Trexall Side Effects
Generic name: methotrexate
Medically reviewed by Drugs.com. Last updated on Feb 23, 2024.
Note: This document provides detailed information about Trexall Side Effects associated with methotrexate. Some dosage forms listed on this page may not apply specifically to the brand name Trexall.
Applies to methotrexate: oral solution, oral tablet.
Other dosage forms:
Important warnings
This medicine can cause some serious health issues
Serious side effects of Trexall
Along with its needed effects, methotrexate (the active ingredient contained in Trexall) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking methotrexate:
More common
- black, tarry stools
- bleeding gums
- blood in the urine or stools
- bloody vomit
- diarrhea
- increased heartbeat
- itching, rash, reddening of the skin
- joint pain
- nausea
- pinpoint red spots on the skin
- sores in the mouth or lips
- stomach pain
- swelling of the eyelids, face, lips, hands, feet, or lower legs
- swelling or inflammation of the mouth
- trouble breathing
- unusual bleeding or bruising
- vomiting
- yellow eyes or skin
Less common
- back pain
- bloody nose
- blurred vision
- body and muscle pain
- burning while urinating
- confusion
- continuing ringing, buzzing, or other unexplained noise in the ears
- cough or hoarseness
- cracked, dry, scaly skin
- dark urine
- dizziness
- drowsiness
- ear congestion
- fever or chills
- headache
- loss of appetite
- loss of hearing
- loss of voice
- lower back or side pain
- painful or difficult urination
- pale skin
- runny nose
- seizures
- sneezing
- sore throat
- stuffy or runny nose
- unusual tiredness or weakness
- weight loss
- white or brownish vaginal discharge
Incidence not known
- anxiety
- blistering, peeling, or loosening of the skin
- bloating
- blurred or change in vision
- changes in skin color
- confusion
- constipation
- decreased interest in sexual intercourse
- difficulty in moving
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- dry mouth
- dryness or soreness of the throat
- eye pain
- fruit-like breath odor
- heartburn
- inability to have or keep an erection
- increased hunger or thirst
- indigestion
- irritation in the mouth
- large, flat, blue, or purplish patches in the skin
- loss in sexual ability, desire, drive, or performance
- loss of consciousness
- menstrual problem
- night blindness
- pain in the chest or groin
- pain, redness, swelling, or tenderness in the arm or leg
- red skin lesions, often with a purple center
- red, wart-like spots on the skin
- sudden loss of coordination
- sudden onset of slurred speech
- swelling or soreness of the breasts
- swollen, painful, or tender lymph glands in the neck or armpit
- tingling or numbness in the hands, feet, or lips
Other side effects of Trexall
Some side effects of methotrexate may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- hair loss or thinning
Less common
- blemishes on the skin
- hard, red, swollen skin irritation
- pimples
For healthcare professionals
Applies to methotrexate: compounding powder, injectable powder for injection, injectable solution, intramuscular solution, oral liquid, oral solution, oral tablet, subcutaneous solution.
General
Frequently observed adverse reactions include ulcerative stomatitis, leukopenia, nausea, and abdominal distress. In addition, infections, malaise, fatigue, chills, fever, and dizziness are commonly reported adverse reactions.[Ref]
Cardiovascular
- Rare (0.01% to 0.1%): Pericardial effusion, pericarditis, pericardial tamponade
- Postmarketing reports: Thromboembolic events (including arterial thrombosis, cerebral thrombosis, deep vein thrombosis, retinal vein thrombosis, thrombophlebitis, and pulmonary embolus), pericarditis, pericardial effusion, hypotension, sudden death[Ref]
