Rykindo Dosage
Generic name: Risperidone 12.5mg in 2mL;
Dosage form: extended-release injectable suspension
Drug class: Atypical antipsychotics
Medically reviewed by Drugs.com. Last updated on Jun 9, 2023.
General Administration Information
For patients who have never taken oral risperidone, establish tolerability with oral risperidone prior to initiating RYKINDO.
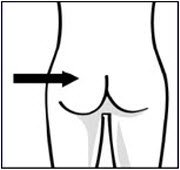
RYKINDO should be administered every 2 weeks by intramuscular (IM) gluteal injection. Each injection should be administered by a health care professional. Do not administer by any other route. Alternate injections between the two buttocks. Do not combine two different dose strengths of RYKINDO in a single administration.
For detailed preparation and administration instructions, see Dosage and Administration (2.8).
Dosage Recommendations for the Treatment of Schizophrenia
The recommended dosage of RYKINDO for the treatment of schizophrenia is 25 mg every 2 weeks. Administer the first dose of RYKINDO along with 7 days of oral risperidone.
Patients not responding to 25 mg may benefit from a higher dose of 37.5 mg or 50 mg. The maximum dose should not exceed 50 mg every 2 weeks. No additional benefit was observed with dosages greater than 50 mg of risperidone long-acting injection (intramuscular); however, a higher incidence of adverse reactions was observed. Dose titration should not be made more frequently than every 4 weeks.
Dosage Recommendations for Maintenance Treatment of Bipolar I Disorder
The recommended dosage of RYKINDO for monotherapy or adjunctive therapy to lithium or valproate for the maintenance treatment of bipolar I disorder is 25 mg every 2 weeks. Administer the first dose of RYKINDO along with 7 days of oral risperidone.
Some patients may benefit from a higher dose of 37.5 mg or 50 mg. Dosages above 50 mg have not been studied in this population. Dose titration should not be made more frequently than every 4 weeks.
Patients Currently Receiving Risperidone Long-acting Injection 2-week Intramuscular Formulation (e.g., Risperdal Consta)
The RYKINDO dose for patients receiving a risperidone long-acting injection (intramuscular) every two week formulation (e.g., Risperdal Consta) should be the same as that of the previous treatment. The first injection of RYKINDO should be given 4 weeks (no later than 5 weeks) after the last injection of the previous treatment. Supplementation with oral risperidone is not recommended [see Clinical Pharmacology (12.3)]. Titration should not be made more frequently than every 4 weeks.
Reinitiation of Treatment in Patients Previously Discontinued
There are no data to specifically address reinitiation of treatment. When restarting patients who have had an interval off treatment with RYKINDO, the previously established dosage should be reinitiated if there has been no change in the patient's general medical condition. Supplementation with oral risperidone is also required.
Dosage Recommendations for Patients with Renal or Hepatic Impairment
Patients with renal or hepatic impairment should be treated with titrated oral risperidone prior to initiating treatment with RYKINDO [see Use in Specific Populations (8.6, 8.7) and Clinical Pharmacology (12.3)]. The recommended starting dose is 0.5 mg oral risperidone twice daily during the first week, which can be increased to 1 mg twice daily or 2 mg once daily during the second week. If a total daily dose of at least 2 mg oral risperidone is well tolerated, RYKINDO 25 mg can be administered every 2 weeks with oral supplementation for 7 days following the first injection [see Dosing and Administration (2.2, 2.3)]. In some patients, slower titration may be appropriate. Alternatively, a starting dose of RYKINDO 12.5 mg may be appropriate. The efficacy of the 12.5 mg dose has not been investigated in clinical trials.
Dosage Recommendations for Concomitant Use of RYKINDO with Strong CYP2D6 Inhibitors and Strong CYP3A4 Inducers
Co-administration of carbamazepine and other CYP3A4 enzyme inducers (e.g., phenytoin, rifampin, phenobarbital) with risperidone would be expected to cause decreases in the plasma concentrations of the sum of risperidone and 9-hydroxyrisperidone combined, which could lead to decreased efficacy of RYKINDO treatment. The risperidone dose needs to be titrated accordingly for patients receiving these enzyme inducers, especially during initiation or discontinuation of therapy with these inducers [see Drug Interactions (7.1)]. At the initiation of therapy with carbamazepine or other known CYP3A4 hepatic enzyme inducers, patients should be closely monitored during the first 1 to 2 months because the dose of RYKINDO may need to be adjusted. A dose increase, or additional oral risperidone, needs to be considered. On discontinuation of carbamazepine or other CYP3A4 hepatic enzyme inducers, the dosage of RYKINDO should be re-evaluated and, if necessary, decreased. Patients may be placed on a lower dose of RYKINDO between 2 to 4 weeks before the planned discontinuation of carbamazepine or other CYP3A4 inducers to adjust for the expected increase in plasma concentrations of risperidone plus 9-hydroxyrisperidone. For patients treated with the recommended dose of 25 mg RYKINDO and discontinuing from carbamazepine or other CYP3A4 enzyme inducers, it is recommended to continue treatment with the 25-mg dose unless clinical judgment necessitates either lowering the RYKINDO dose to 12.5 mg or interruption of RYKINDO treatment. The efficacy of the 12.5 mg dose has not been investigated in clinical trials.
