Pneumonia in Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
Pneumonia is an infection in one or both lungs. Pneumonia can be caused by bacteria, viruses, fungi, or parasites. Viruses are usually the cause of pneumonia in children. Children with viral pneumonia can also develop bacterial pneumonia. Often, pneumonia begins after an infection of the upper respiratory tract (nose and throat). This causes fluid to collect in the lungs, making it hard to breathe. Pneumonia can also develop if something such as food or stomach acid is inhaled into the lungs.
 |
DISCHARGE INSTRUCTIONS:
Seek care immediately if:
- Your child is younger than 3 months and has a fever.
- Your child is struggling to breathe or is wheezing.
- Your child's lips or nails are bluish or gray.
- Your child's skin between the ribs and around the neck pulls in with each breath.
- Your child has any of the following signs of dehydration:
- Crying without tears
- Dizziness
- Dry mouth or cracked lip
- More irritable or fussy than normal
- Sleepier than usual
- Urinating less than usual or not at all
- Sunken soft spot on the top of the head if your child is younger than 1 year
Call your child's doctor if:
- Your child has a fever of 102°F (38.9°C), or above 100.4°F (38°C) if your child is younger than 6 months.
- Your child cannot stop coughing.
- Your child is vomiting.
- You have questions or concerns about your child's condition or care.
Medicines:
Your child may need any of the following:
- Antibiotics may be given if your child has bacterial pneumonia.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If your child takes blood thinner medicine, always ask if NSAIDs are safe for him or her. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to give your child and how often to give it. Follow directions. Read the labels of all other medicines your child uses to see if they also contain acetaminophen, or ask your child's doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Ask your child's healthcare provider before you give your child medicine for his or her cough. Cough medicines may stop your child from coughing up mucus. Also, children younger than 4 years should not take over-the-counter cough and cold medicines.
- Do not give aspirin to children younger than 18 years. Your child could develop Reye syndrome if he or she has the flu or a fever and takes aspirin. Reye syndrome can cause life-threatening brain and liver damage. Check your child's medicine labels for aspirin or salicylates.
- Give your child's medicine as directed. Contact your child's healthcare provider if you think the medicine is not working as expected. Tell the provider if your child is allergic to any medicine. Keep a current list of the medicines, vitamins, and herbs your child takes. Include the amounts, and when, how, and why they are taken. Bring the list or the medicines in their containers to follow-up visits. Carry your child's medicine list with you in case of an emergency.
Care for your child at home:
- Let your child rest and sleep as much as possible. Your child may be more tired than usual. Rest and sleep help your child's body heal.
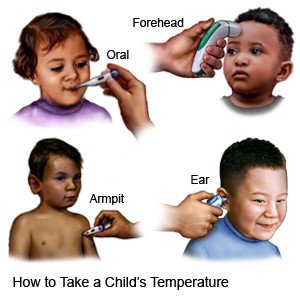
- Take your child's temperature at least 1 time each morning and 1 time each evening. You may need to take it more often if your child feels warmer than usual.
- Give your child liquids as directed. Liquids help your child to loosen mucus and keeps him or her from becoming dehydrated. Ask how much liquid your child should drink each day and which liquids are best for him or her. Your child's healthcare provider may recommend water, apple juice, gelatin, broth, and popsicles. Bottle feed or breastfeed your baby smaller amounts more often. Your child may become tired easily when feeding.
- Give your child foods that are easy to swallow. When your child starts to eat solid foods again, feed him or her small meals often. Yogurt, applesauce, and pudding are good choices.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Help your child breathe easier:
- Teach your child to take a deep breath and then cough. Have your child do this when he or she feels the need to cough up mucus. This will help get rid of the mucus in the throat and lungs, making it easier for your child to breathe.
- Do not let anyone smoke around your child. Smoke can make your child's coughing or breathing worse.
- Clear mucus out of your baby's nose. If your baby has trouble breathing through his or her nose, use a bulb syringe to remove mucus. Use a bulb syringe before you feed your child and put him or her to bed.
- Squeeze the bulb and put the tip into one of your baby's nostrils. Close the other nostril with your fingers. Slowly release the bulb to suck up the mucus.
