Cutaquig Dosage
Generic name: HUMAN IMMUNOGLOBULIN G 165mg in 1mL
Dosage form: subcutaneous injection
Drug class: Immune globulins
Medically reviewed by Drugs.com. Last updated on Nov 20, 2023.
For subcutaneous use only .
- Before receiving treatment with CUTAQUIG: Obtain the patient's serum Immunoglobulin G (IgG) trough level to guide subsequent dose adjustments (see Dose Adjustment ).
Dose
- Individualize the dose based on the patient’s pharmacokinetic and clinical response. Monitor serum IgG trough levels regularly to guide subsequent dose adjustments as needed (see Dose Adjustment ).
- Start CUTAQUIG treatment one week after the last Immune Globulin Intravenous (IGIV)/ Immune Globulin Subcutaneous (IGSC) infusion.
Dose for patients switching to CUTAQUIG from IGIV:
- Establish the initial weekly dose of CUTAQUIG by converting the monthly IGIV dose into an equivalent weekly dose and increasing it using a dose adjustment factor.
- To calculate the initial weekly dose of CUTAQUIG, divide the monthly IGIV dose in grams by the number of weeks between IGIV infusions and then multiply this value with a Dose Adjustment Factor of 1.30.
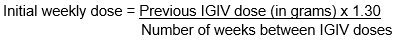
- To convert the dose (in grams) to milliliters (mL), multiply the calculated dose (in grams) by 6.
- Provided the total weekly dose is maintained, any dosing interval from daily up to weekly can be used and will result in systemic IgG exposure that is comparable to the previous IGIV treatment.
- For every other week dosing, multiply the calculated weekly CUTAQUIG dose by 2.
- For more frequent than weekly dosing (2-7 times a week) divide the calculated weekly CUTAQUIG dose by the desired number of infusions per week (e.g.: if you want to infuse CUTAQUIG 2 times per week, divide the weekly dose by 2).
- On average, serum IgG trough levels were approximately 23% higher during CUTAQUIG administration compared to those obtained during prior IGIV therapy.
- To guide dose adjustments, see Table 1 under Dose Adjustment .
Dose for patients switching to CUTAQUIG from IGSC:
- It is recommended to maintain the same weekly dosing (in grams) of CUTAQUIG that was used for the previous Immune Globulin Subcutaneous (Human) (IGSC) therapy (in grams).
- For every other week dosing, multiply the weekly dose by 2.
- For more frequent than weekly dosing (2-7 times a week) divide the weekly dose by the desired number of infusions per week (e.g.: if you want to infusion CUTAQUIG 2 times per week, divide the weekly dose by 2).
- To convert the dose (in grams) to milliliters (mL), multiply the calculated dose (in grams) by 6.
- Obtain a trough IgG level before switching, monitor clinical response and check the trough IgG level 2 to 3 months after initiating CUTAQUIG.
- To guide dose adjustments, see Table 1 under Dose Adjustment , if the trough IgG level during CUTAQUIG administration differs from the trough IgG level obtained during treatment with the previously administered IGSC product or target trough level.
Over time the dose may need to be individualized for each patient, depending on the pharmacokinetic and clinical response and on the desired IgG trough level. Measure the patient’s serum IgG trough level 2-3 months after switching to CUTAQUIG or after the last CUTAQUIG dose adjustment, in order to determine if a dose adjustment is necessary.
Calculate the difference between the patient’s target serum IgG trough level (in mg/dL) and the IgG trough level obtained during subcutaneous treatment with CUTAQUIG. Find this difference in column 1 of Table 1 and according to frequency of administration (weekly or every other week) locate the corresponding adjustment amount of CUTAQUIG in mL/administration according to the body weight of the patient.
For more frequent dosing than weekly or every other week, add the weekly increment from Table 1 to the weekly equivalent dose of the patient and then divide by the desired number of administrations per week.
Use the patient’s clinical response as the primary point to consider for any dose adjustment. Additional dose increments may be indicated based on the patient's clinical response (i.e., infection frequency and severity).