Fluoxetine and paroxetine, CYP2D6 inhibitors, have been shown to increase the plasma concentration of risperidone by 2.5 to 2.8-fold and 3 to 9-fold, respectively. Fluoxetine did not affect the plasma concentration of 9-hydroxyrisperidone. Paroxetine lowered the concentration of 9-hydroxyrisperidone by about 10%. The dose of risperidone needs to be titrated accordingly when co-administering fluoxetine or paroxetine. When either concomitant fluoxetine or paroxetine is initiated or discontinued, the physician should re-evaluate the dose of RYKINDO. When initiation of fluoxetine or paroxetine is considered, patients may be placed on a lower dose of RYKINDO between 2 to 4 weeks before the planned start of fluoxetine or paroxetine therapy to adjust for the expected increase in plasma concentrations of risperidone. When fluoxetine or paroxetine is initiated in patients receiving the recommended dose of 25 mg RYKINDO it is recommended to continue treatment with the 25 mg dose unless clinical judgment necessitates either lowering the RYKINDO dose to 12.5 mg or interruption of RYKINDO treatment. When RYKINDO is initiated in patients already receiving fluoxetine or paroxetine, a starting dose of 12.5 mg can be considered. The efficacy of the 12.5 mg dose has not been investigated in clinical trials. The effects of discontinuation of concomitant fluoxetine or paroxetine therapy on the pharmacokinetics of risperidone and 9-hydroxyrisperidone have not been studied [see Drug Interactions (7.1)].
Preparation and Administration Instructions
- Read the instructions for preparation and administration below and consider referring to the separate Healthcare Provider "Instructions for Use" for additional preparation and administration considerations.
- For gluteal intramuscular injection only. Do not inject by any other route. Alternate injections between the two buttocks.
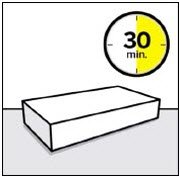
- Allow package to come to room temperature for at least 30 minutes prior to preparation. Prepare medication when you are ready to administer the dose.
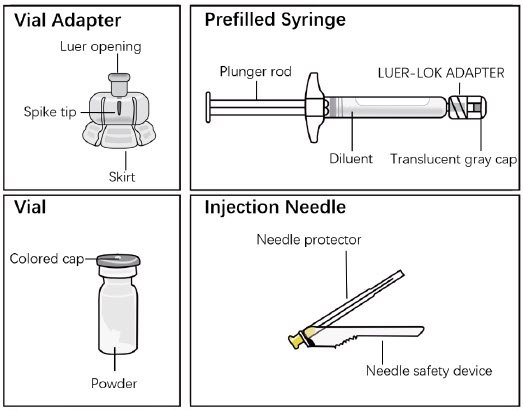
- The components in the single-dose kit are shown in Figure 1.
Figure 1. Single-dose Kit Components
Step 1. Take out kit and connect vial adapter to vial
|
|
|
|
|
|||
| Wait 30 minutes Remove dose pack from the refrigerator and allow to sit at room temperature for at least 30 minutes before reconstituting. Do not warm any other way. |
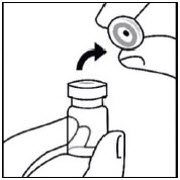
Remove cap from vial Flip off colored cap from vial. Wipe top of the gray stopper with an alcohol swab. Allow to air dry. Do not remove gray rubber stopper. |
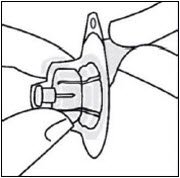
Prepare vial adapter Hold sterile blister as shown. Peel back and remove paper backing. Do not remove vial adapter from blister. Do not touch spike tip at any time. This will result in contamination. |
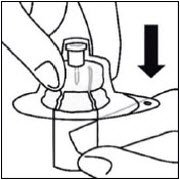
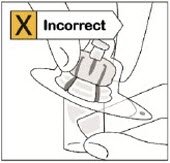
Connect vial adapter to vial Place vial on a hard surface and hold by the base. Center vial adapter over the gray rubber stopper. Push vial adapter straight down onto vial top until it snaps securely into place. Do not place vial adapter on at an angle or diluent may leak upon transfer to the vial.
