Etanercept
Pronunciation: ee-TAN-er-sept
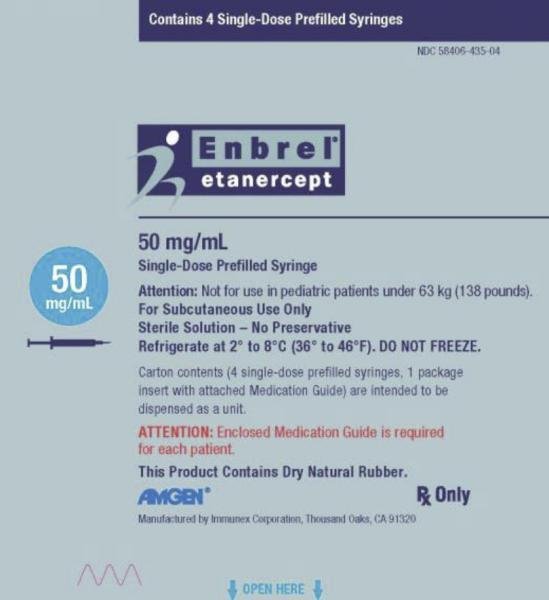
Generic name: Etanercept
Brand name: Enbrel
Dosage form: subcutaneous injection
Drug classes: Antirheumatics, TNF alfa inhibitors
What is etanercept?
Etanercept (Enbrel) is a TNF blocker used to treat plaque psoriasis, rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, or polyarticular juvenile idiopathic arthritis in specific patients. Etanercept works by decreasing tumor necrosis factor (TNF), a protein produced by the immune system to help the body fight infections. In people with autoimmune disorders, the immune system produces too much TNF and mistakenly attacks healthy cells.
Etanercept is FDA-approved to treat specific types of:
- plaque psoriasis in patients 4 years and older
- rheumatoid arthritis
- psoriatic arthritis
- ankylosing spondylitis
- polyarticular juvenile idiopathic arthritis in patients 2 years or older.
Etanercept became an FDA-approved medicine on November 2, 1998.
Etanercept side effects
Common Etanercept side effects
- pain, swelling, itching, or redness where the medicine was injected;
- headache; or
- cold symptoms such as stuffy nose, sneezing, sore throat.
Serious Etanercept side effects
Get emergency medical help if you have signs of an allergic reaction to etanercept hives, difficulty breathing, or swelling of your face, lips, tongue, or throat.
Serious and sometimes fatal infections may occur. Call your doctor right away if you have signs of infection such as fever, chills, cough, sweating, body aches, skin sores or redness, diarrhea, weight loss, burning when you urinate, coughing up blood, or feeling very tired or short of breath.
Also call your doctor at once if you have:
- fever, chills, flu symptoms;
- pale skin, easy bruising or bleeding;
- pain, redness, or swelling where etanercept was injected (for longer than 5 days after injection);
- signs of lymphoma - fever, night sweats, weight loss, stomach pain or swelling, swollen glands (in your neck, armpits, or groin);
- signs of tuberculosis - cough, night sweats, loss of appetite, weight loss, feeling very tired;
- new or worsening psoriasis - skin redness or scaly patches, raised bumps filled with pus;
- nerve problems - dizziness, numbness or tingling, problems with vision, or weak feeling in your arms or legs;
- signs of heart failure - shortness of breath, swelling in your lower legs;
- lupus-like syndrome - joint pain or swelling, chest discomfort, feeling short of breath, skin rash on your cheeks or arms (worsens in sunlight); or
- liver problems - right-sided upper stomach pain, vomiting, tiredness, loss of appetite, yellowing of your skin or eyes.
This is not a complete list of side effects, and others may occur. Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Warnings
Using etanercept may increase your risk of developing certain types of cancer, including a rare type of lymphoma. Ask your doctor about your specific risk. This has occurred mainly in teenagers and young adults using etanercept or similar medicines to treat Crohn's disease or ulcerative colitis. Call your doctor at once if you have any of the following symptoms: fever, night sweats, itching, loss of appetite, weight loss, tiredness, feeling full after eating only a small amount, pain in your upper stomach that may spread to your shoulder, nausea, easy bruising or bleeding, pale skin, feeling light-headed or short of breath, rapid heart rate, dark urine, clay-colored stools, or jaundice (yellowing of the skin or eyes).
Etanercept can weaken your immune system. Serious and sometimes fatal infections may occur. Call your doctor right away if you have signs of infection such as fever, chills, cough, sweating, body aches, skin sores or redness, diarrhea, burning when you urinate, or feeling very tired or short of breath.
Before taking this medicine
You should not use etanercept if you are allergic to it or if you have a severe infection such as sepsis (infection throughout your body).