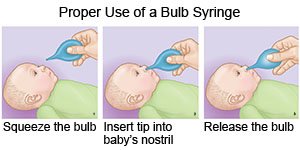
- You may need to use saline nose drops to loosen the mucus in your baby's nose. Put 3 drops into 1 nostril. Wait for 1 minute so the mucus can loosen. Then use the bulb syringe to remove the mucus and saline.
- Empty the mucus in the bulb syringe into a tissue. You can use the bulb syringe again if the mucus did not come out. Do this again in the other nostril. The bulb syringe should be boiled in water for 10 minutes when you are done, and then left to dry. This will kill most of the bacteria in the bulb syringe for the next use.
- Squeeze the bulb and put the tip into one of your baby's nostrils. Close the other nostril with your fingers. Slowly release the bulb to suck up the mucus.
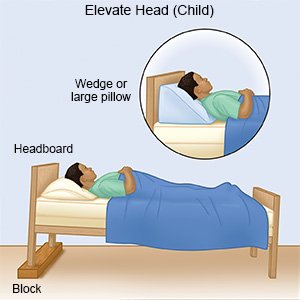
- Keep your child's head elevated. Ask your child's healthcare provider about the best way to elevate your child's head. Your child may be able to breathe better when lying with the head of the crib or bed up. Do not put pillows in the bed of a child younger than 1 year. Make sure your child's head does not flop forward. If this happens, your child will not be able to breathe properly.
- Use a cool mist humidifier to increase air moisture in your home. This may make it easier for your child to breathe and help decrease his or her cough.
Prevent pneumonia:
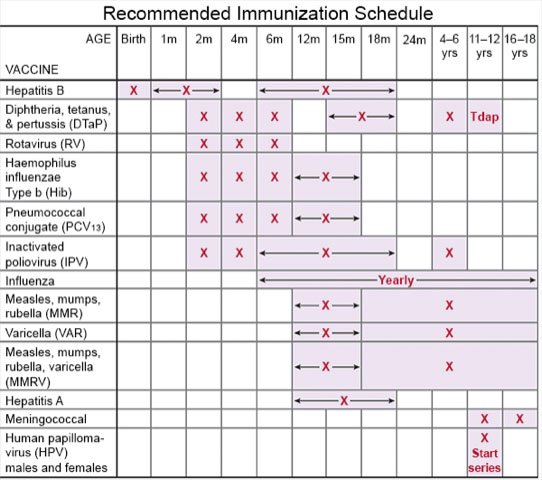
- Ask about vaccines your child needs. Children routinely get 4 doses of a vaccine to lower the risk for pneumonia. Other vaccines help lower the risk for infections that can become serious for a child who has pneumonia. Have your child get a flu vaccine each year as soon as recommended, usually in September or October. A COVID-19 vaccine is available for children 6 months or older. Your child's healthcare provider can tell you if your child also needs other vaccines, and when to get them.
- Have your child wash his or her hands often. Teach your child to use soap and water every time. Show him or her how to rub soapy hands together, lacing the fingers. The fingers of one hand should scrub under the nails of the other hand. Wash for at least 20 seconds. You can use a timer or sing a song, such as singing the alphabet song 2 times. Teach your child to rinse his or her hands with warm, running water for several seconds. Then dry with a clean towel or paper towel. Your child can use germ-killing hand sanitizer if soap and water are not available. Remind your child not to touch his or her eyes, nose, or mouth without washing his or her hands first.

- Teach your child to cover a sneeze or cough. Have your child use a tissue that covers his or her mouth and nose. Have your child throw the tissue away in a trash can right away. Show him or her how to use the bend of the arm if a tissue is not available. Then have your child wash his or her hands well with soap and water or use a hand sanitizer.
- Prevent the spread of germs. Do not let your child share food, drinks, or utensils with others.
- Keep your child away from others when needed. This includes anyone who has symptoms of a respiratory infection, such as a sore throat or cough. If your child is sick, do not let him or her go to school or other activities. Wait until your child is well or his or her healthcare provider says it is okay.
 |
Follow up with your child's doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Pneumonia
Treatment options
Care guides
- Aspiration Pneumonia
- Bacterial Pneumonia
- Community Acquired Pneumonia
- Hospital Acquired Pneumonia
- Pneumonia
- Pontiac Fever
- Viral Pneumonia
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
