Preeclampsia during Pregnancy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
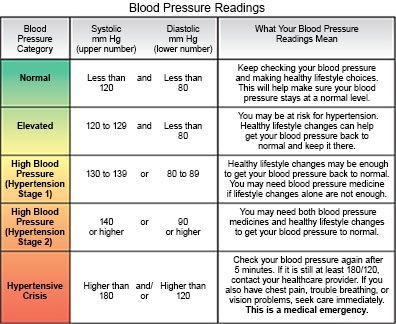
Preeclampsia is high blood pressure (BP) that usually develops after week 20 of pregnancy. It can also develop days or weeks after delivery. Your blood pressure may be 140/90 or higher. One or both numbers may be high. You may also have protein in your urine or damage to organs such as your kidneys or liver. Chronic hypertension with superimposed preeclampsia is preeclampsia in a woman with a history of hypertension before pregnancy. It can also be preeclampsia that develops before week 20 of pregnancy. Preeclampsia can lead to life-threatening conditions such as a stroke, eclampsia (seizures), or HELLP syndrome (blood cell destruction). It is important to get screened for high BP during pregnancy. High BP does not always cause symptoms. Symptoms that do develop may be general, such as headaches and swelling that you may think are not serious.
 |
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
You may need extra oxygen
if your blood oxygen level is lower than it should be. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils. Ask your healthcare provider before you take off the mask or oxygen tubing.
Intake and output:
Healthcare providers will keep track of the amount of liquid you get. They also may need to know how much you urinate. Ask healthcare providers if they need to measure or collect your urine.
Activity:
Healthcare providers may want you to limit activity. Ask your healthcare provider about activities you can and cannot do.
Medicines:
- Blood pressure medicine helps lower your blood pressure to protect your heart, lungs, brain, kidneys, and unborn baby.
- Medicine may be given to prevent seizures. This medicine is usually given through an IV.
- Steroids may be given 12 to 24 hours before your baby is delivered if he or she needs to be born early. The medicine will help your baby's lungs develop.
Tests:
- Blood tests are done to check your liver and kidney function.
- Urine tests are checked for protein.
Fetal monitoring:
- External fetal heart monitoring is used to monitor your baby's heartbeat, and the contractions of your uterus. A small monitor with gel on it is placed on your abdomen. A belt will be fastened around your waist to hold the monitor in place. The monitor may need to be moved as your baby moves inside you. A paper printout shows a tracing of your uterus contracting, and the baby's heartbeat.
- A fetal ultrasound is used to check the placenta and your baby's movement, heart rate, and position.
- An amniotic fluid index is used to measure the amniotic fluid around your unborn baby. Amniotic fluid cushions and protects your baby as he or she grows. Low amounts of amniotic fluid can limit his or her growth.
- An umbilical cord Doppler is used to check blood flow through the umbilical cord.
Delivery:
Preeclampsia may go away after the baby is born. Healthcare providers may deliver your baby right away if he or she is full-term. He or she may need to be delivered early if you or the baby has life-threatening symptoms.
RISKS:
Your baby may not grow as he or she should and may need to be delivered early. Placental abruption can occur if the placenta pulls away from the uterus too soon. This condition is life-threatening for your baby. Severe preeclampsia may cause seizures or coma. This condition is called eclampsia. Eclampsia is a life-threatening condition for you and your unborn baby. Preeclampsia and eclampsia can sometimes develop up to 30 days after you give birth. You are at increased risk for heart disease, high blood pressure, or a stroke.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Preeclampsia during Pregnancy
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