To make sure etanercept is safe for you, tell your doctor if you have:
- a weak immune system, HIV or AIDS, tuberculosis, or any type of recurring infection;
- symptoms of an active infection such as fever, flu symptoms, diarrhea, or painful urination;
- an open cut or skin sores;
- diabetes;
- congestive heart failure;
- a history of nerve disorders such as multiple sclerosis, Guillain-Barré syndrome, myelitis, or optic neuritis;
- epilepsy or other seizure disorder;
- asthma or other breathing disorder;
- if you have ever had hepatitis B;
- if you are allergic to latex rubber; or
- if you are scheduled to receive any vaccines, or if you have recently been vaccinated with BCG (Bacille Calmette-Guerin).
Tell your doctor if you have ever had tuberculosis, were exposed to tuberculosis indicated by a positive PPD test, if anyone in your household has tuberculosis, or if you have recently traveled to an area where certain infections are common (Ohio River Valley, Mississippi River Valley, and the Southwest).
Children should be current on all childhood immunizations before starting treatment with etanercept.
Using etanercept may increase your risk of developing certain types of cancer, including a fast-growing lymphoma that can be fatal. This rare lymphoma has occurred in male teenagers and young men using a combination of immunosuppressant medicines to treat Crohn's disease or ulcerative colitis. However, people with autoimmune disorders (including rheumatoid arthritis, Crohn's disease, ankylosing spondylitis, and psoriasis) may have a higher risk of lymphoma. Talk to your doctor about your individual risk.
Pregnancy
Tell your doctor if you are pregnant or plan to become pregnant while using this medicine. If you are pregnant, your name may be listed on a pregnancy registry. This is to track the outcome of the pregnancy and to evaluate any effects of etanercept on the baby.
Breastfeeding
Etanercept can pass into breast milk and may harm a nursing baby. You should not breastfeed while using this medicine.
How should I use etanercept?
Before you start treatment with etanercept, your doctor may perform tests to make sure you do not have an infection.
Etanercept is injected under the skin (subcutaneous injection). A healthcare provider may teach you how to use the medication by yourself properly. Read and carefully follow any Instructions for Use provided with your medicine. Ask your doctor or pharmacist if you don't understand all instructions.
Do not shake this medicine. Prepare an injection only when you are ready to give it. Do not use it if the medicine looks cloudy, has changed colors, or has particles in it. Call your pharmacist for new medicine.
You may need to mix etanercept with a liquid (diluent). When using injections by yourself, be sure you understand how to mix and store the medicine properly.
Etanercept doses are based on weight in children. Your child's dose needs may change if the child gains or loses weight.
If you need surgery, tell the surgeon ahead of time that you are using this medicine
Etanercept affects your immune system, and so you may get infections more easily, even serious or fatal infections. Your doctor will need to examine you on a regular basis.
If you've ever had hepatitis B, using etanercept can cause this virus to become active or get worse. You may need frequent liver function tests while using this medicine and for several months after you stop.
Each cartridge, injection pen, or prefilled syringe is for one use only. Throw it away after one use, even if there is still medicine left inside.
Use a needle and syringe only once and then place them in a puncture-proof "sharps" container. Follow state or local laws about how to dispose of this container. Keep it out of the reach of children and pets.
Dosage Information
Usual adult etanercept dose for rheumatoid arthritis (RA) Ankylosing Spondylitis (AS), or psoriatic arthritis (PsA)
Dose: 50 mg once weekly with or without methotrexate.
Comments:
- Methotrexate, glucocorticoids, salicylates, nonsteroidal anti-inflammatory drugs (NSAIDs), or analgesics may be continued during therapy with this drug.
- Doses higher than 50 mg per week are not recommended.
Uses:
- Rheumatoid arthritis: To reduce symptoms, induce major clinical response, inhibit the progression of structural damage, and improve physical function in patients with moderately to severely active RA; this drug can be used alone or in combination with methotrexate.
- Ankylosing spondylitis: To reduce symptoms in patients with active AS.
- Psoriatic arthritis: To reduce symptoms, inhibiting the progression of structural damage of active arthritis, and improving physical function in patients with PsA; this drug can be used alone or in combination with methotrexate.
Usual Pediatric etanercept Dose for Juvenile Idiopathic Arthritis:
Dose: 2 years and older:
- Less than 63 kg: 0.8 mg/kg subcutaneously once a week.
- Greater than or equal to 63 kg: 50 mg subcutaneously once a week.
- Maximum dose: 50 mg subcutaneously once a week.
Comments:
- Glucocorticoids, nonsteroidal anti-inflammatory drugs (NSAIDs), or analgesics may be continued during treatment with this drug.
Use: For reducing symptoms of moderately to severely active polyarticular juvenile idiopathic arthritis (JIA) in patients 2 years and older.
Usual Pediatric etanercept Dose for Plaque Psoriasis:
Dose: 4 years and older:
- Less than 63 kg: 0.8 mg/kg subcutaneously once a week.
- Greater than or equal to 63 kg: 50 mg subcutaneously once a week.
