical and inguinal adenopathy) immediately to a clinician.1 Advise patients that HIV-1 resistance substitutions may emerge in individuals with undetected HIV-1 infection who are taking FTC/TDF, because FTC/TDF alone does not constitute a complete regimen for HIV-1 treatment.1
-
Inform patients that testing for HBV infection is recommended before antiretroviral therapy is initiated.1 Also advise patients that severe acute exacerbations of HBV infection have been reported following discontinuance of FTC/TDF in patients infected with HBV.1 Advise patients with HBV not to discontinue FTC/TDF without consulting their clinician.1
-
Importance of advising patients that renal impairment, including cases of acute renal failure and Fanconi syndrome, has been reported in association with the use of TDF, a component of FTC/TDF.1 Advise patients to avoid FTC/TDF with concurrent or recent use of a nephrotoxic agent (e.g., high-dose or multiple nonsteroidal anti-inflammatory agents [NSAIAs]).1 The dosage interval of FTC/TDF may need adjustment in HIV-1 infected patients with renal impairment.1 FTC/TDF should not be used for HIV-1 PrEP in HIV-1 uninfected individuals if estimated creatinine clearance is less than 60 mL/minute.1 If a decrease in estimated creatinine clearance is observed in uninfected individuals while using FTC/TDF for HIV-1 PrEP, potential causes should be evaluated and potential risks and benefits of continued use reassessed.1
-
Inform patients that in some patients with advanced HIV infection, signs and symptoms of inflammation from previous infections may occur soon after anti-HIV treatment is initiated.1 These symptoms may be due to an improvement in immune response, enabling the body to fight infections that may have been present with no obvious symptoms.1 Advise patients to inform their clinician immediately of any symptoms of possible infection.1
-
Inform patients that decreases in bone mineral density have been observed with the use of TDF or FTC/TDF.1 Bone monitoring may be recommended in those with a history of pathologic bone fracture or at risk for osteopenia.1
-
Advise patients of risk of lactic acidosis and severe hepatomegaly with steatosis, including fatal cases.1 Importance of contacting clinician and suspending treatment if recommended if symptoms suggestive of lactic acidosis or pronounced hepatotoxicity (e.g., unusual muscle pain, shortness of breath or fast breathing, cold or blue hands and feet, dizziness or lightheadedness, fast or abnormal heartbeat, nausea, vomiting, unusual/unexpected stomach discomfort, weakness or unusual tiredness) occur.1
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 Advise patients of pregnancy registry.1 Advise HIV-infected women and women in whom acute HIV-1 infection is suspected not to breast-feed.1
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription (e.g., other antiviral agents) and OTC drugs and dietary or herbal products.1 Importance of advising patients that FTC/TDF may interact with many other drugs.1
-
Importance of advising patients of other important precautionary information.1 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
Emtricitabine 100 mg and Tenofovir Disoproxil Fumarate 150 mg |
Truvada |
Gilead |
|
Emtricitabine 133 mg and Tenofovir Disoproxil Fumarate 200 mg |
Truvada |
Gilead |
||
|
Emtricitabine 167 mg and Tenofovir Disoproxil Fumarate 250 mg |
Truvada |
Gilead |
||
|
Emtricitabine 200 mg and Tenofovir Disoproxil Fumarate 300 mg |
Truvada |
Gilead |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions November 28, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Gilead Sciences. Truvada (emtricitabine/tenofovir disoproxil fumarate) tablets prescribing information. Foster City, CA; 2020 Jun. https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=54e82b13-a037-49ed-b4b3-030b37c0ecdd
5. Seigneres B, Martin P, Werle B et al. Effects of pyrimidine and purine analog combinations in the duck hepatitis B virus infection model. Antimicrob Agents Chemother. 2003; 47:1842-52. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=155836&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/12760857?dopt=AbstractPlus
7. Gish RG, Leung NWY, Wright TL et al. Dose range study of pharmacokinetics, safety, and preliminary antiviral activity of emtricitabine in adults with hepatitis B virus infection. Antimicrob Agents Chemother. 2002; 46:1734-40. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=127249&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/12019083?dopt=AbstractPlus
23. Gallant JE, DeJesus E, Arribas JR et al. Tenofovir DF, emtricitabine, and efavirenz vs. zidovudine, lamivudine, and efavirenz for HIV. N Engl J Med. 2006; 354:251-60. http://www.ncbi.nlm.nih.gov/pubmed/16421366?dopt=AbstractPlus
30. Dumond JB, Yeh RF, Patterson KB et al. Antiretroviral drug exposure in the female genital tract: implications for oral pre- and post-exposure prophylaxis. AIDS. 2007; 21:1899-907. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=2862268&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/17721097?dopt=AbstractPlus
31. Karim SS, Kashuba AD, Werner L et al. Drug concentrations after topical and oral antiretroviral pre-exposure prophylaxis: implications for HIV prevention in women. Lancet. 2011; 378:279-81. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=3652579&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/21763939?dopt=AbstractPlus
33. de Lastours V, Fonsart J, Burlacu R et al. Concentrations of tenofovir and emtricitabine in saliva: implications for preexposure prophylaxis of oral HIV acquisition. Antimicrob Agents Chemother. 2011; 55:4905-7. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=3186994&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/21788466?dopt=AbstractPlus
34. Benaboud S, Pruvost A, Coffie PA et al. Concentrations of tenofovir and emtricitabine in breast milk of HIV-1-infected women in Abidjan, Cote d'Ivoire, in the ANRS 12109 TEmAA Study, Step 2. Antimicrob Agents Chemother. 2011; 55:1315-7. http://www.ncbi.nlm.nih.gov/pubmed/21173182?dopt=AbstractPlus
36. Patterson KB, Prince HA, Kraft E et al. Penetration of tenofovir and emtricitabine in mucosal tissues: implications for prevention of HIV-1 transmission. Sci Transl Med. 2011; 3:112re4. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=3483088&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/22158861?dopt=AbstractPlus
177. Merck & Co., Inc. Zepatier (elbasvir and grazoprevir) tablets prescribing information. Whitehouse Station, NJ; 2016 Jan.