Table 1 Incremental adjustment (mL) of weekly or every other week CUTAQUIG dosing based on the calculated difference between actual IgG trough level and the target trough level for the patient*
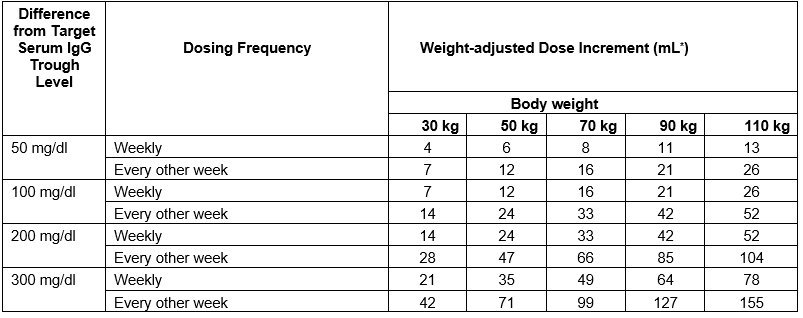
* Derived from a linear regression model of trough levels and weekly dose per kg body weight.
For example: a patient with body weight of 70 kg is treated weekly and has a trough level of 600 mg/dL, but the target trough level is 900 mg/dL. The difference between the actual trough level (600) and the targeted trough level (900) is plus 300 mg/dL. Therefore, the recommended increase in the weekly dose would be approximately 49 mL.
A patient with a body weight of 50 kg, on an every other week dosing schedule and with an actual trough level of 900 mg/dL has a target trough level of 700 mg/dL. The difference between actual trough level (900) and targeted trough level (700) is minus 200 mg/dL, therefore the patient needs a decrease in his every other week dose of approximately 47 mL.
Monitor the patient’s clinical response and periodically check trough IgG levels, and repeat dose adjustment as needed.
Measles Exposure
If a patient has been exposed to measles, it may be prudent to administer a dose of Immune Globulin Intravenous as soon as possible and within 6 days of exposure. A dose of 400 mg/kg should provide a serum level > 240 mIU/mL of measles antibodies for at least two weeks.
If a patient is at risk of future measles exposure and receives a dose of less than 245 mg/kg subcutaneously per week, increase the dose to 245 mg/kg.
Preparation
CUTAQUIG is a clear and colorless solution that may turn to slightly opalescent and pale yellow during storage. Do not use the solution if it appears cloudy or contains particulates.
- Use aseptic technique when preparing and administering CUTAQUIG.
- Prior to administration visually inspect each vial of CUTAQUIG for particulate matter, whenever the solution and container permit.
- Do not mix CUTAQUIG with other products.
- Do not dilute CUTAQUIG.
- Do not shake the solution.
- Check the labeling for the expiration date and do not use beyond this date.
- CUTAQUIG vials are for single use only. Discard any unused product after each infusion in accordance with local requirements.
- Do not freeze. Do not use frozen product.
- Record lot number in patient’s medical history.
Administration
CUTAQUIG is for subcutaneous use only.
Administer CUTAQUIG by a healthcare provider, or by caregiver or self-administered by the patient after appropriate training.
Infuse CUTAQUIG in the following areas: abdomen, thigh, upper arm, and/or upper leg/hip area.
CUTAQUIG is intended for subcutaneous use using an infusion pump and compatible syringe(s).
Infuse CUTAQUIG simultaneously into up to 6 different sites. Infusion sites should be at least 2 inches (5 cm) apart. Rotate infusion sites between subsequent administrations.
Volume:
For patients not already on IGSC therapy, do not exceed the maximum initial volume per injection site of 25 mL/site for adults (≥17 years), 15 mL/site (for ages 7-16 years) and 10 mL/site (for ages 2-6 years) for the first 2 infusions.
For subsequent infusions, if tolerated, you may gradually increase infusion volume/site by approximately 10 mL per infusion site in adults (≥17 years) and by approximately 5-10 mL per infusion site in children (2-16 years) every 2-4 weeks.