- Maximum: 50 mg subcutaneously once a week.
Comments:
- Glucocorticoids, nonsteroidal anti-inflammatory drugs (NSAIDs), or analgesics may be continued during treatment with this drug.
Use: For the treatment of patients 4 years and older with chronic moderate to severe plaque psoriasis (PsO) who are candidates for systemic therapy or phototherapy.
What happens if I miss a dose?
Call your doctor for instructions if you miss a dose of etanercept..
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while using etanercept?
Avoid being near people who are sick or have infections. Call your doctor for preventive treatment if you are exposed to chicken pox.
Do not receive a "live" vaccine while using etanercept. The vaccine may not work as well during this time, and may not fully protect you from disease. Live vaccines include measles, mumps, rubella (MMR), polio, rotavirus, one form of typhoid, yellow fever, varicella (chickenpox), the older form of the shingles vaccine, and nasal flu (influenza) vaccine.
What other drugs will affect etanercept?
Tell your doctor about all your current medicines and any you start or stop using, especially:
- abatacept (Orencia);
- anakinra (Kineret);
- cyclophosphamide (Cytoxan); or
- insulin or oral diabetes medicine.
This list is not complete. Other drugs may interact with etanercept, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed in this medication guide.
Ingredients
Enbrel Brand
Active Ingredient: etanercept
Inactive Ingredients:
Single-dose Prefilled Syringe, Single-dose Prefilled SureClick Autoinjector, Single-dose Vial and Enbrel Mini single-dose cartridge: L-arginine hydrochloride, sodium chloride, and sucrose
Multiple-dose Vial: mannitol, sucrose, tromethamine
Storage
Carefully follow all storage instructions provided with your medicine.
For Enbrel brand.
- Store in the refrigerator at 36°F to 46°F (2°C to 8°C).
- Store in the original carton to protect from light or physical damage.
- If needed, you may store the prefilled syringe or the unmixed multiple-dose vial and diluent syringe (dose tray) at room temperature between 68°F to 77°F (20°C to 25°C) for up to 14 days.
- Once an prefilled syringe or an unmixed multiple-dose vial has reached room temperature, do not put it back in the refrigerator.
- Throw away any that has been stored at room temperature after 14 days.
- A mixed (reconstituted) multiple-dose vial should be used right away or kept in the refrigerator at 36°F to 46°F (2°C to 8°C) for up to 14 days.
- Do not store the in extreme heat or cold. For example, avoid storing in your vehicle’s glove box or trunk.
- Do not use after the expiration date on the label has passed.
- Do not freeze.
- Do not shake.
Company
Enbrel Brand
Amgen
Manufactured by:
Immunex Corporation, Thousand Oaks, CA 91320-1799.
Popular FAQ
Does perispinal etanercept work for stroke recovery?
There is good evidence that perispinal administration of etanercept works extremely well for stroke recovery, with the publication of the first RCT in 2019 that supported thousands of individual case reports of a beneficial effect. Improvements in chronic post-stroke symptoms with etanercept is usually rapid and long-lasting. Perispinal etanercept was first developed as a treatment for poststroke symptoms by Dr. Edward Tobinick, in 2010. Continue reading
How long does it take for Enbrel (etanercept) to work?
Enbrel starts to have some effect within one to two weeks, although it may take 3 to 6 months for the full effects to develop. Continue reading
How long can Enbrel (etanercept) be left unrefrigerated?
Enbrel may be left unrefrigerated for up to 14 days, as long as it is protected from light and not exposed to heat. Once Enbrel has been taken out of the refrigerator for more than 15 minutes, do not put it back in the refrigerator. If Enbrel has not been used within 14 days of being taken out of the refrigerator, discard it. Continue reading
Can Enbrel (etanercept) be taken with antibiotics?
Yes, Enbrel can be taken with antibiotics if your doctor has prescribed these for you because you currently have a bacterial infection. However, if you develop a serious infection or sepsis, your doctor may stop Enbrel, either temporarily or permanently, while you are receiving treatment for the infection. Continue reading
Can you take Enbrel (etanercept) with a cold?
Yes, you can take Enbrel if you have a cold, but make sure you let your doctor know that you have a cold because he/she may wish to monitor your health while your cold symptoms are present, as you are at a higher risk of developing a more serious infection because you are taking Enbrel. Continue reading
More FAQ
- What are the new drugs for rheumatoid arthritis (RA)?
- What are the new drugs for plaque psoriasis?
- How many biosimilars have been approved in the United States?
- What are biologic drugs and how do they work?
More about etanercept
- Check interactions
- Compare alternatives
- Reviews (321)
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: antirheumatics
- Breastfeeding
Patient resources
- Etanercept-szzs advanced reading
- Etanercept-ykro (Advanced Reading)
- Etanercept Auto-Injectors
- Etanercept Prefilled Syringes
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.