187. Janssen. Olysio (simeprevir) capsules prescribing information. Titusville, NJ; 2016 Jan.
188. Gilead Sciences, Inc. Sovaldi (sofosbuvir) tablets prescribing information. Foster City, CA; 2015 Aug.
197. US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States - 2021 update: a clinical practice guideline. From CDC website. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf
198. Centers for Disease Control and Prevention. Updated guidelines for antiretroviral postexposure prophylaxis after sexual, injection drug use, or other nonoccupational exposure to HIV – United States, 2016. From CDC website. https://stacks.cdc.gov/view/cdc/38856
199. Kuhar DT, Henderson DK, Struble KA et al. Updated US Public Health Service guidelines for the management of occupational exposures to human immunodeficiency virus and recommendations for postexposure prophylaxis. Infect Control Hosp Epidemiol. 2013; 34:875-92. http://www.ncbi.nlm.nih.gov/pubmed/23917901?dopt=AbstractPlus
200. Panel on Antiretroviral Guidelines for Adults and Adolescents, US Department of Health and Human Services (HHS). Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents (August 16, 2021). Updates may be available at HHS HIV Information (HIVinfo) website. https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/AdultandAdolescentGL.pdf
201. Panel on Antiretroviral Therapy and Medical Management of Children Living with HIV, US Department of Health and Human Services (HHS). Guidelines for the use of antiretroviral agents in pediatric HIV infection (April 14, 2020). Updates may be available at HHS AIDS Information (AIDSinfo) website. https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/PediatricGuidelines.pdf
202. Panel on Treatment of HIV During Pregnancy and Prevention of Perinatal Transmission, US Department of Health and Human Services (HHS). Recommendations for the use of antiretroviral drugs during pregnancy and interventions to reduce perinatal HIV transmission in the United States (March 17, 2022). Updates may be available at HHS HIV Information (HIVinfo) website. https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/Perinatal_GL.pdf
203. Bristol-Myers Squibb. Reyataz (atazanavir sulfate) capsules prescribing information. Princeton, NJ; 2012 Mar.
211. Boehringer Ingelheim. Aptivus (tipranavir) capsules and oral solution prescribing information. Ridgefield, CT; 2012 Apr.
214. Janssen. Intelence (etravirine) tablets prescribing information. Raritan, NJ; 2012 Mar.
218. Gilead Sciences, Inc. Emtriva (emtricitabine) capsules and oral solution prescribing information. Foster City, CA; 2021 Jun. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/208215s019lbl.pdf
221. Gilead Sciences, Inc. Viread (tenofovir disoproxil fumarate) tablets prescribing information. Foster City, CA: 2019 Apr. https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=33fd6418-fbdc-42ca-a50d-ce2a476a5418
224. ViiV Healthcare. Selzentry (maraviroc) tablets prescribing information. Research Triangle Park, NC; 2011 Nov.
226. Tibotec Therapeutics. Edurant (rilpivirine) tablets prescribing information. Raritan, NJ; 2011 May.
232. Gilead Sciences. Atripla (efavirenz/emtricitabine/tenofovir disoproxil fumarate) tablets prescribing information. Foster City, CA; 2021 Dec. https://dailymed.nlm.nih.gov/dailymed/fda/fdaDrugXsl.cfm?setid=2e97aa6d-09f7-46df-9499-63db7e9bac35
450. Grant RM, Lama JR, Anderson PL et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010; 363:2587-99. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=3079639&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/21091279?dopt=AbstractPlus
457. Thigpen MC, Kebaabetswe PM, Paxton LA et al. Antiretroviral Preexposure Prophylaxis for Heterosexual HIV Transmission in Botswana. N Engl J Med. 2012; :. http://www.ncbi.nlm.nih.gov/pubmed/22784038?dopt=AbstractPlus
463. Baeten JM, Donnell D, Ndase P et al. Antiretroviral Prophylaxis for HIV Prevention in Heterosexual Men and Women. N Engl J Med. 2012; :. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=3770474&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/22784037?dopt=AbstractPlus
Frequently asked questions
More about emtricitabine / tenofovir
- Check interactions
- Compare alternatives
- Reviews (40)
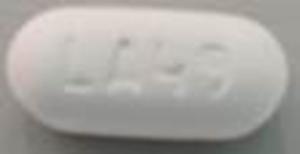
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: antiviral combinations
Patient resources
- Emtricitabine and tenofovir drug information
- Emtricitabine and tenofovir (Advanced Reading)
- Emtricitabine and Tenofovir Disoproxil Fumarate