Pleural Effusion
Medically reviewed by Drugs.com. Last updated on May 6, 2024.
Pleural effusion is fluid buildup in the space between the layers of the pleura. The pleura is a thin piece of tissue with 2 layers. One layer rests directly on the lungs. The other rests on the chest wall. There is normally a small amount of fluid between these layers. This fluid helps your lungs move easily when you breathe.
 |
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
Keep the head of your bed raised to help you breathe easier.
You can also raise your head and shoulders on pillows or rest in a reclining chair. If you feel short of breath, let healthcare providers know right away.
Medicines:
- Cardiac medicines may be needed if your pleural effusion is caused by heart failure.
- Antibiotics help treat an infection caused by bacteria.
- NSAIDs help decrease swelling and pain or fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Steroids or other medicines may be given to decrease swelling.
- Cough medicine may be given to help loosen phlegm in your lungs and make it easier to cough up.
Tests:
- Blood tests may show signs of an infection.
- An x-ray, ultrasound, or CT may show fluid around your lungs, an enlarged heart, or signs of infection. You may be given contrast liquid to help your lungs show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
- A thoracentesis is a procedure to take fluid out of your chest through a needle put between your ribs. The fluid may be sent to a lab for tests.
- A sputum sample is collected in a cup when you cough. The sample is sent to a lab for tests.
- A biopsy is a procedure to remove a small piece of tissue from your lung or pleural lining. The tissue will be sent to a lab for tests. A biopsy may be taken with a needle, or through a small incision in your chest wall.
- A procedure to look inside your airway may be used to learn the cause of your pleural effusion. A bronchoscopy or video-assisted thoracic surgery (VATS) may be used. These procedures use a thin tube with a light or a scope guided down to your lungs. Tissue and fluid may be collected and sent to a lab for tests.
Treatment:
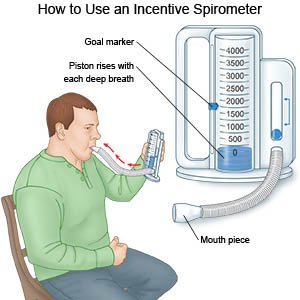
- Take deep breaths and cough 10 times each hour. This will decrease your risk for a lung infection. Take a deep breath and hold it for as long as you can. Let the air out and then cough strongly. Deep breaths help open your airway. You may be given an incentive spirometer to help you take deep breaths. Put the plastic piece in your mouth and take a slow, deep breath. Then let the air out and cough. Repeat these steps 10 times every hour.
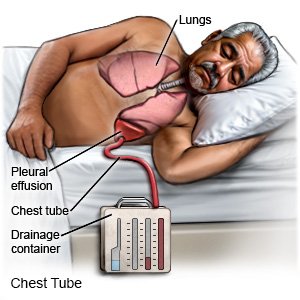
- Drainage of extra pleural fluid may be done using thoracentesis or a chest tube. A chest tube may stay in your chest for days or weeks. This allows the extra fluid around your lungs to drain over time. You may need medicines put directly into your chest if the fluid does not drain out easily.
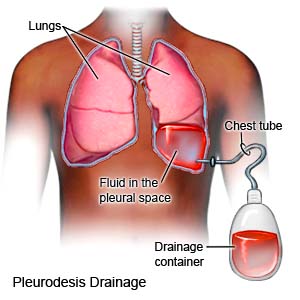
- Pleurodesis is a procedure that causes the 2 pleural layers to stick together. The extra fluid is drained from the pleural effusion through a tube. A medicine or chemical is put into the tube. The pleural layers become irritated and stick together, leaving no room for extra fluid. Pleurodesis may also be done during a thoracoscopy.
- A pleuroperitoneal shunt allows extra pleural fluid to drain into your abdomen. The fluid is then absorbed back into your body. A shunt is a thin, flexible tube that is placed underneath your skin. One end is in your pleural space, and the other is in your abdomen.
- Thoracotomy or other surgeries may be used to open the chest wall. Some conditions, such as cancer, may cause your pleural effusion to come back often. You may also need surgery to treat health problems caused by pleural effusion. Examples include surgery to remove scarring around the lung, or to remove part of the pleural lining.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
RISKS:
A pleural effusion may cause or worsen a lung infection, such as pneumonia. The pleural fluid may get infected and form a pocket of pus, called empyema. You may have other health problems, such as a collapsed lung.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Pleural Effusion
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