The maximum infusion volume is 40 mL/site (for adults ≥17 years), 29 mL/site (for ages 7-16 years) and 15.5 mL/site (for ages 2-6 years).
Rate:
For patients not already on IGSC therapy, do not exceed the maximum recommended flow rates per hour per infusion site of 20 mL per hour per site for adults (≥17 years) and 15 mL per hour per site for children (2-16 years) for the first 2 infusions.
For subsequent infusions, if tolerated, you may gradually increase the infusion rate by approximately 10mL/hr/site in adults (≥17 years) and by approximately 5-10 mL/hr/site in children (2-16 years) every 2-4 weeks.
The maximum infusion rate is 52 mL per hour per site for adults (≥17 years) and 25 mL per hour per site for children (2-16 years).
Table 2 Infusion Volumes and Infusion Rates (Infusion rate and infusion volume per site may gradually be increased every 2-4 weeks as tolerated by patients)
| Infusion parameters* | Infusion Number | ||
| First 2 infusions | Subsequent infusions | ||
| Volume (mL/site) | Adults ≥17 years |
≤ 25 | gradually increase by approximately 10 mL/site every 2-4 weeks up to a maximum of 40 |
| 7-16 years | ≤ 15 | gradually increase by approximately 5-10 mL/site every 2-4 weeks up to a maximum of 29 | |
| 2-6 years | ≤ 10 | gradually increase by approximately 5-10 mL/site every 2-4 weeks up to a maximum of 15.5 | |
| Rate (mL/hr/site) | Adults ≥17 years |
≤ 20 | gradually increase by approximately 10 mL/hr/site every 2-4 weeks up to a maximum of 52 |
| 2-16 years | ≤ 15 | gradually increase by approximately 10 mL/hr/site every 2-4 weeks up to a maximum of 25 |
* As tolerated
Administration/Handling instructions
CUTAQUIG is for subcutaneous use only.
Follow the administration guidance below and use aseptic technique when administrating CUTAQUIG.
 Figure 1 |
1. Getting ready for infusion - Choose and prepare a clean work area. - Gather your infusion equipment: Infusion pump and compatible syringe(s). Needle or needleless transfer device (for drawing up product from the vial). Infusion set (varies according to manufacturer’s instructions). Infusion tubing and Y-connector (if required). Ancillary supplies: disinfectant wipes, gauze or transparent dressing, tape and sharps container. Patient’s treatment diary/log book. - Wash your hands thoroughly and let them dry ( Figure 1 ). |
 Figure 2 |
2. Checking and opening the vials - If taken out of the refrigerator, allow products to reach room temperature (≤ 25°C / 77°F). - Inspect each vial carefully: Check that labelled dose is correct and based on prescription. Check that the expiration date has not been passed. Check the appearance of the solution: do not use the solution if it is cloudy or contains particles. Make sure the protective cap is not broken or missing. - Remove the protective cap. - Disinfect the rubber stopper by using a sterile wipe and allow it to dry ( Figure 2). |
 Figure 3 |
3. Preparing and filling the syringe - Open sterile syringe and needle or needleless transfer device. - If a needleless transfer device is used, follow the instructions of the device manufacturer. - If the transfer is done using needle and syringe follow the instructions below: Attach the needle to the syringe with a screw action. Draw back on the plunger to fill the syringe with air which should be roughly equal to the amount of solution needed from the vial. Insert the needle into the center of the vial stopper and turn the vial upside down. To avoid foaming, ensure that the tip of the needle is not in the solution, and then inject the air. Next, move the needle so that the tip is in the solution, and then slowly draw up the desired volume of CUTAQUIG ( Figure 3 ). Withdraw the needle from the vial. This procedure might be repeated if you need to use more than one vial. When finished, remove the needle and dispose of it into the sharps bin and proceed to the next step. |
