Community Acquired Pneumonia
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is community-acquired pneumonia (CAP)?
CAP is a lung infection that you get outside of a hospital or nursing home setting. Your lungs become inflamed and cannot work well. CAP may be caused by bacteria, viruses, or fungi.
 |
What increases my risk for CAP?
- Chronic lung disease
- Cigarette smoking
- Brain disorders such as stroke, dementia, and cerebral palsy
- Weakened immune system
- Recent surgery or trauma
- Surgery for cancer of the mouth, throat, or neck
- Medical conditions such as diabetes or heart disease
What are the signs and symptoms of CAP?
- Cough that may bring up green, yellow, or bloody mucus
- Fever, chills, or severe shaking
- Shortness of breath
- Breathing and heartbeat that are faster than usual
- Pain in your chest or back when you breathe in or cough
- Fatigue and loss of appetite
- Trouble thinking clearly
How is CAP diagnosed?
Your healthcare provider will listen to your lungs. You may need a chest x-ray. You may also need any of the following if you are admitted to the hospital:
- CT scan pictures may show a lung infection or other problems, such as fluid around your lungs. You may be given contrast liquid to help your lungs show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
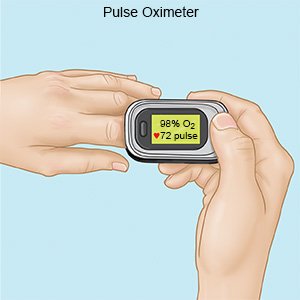
- A pulse oximeter is a device that measures the amount of oxygen in your blood.
- Blood and sputum tests may be done to check for the germ causing your infection.
- Bronchoscopy is a procedure to look inside your airway and learn the cause of your airway or lung condition. A bronchoscope (thin tube with a light) is inserted into your mouth and moved down your throat to your airway. Tissue and fluid may be collected from your airway or lungs to be tested.
- Nucleic acid-based testing , also called a PCR test, may be used to check for a virus causing your pneumonia. You may need the test if you have severe CAP or a weakened immune system.
How is CAP treated?
Treatment will depend on the type of germ causing your CAP, and how bad your symptoms are. You may need antibiotics for at least 5 days if your pneumonia is caused by bacteria. Antiviral medicines may be given if you have viral pneumonia. You may need medicines that dilate your bronchial tubes. You may need oxygen if your blood oxygen level is lower than it should be. You may need to be admitted to the hospital if your pneumonia is severe.
What can I do to manage CAP?
- Get plenty of rest. Rest helps your body heal.
- Do not smoke or allow others to smoke around you. Nicotine and other chemicals in cigarettes and cigars can cause lung damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Breathe warm, moist air. This helps loosen mucus. Loosely place a warm, wet washcloth over your nose and mouth. A room humidifier may also help make the air moist.
- Gently tap your chest. This helps loosen mucus so it is easier to cough up.
- Take deep breaths and cough. Deep breathing helps open the air passages in your lungs. Coughing helps bring up mucus from your lungs. Take a deep breath and hold the breath as long as you can. Then push the air out of your lungs with a deep, strong cough. Spit out any mucus you have coughed up. Take 10 deep breaths in a row every hour that you are awake. Remember to follow each deep breath with a cough.
- Drink liquids as directed. Ask your healthcare provider how much liquid to drink each day and which liquids to drink. Liquids help make mucus thin and easier to get out of your body.
How can I prevent CAP?
- Wash your hands often. Use soap for at least 20 seconds. Rinse with warm running water. Dry your hands with a clean towel or paper towel. Use hand sanitizer that contains alcohol if soap and water are not available. Wash your hands several times each day. Wash after you use the bathroom, change a child's diaper, and before you prepare or eat food. Do not touch your eyes, nose, or mouth without washing your hands first.

- Cover a sneeze or cough. Use a tissue that covers your mouth and nose. Throw the tissue away in a trash can right away. Use the bend of your arm if a tissue is not available. Wash your hands well with soap and water or use a hand sanitizer. Do not stand close to anyone who is sneezing or coughing.
- Clean surfaces often. Clean doorknobs, countertops, cell phones, and other surfaces that are touched often. Use a disinfecting wipe, a single-use sponge, or a cloth you can wash and reuse. Use disinfecting cleaners if you do not have wipes. You can create a disinfecting cleaner by mixing 1 part bleach with 10 parts water.
- Try to avoid people who have a cold or the flu. If you are sick, stay away from others as much as possible.
- Ask about vaccines you may need. Your healthcare provider can tell you if you should also get vaccines other than those listed below, and when to get them:
- Get an influenza (flu) vaccine as directed. The flu vaccine is recommended for everyone 6 months or older. Get the vaccine as soon as recommended each year, usually in September or October.
- Get a COVID-19 vaccine as directed. At least 1 dose of an updated vaccine is recommended for everyone 6 months or older. COVID-19 vaccines are given as a shot in 1 to 3 doses, depending on the age of the person who receives it. COVID-19 vaccines are updated throughout the year. Your healthcare provider can help you schedule all needed doses as updated vaccines become available.
- Get a pneumonia vaccine as directed. The vaccine is recommended for all adults aged 50 or older. Adults aged 19 to 49 years who are at high risk for pneumonia should also receive the vaccine. You may need 1 dose or 2. The number depends on the vaccine used and your risk factors. Children routinely receive 4 doses of the pneumonia vaccine, starting at 2 months.
 |
When should I seek immediate care?
- You are confused and cannot think clearly.
- You have increased trouble breathing.
- Your lips or fingernails turn gray or blue.
When should I call my doctor?
- Your symptoms do not get better, or get worse.
- You are urinating less, or not at all.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Community Acquired Pneumonia
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