Dermatologic
- Common (1% to 10%): Rash, pruritus, dermatitis, alopecia, photosensitivity, burning of skin lesions
- Uncommon (0.1% to 1%): Allergic vasculitis, herpetiform eruptions of the skin, Stevens-Johnson´s syndrome, toxic epidermal necrolysis, increase in rheumatoid nodules, increased skin pigmentation, impaired wound healing
- Rare (0.01% to 0.1%): Increased nail pigment changes, photo-hypersensitivity, acne petechiae, depigmentation, urticaria, erythema multiforme, painful damage to psoriatic lesion, skin ulceration, onycholysis
- Very rare (less than 0.01%): Acute paronychia, telangiectasia, furunculosis, ecchymoses, hidradenitis
- Frequency not reported: Skin exfoliation / dermatitis exfoliative
- Postmarketing reports: Toxic epidermal necrolysis, Stevens-Johnson syndrome, exfoliative dermatitis, skin necrosis, and erythema multiforme, erythematous rashes, pruritus, alopecia, skin ulceration, accelerated nodulosis, urticaria, pigmentary changes, ecchymosis, telangiectasia, photosensitivity, acne, furunculosis[Ref]
Endocrine
- Postmarketing reports: Diabetes[Ref]
Gastrointestinal
- Very common (10% or more): Nausea/vomiting (10%), dyspepsia, abdominal pain
- Common (1% to 10%): Diarrhea, stomatitis, oral ulcers
- Uncommon (0.1% to 1%): Gastrointestinal ulcerations and bleeding
- Rare (0.01% to 0.1%): Pancreatitis, gingivitis, enteritis, melena
- Very rare (less than 0.01%): Toxic megacolon, hematemesis
- Frequency not reported: Anorexia
- Postmarketing reports: Hemorrhagic enteritis, intestinal perforation, gingivitis, pancreatitis, pharyngitis, hematemesis, melena, gastrointestinal ulceration[Ref]
Genitourinary
- Uncommon (0.1% to 1%): Vaginal inflammation and ulceration
- Rare (0.01% to 0.1%): Impotence, menstrual disorders
- Very rare (less than 0.01%): Loss of libido, formation of defective oocytes or sperm cells, transient oligospermia, infertility, vaginal discharge, vaginal bleeding, gynecomastia
- Frequency not reported: Vaginal discharge
- Postmarketing reports: Defective oogenesis or spermatogenesis, loss of libido, impotence, gynecomastia, menstrual dysfunction[Ref]
Hematologic
- Common (1% to 10%): Thrombocytopenia (platelet count less than 100,000/mm3), leukopenia (white blood cell count less than 3000/mm3), pancytopenia, anemia
- Uncommon (0.1% to 1%): Bone marrow depression, agranulocytosis, hematopoietic disorders
- Rare (0.01% to 0.1%): Megaloblastic anemia, hypotension
- Very rare (less than 0.01%): Hypogammaglobulinemia, aplastic anemia, lympho-proliferative disorder, neutropenia, lymphadenopathy, vasculitis
- Frequency not reported: Decreased hematocrit, eosinophilia
- Postmarketing reports: Aplastic anemia, lymphadenopathy, hypogammaglobulinemia[Ref]
Hepatic
- Very common (10% or more): Elevated liver function tests (15%)
- Uncommon (0.1% to 1%): Cirrhosis, fibrosis and fatty degeneration of the liver, decrease in serum albumin
- Rare (0.01% to 0.1%): Hepatotoxicity, acute hepatitis
- Very rare (less than 0.01%): Reactivation of chronic hepatitis, hepatic failure
- Postmarketing reports: Acute hepatitis, decreased serum albumin, fibrosis, cirrhosis, liver failure[Ref]
Immunologic
- Uncommon (0.1% to 1%): Anaphylactic-type reaction, allergic reactions, anaphylactic shock
- Very rare (less than 0.01%): Immuno-suppression
- Postmarketing reports: Anaphylaxis, anaphylactoid reactions, vasculitis[Ref]
Metabolic
- Uncommon (0.1% to 1%): Diabetes mellitus
- Postmarketing reports: Hyperglycemia[Ref]
Musculoskeletal
- Rare (0.01% to 0.1%): Osteoporosis, arthralgia, myalgia
- Very rare (less than 0.01%): Stress fracture
- Frequency not reported: Osteonecrosis of jaw (secondary to lymphoproliferative disorders)