 Figure 4 |
4. Preparing the infusion pump and tubing - Follow the manufacturer’s instructions for preparing the infusion pump. - Prime the administration tubing according to manufacturer’s instruction to eliminate all remaining air ( Figure 4 ). - Stop priming before fluid reaches the needle tip. |
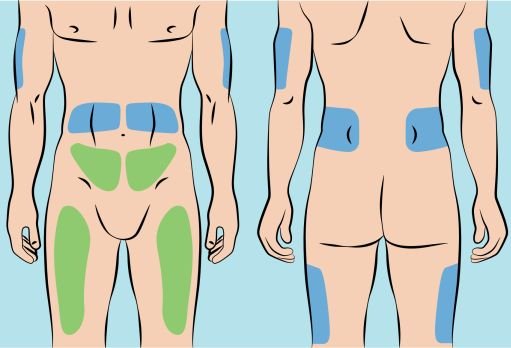 Figure 5 |
5. Preparing the infusion site(s) and inserting the infusion needle(s) - CUTAQUIG can be infused in the following areas: abdomen, thigh, upper arm, and/or upper leg/hip area ( Figure 5 ). - The number and location of injection sites depends on the volume of the total dose. The infusion sites should be at least 2 inches apart. A maximum of 6 infusion sites can be used simultaneously. - Rotate sites between infusions. - Avoid inserting the needle into scars, tattoos or injured/inflamed skin areas and inspect skin for signs of infection. - Clean your skin at your selected infusion site(s) with an antiseptic skin wipe starting at the center and working outward in a circular motion, and allow each site to dry before proceeding. |
 Figure 6 |
- Pinch the skin between your thumb and forefinger around the injection site ( Figure 6 ) and insert the needle into the subcutaneous tissue ( Figure 7 ). The angle of the needle will depend on the type of infusion set being used. |
 Figure 7 |
|
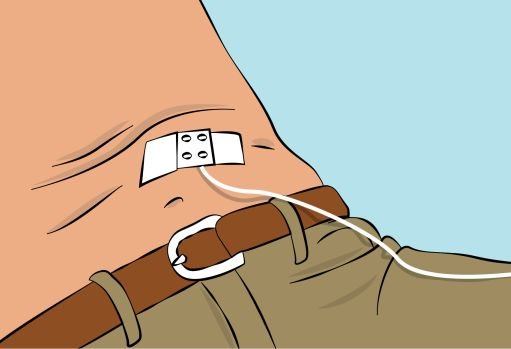 Figure 8 |
- Secure the needle in place by applying sterile gauze and tape or transparent dressing ( Figure 8 ). |
6. Checking the infusion
- Check needle placement by pulling back on the syringe plunger. There should not be any blood return in the tubing.
- If blood return is seen, remove needle and restart from step 5 with new tubing at a different location.
7. Starting the infusion
- Start the infusion. Follow infusion pump manufacturer’s instructions.
8. Recording the infusion
- On each vial of CUTAQUIG, you will find a peel-off portion of the label with the batch number details. Stick this label in your patient’s treatment diary or infusion log book. Record details of the dose, date, time, infusion site location and any infections, side effects or other comments.
9. After infusion is complete
- Gently remove the needle(s) and immediately place into the sharps bin.
- If necessary, press a small piece of gauze on the needle site and apply a dressing.
- Discard all used disposable supplies as well as any unused product and the empty vial(s) as recommended by your healthcare provider and according to local requirements.
- Clean and store the infusion pump according to the manufacturer’s instructions.
For self-administration, provide the patient and caregiver with instructions and appropriate training for infusion at home or other appropriate setting. Verify that the patient or caregiver is capable of self-administration or administration, respectively, using appropriate technique.
More about Cutaquig (immune globulin subcutaneous)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Latest FDA alerts (1)
- Side effects
- During pregnancy
- Drug class: immune globulins
- En español
Patient resources
- Cutaquig subcutaneous drug information
- Cutaquig (Immune globulin-hipp Subcutaneous) (Advanced Reading)
Other brands
Hizentra, Cuvitru, Xembify, Vivaglobin
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.