|
Step 2. Connect prefilled syringe to vial adapter
|
|
|
|
|
|||
Remove sterile blister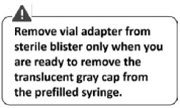 Keep vial vertical to prevent leakage. Hold base of vial and pull up on the sterile blister to remove. Do not shake. Do not touch exposed luer opening on vial adapter. This will result in contamination. |
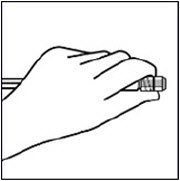
Use proper grip Hold by the LUER-LOK ADAPTER at the tip of the syringe. Do not hold syringe by the glass barrel during assembly.
|
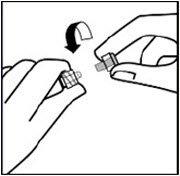
Remove cap Holding the transparent LUER-LOK ADAPTER, unscrew the translucent gray cap Do not snap or cut off the translucent gray cap Do not touch syringe tip. This will result in contamination. 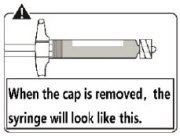 The unscrewed cap can be discarded. |
Connect syringe to vial adapter Hold vial adapter by skirt to keep stationary. Hold syringe by the LUER-LOK ADAPTER then turn it to connect with the luer opening of the vial adapter Do not hold the glass syringe barrel. This may cause the LUER-LOK ADAPTER to loosen or detach. Attach the syringe to the vial adapter with a firm clockwise twisting motion until it feels snug. Do not over-tighten. Over-tightening may cause the syringe tip to break. |
Step 3. Reconstitute powder
|
|
|
|
|
|||
| Inject diluent Inject entire amount of diluent from syringe into the vial.  |
Suspend Powder in diluent Continuing to hold down the plunger rod, shake vigorously for at least 30 seconds, as shown. Check the suspension. When properly mixed, the suspension appears uniform, thick and milky in color. Immediately proceed to the next step so suspension does not settle. |
Transfer suspension to syringe Invert vial completely. Slowly pull plunger rod down to withdraw entire contents from the vial into the syringe. |
Remove vial adapter Hold LUER-LOK ADAPTER on the syringe and unscrew from vial adapter. Tear section of the vial label at the perforation. Apply detached label to the syringe for identification purposes. Discard both vial and vial adapter appropriately. |
Step 4. Attach Needle
|
|
|
|
| Take out needle Take out needle for gluteal injection. |
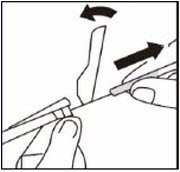
Attach needle Peel blister pouch open part way and use to grasp the base of the needle, as shown. Holding the LUER-LOK ADAPTER on the syringe, attach syringe to needle luer connection with a firm clockwise twisting motion until snug. Do not touch needle luer opening. This will result in contamination. |
Resuspend Powder Fully remove the blister pouch. Just before injection, shake syringe vigorously for 20 to 30 seconds until there is no deposition of powder, as some settling will have occurred. |
Step 5. Inject RYKINDO
|
|
|
|
|
|
||||
| Remove transparent needle protector Move the needle safety device back towards the syringe, as shown. Then hold the LUER-LOK ADAPTER on syringe and carefully pull the transparent needle protector straight off. Do not twist transparent needle protector, as the luer connection may loosen. |
Remove air bubbles Hold syringe upright and tap gently to make any air bubbles rise to the top. Slowly and carefully press plunger rod upward to remove air. |
Inject Immediately inject entire contents of syringe intramuscularly into the upper-outer quadrant of the gluteal muscle of the patient. |
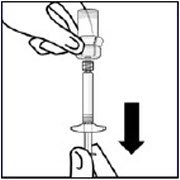
Secure needle in safety device Using one hand, place needle safety device at a 45-degree angle on a hard, flat surface. Press down with a firm, quick motion until needle is fully engaged in safety device. |
Properly dispose of syringes Check to confirm needle safety device is fully engaged. Discard in an approved sharps container. |
Frequently asked questions
More about Rykindo (risperidone)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Side effects
- During pregnancy
- FDA approval history
- Drug class: atypical antipsychotics
- Breastfeeding
Patient resources
Other brands
Risperdal, Uzedy, Risperdal Consta, Perseris, ... +2 more
Professional resources
Other brands
Risperdal, Uzedy, Risperdal Consta, Perseris
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.