- Postmarketing reports: Stress fracture, soft tissue necrosis, arthralgia, myalgia, osteoporosis[Ref]
Nervous system
- Common (1% to 10%): Dizziness, headache, fatigue, drowsiness
- Uncommon (0.1% to 1%): Convulsions, vertigo
- Rare (0.01% to 0.1%): Hemiparesis, paresis
- Very rare (less than 0.01%): Cerebral edema, acute aseptic meningitis with meningism (paralysis, vomiting), irritation, dysarthria, aphasia, lethargy, transient subtle cognitive dysfunction, dysarthria, unusual cranial sensations, pain, muscular asthenia, paresthesia/ hypoesthesia, changes in sense of taste (metallic taste)
- Frequency not reported: Encephalopathy/leukoencephalopathy
- Postmarketing reports: Headaches, drowsiness, blurred vision, speech impairment (including dysarthria and aphasia), transient cognitive dysfunction, mood alteration, unusual cranial sensations, paresis, encephalopathy, leukoencephalopathy, convulsions, spinal radiculopathy (with intrathecal use)[Ref]
Ocular
- Rare (0.01% to 0.1%): Severe visual disturbances
- Very rare (less than 0.01%): Conjunctivitis, impaired vision, retinopathy
- Frequency not reported: Eye discomfort
- Postmarketing reports: Optic neuropathy, blurred vision, ocular irritation, conjunctivitis, xerophthalmia[Ref]
Oncologic
- Uncommon (0.1% to 1%): Lymphoma[Ref]
Other
- Uncommon (0.1% to 1%): Chills
- Frequency not reported: Fever, infection, sweating, tinnitus[Ref]
Psychiatric
- Uncommon (0.1% to 1%): Depression, confusion
- Rare (0.01% to 0.1%): Mood swings
- Very rare (less than 0.01%): Insomnia[Ref]
Renal
- Uncommon (0.1% to 1%): Disturbed micturition, inflammation and ulceration of the urinary bladder (possibly with hematuria), renal insufficiency, nephropathy
- Rare (0.01% to 0.1%): Oliguria, anuria, electrolyte disturbances
- Very rare (less than 0.01%): Dysuria, azotemia, cystitis, hematuria, proteinuria
- Postmarketing reports: Azotemia, hematuria, proteinuria, cystitis[Ref]
Respiratory
- Common (1% to 10%): Interstitial pneumonitis
- Uncommon (0.1% to 1%): Nosebleed, interstitial fibrosis
- Rare (0.01% to 0.1%): Respiratory paralysis, dyspnea, pharyngitis, bronchial asthma
- Very rare (less than 0.01%): Chronic interstitial obstructive lung disease, pleuritis, dry cough, pleural effusion
- Frequency not reported: Upper respiratory infection, chest pain, coughing, epistaxis, alveolitis, pulmonary alveolar hemorrhage
- Postmarketing reports: Pulmonary fibrosis, respiratory failure, chronic interstitial obstructive pulmonary disease, pleuritic pain and thickening, alveolitis[Ref]
References
1. Cerner Multum, Inc. "UK Summary of Product Characteristics."
2. Cerner Multum, Inc. "Australian Product Information."
3. (2017) "Product Information. Methotrexate Sodium (methotrexate)." Teva Pharmaceuticals (formerly IVAX)
Frequently asked questions
- Why should I take folic acid with methotrexate?
- Does it cause weight gain?
- How long does it take to work?
- How do I know if methotrexate is working for rheumatoid arthritis?
- What are the different brands of methotrexate?
- How long does methotrexate stay in your system?
- What causes Plaque Psoriasis?
- How does methotrexate work for ectopic pregnancy?
More about Trexall (methotrexate)
- Check interactions
- Compare alternatives
- Pricing & coupons
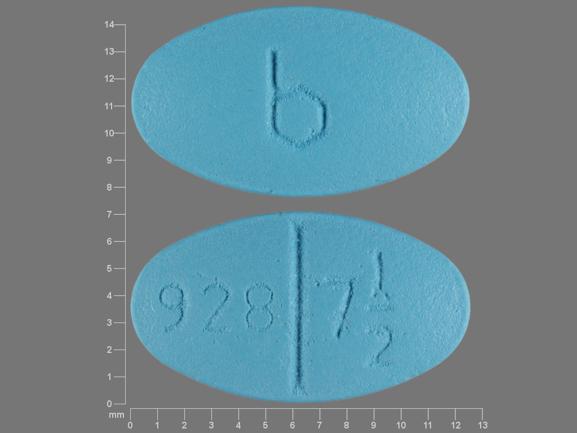
- Drug images
- Dosage information
- During pregnancy
- Drug class: antimetabolites
- Breastfeeding
- En español
Patient resources
Other brands
Otrexup, Rasuvo, Rheumatrex Dose Pack, Xatmep, ... +2 more
Professional resources
Other brands
Otrexup, Rasuvo, Rheumatrex Dose Pack, Xatmep, ... +2 more
Related treatment guides
Further information
Trexall side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.