Mirapex ER Side Effects
Generic name: pramipexole
Medically reviewed by Drugs.com. Last updated on Jul 13, 2024.
Note: This document provides detailed information about Mirapex ER Side Effects associated with pramipexole. Some dosage forms listed on this page may not apply specifically to the brand name Mirapex ER.
Applies to pramipexole: oral tablet, oral tablet extended release.
Precautions
It is very important that your doctor check your progress at regular visits. This is to allow for changes in your dose and to check for any unwanted effects.
Do not change your dose or Stop taking pramipexole (the active ingredient contained in Mirapex ER) without first checking with your doctor. Your doctor may want you to gradually reduce the amount you are taking before stopping it completely. Stopping this medicine suddenly may cause anxiety, discouragement, feeling sad or empty, irritability, lack of appetite, lack of feeling or emotion, loss of interest or pleasure, sweating, tiredness, trouble concentrating, trouble sleeping, uncaring, or unusual tiredness or weakness.
People taking pramipexole have reported falling asleep without warning during activities of daily living, including driving, which sometimes resulted in accidents. This may happen as late as one year after taking the medicine. Make sure you know how you react to this medicine before you drive, use machines, or do anything else that could be dangerous if you are not alert, well-coordinated, or able to think or see well.
Check with your doctor before using this medicine with alcohol or other medicines that affect the central nervous system (CNS). This medicine will add to the effects of alcohol and other CNS depressants (medicines that make you drowsy or less alert). Some examples of CNS depressants are antihistamines or medicine for hay fever or colds, sedatives, tranquilizers, or sleeping medicine, prescription pain medicine or narcotics, barbiturates or medicine for seizures, muscle relaxants, or anesthetics, including some dental anesthetics. .
Dizziness, lightheadedness, or fainting may occur, especially when you get up suddenly from a lying or sitting position. These symptoms are more likely to occur when you begin taking this medicine, or when the dose is increased. Getting up slowly may help. If you have this problem, talk to your doctor.
Hallucinations (seeing, hearing, or feeling things that are not there) may occur in some patients. This is more common with elderly patients. If you have hallucinations, check with your doctor.
This medicine may cause posture changes that you cannot control. Tell your doctor right away if you have your neck bending forward, bending forward at the waist, or tilting sideways when you sit, stand, or walk.
Check with your doctor right away if you have dark-colored urine, fever, muscle cramps or spasms, muscle pain or stiffness, or unusual tiredness or weakness. These may be symptoms of a condition called rhabdomyolysis (muscle disease that can lead to kidney problems).
Some people who have used this medicine had unusual changes in their thoughts or behavior, including an urge to gamble, spend money, binge eat, or an increased sex drive. Talk with your doctor if this is a concern for you.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Serious side effects of Mirapex ER
Along with its needed effects, pramipexole may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking pramipexole:
More common side effects
- dizziness, lightheadedness, or fainting, especially when standing up suddenly from a sitting/lying position
- drowsiness
- nausea
- seeing, hearing, or feeling things that are not there
- trouble sleeping
- twitching, twisting, or other unusual body movements
- unusual tiredness or weakness
Less common side effects
- chest tightness
- confusion
- cough
- difficulty with swallowing
- double vision or other changes in vision
- falling asleep without warning
- fearfulness, suspiciousness, or other mental changes
- fever
- frequent urination
- memory loss
- muscle or joint pain
- muscle weakness
- restlessness or need to keep moving
- swelling of the body
- trouble breathing
- writhing, twisting, or other unusual body movements
Rare side effects
- abnormal thinking
- anxiety
- bloody or cloudy urine
- chest pain
- difficult, burning, or painful urination
- dizziness
- frequent urge to urinate
- loss of bladder control
- swelling of the arms or legs
Incidence not known
- discouragement
- feeling sad or empty
- lack of appetite
- lack of feeling or emotion
- loss of interest or pleasure
- sweating
- trouble concentrating
- uncaring
Other side effects of Mirapex ER
Some side effects of pramipexole may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common side effects
- constipation
- dryness of the mouth
- headache
- heartburn, indigestion, or acid stomach
Less common side effects
- abnormal dreams
- decreased sexual drive or ability
- general feeling of discomfort or illness
- increased cough
- increased sweating
- joint pain
- loss of appetite
- runny nose
- skin rash, itching
- weight loss
See also:
For healthcare professionals
Applies to pramipexole: oral tablet, oral tablet extended release.
General adverse events
The most common adverse reactions occurring in early Parkinson's disease when used without levodopa were somnolence, insomnia, nausea, constipation, dizziness, fatigue, asthenia, hallucinations, dry mouth, muscle spasms, and peripheral edema. In advanced Parkinson's disease when used with levodopa, the more common adverse reactions included postural hypotension, dyskinesia, extrapyramidal syndrome, insomnia, abnormal dreams, confusion, asthenia, dystonia, somnolence, hypertonia, dry mouth, amnesia, urinary frequency, dizziness, nausea, constipation, hallucinations, headache, and anorexia.
The most common adverse reactions occurring in patients receiving treatment for Restless Legs Syndrome were nausea, somnolence, fatigue, and headache.[Ref]
Nervous system
Early Parkinson's disease:
- Very common (10% or more): Somnolence (up to 36%), dizziness (up to 25%), dyskinesia (17%)
- Common (1% to 10%): Headache, hypesthesia, dystonia, myoclonus, akathisia, tremor, balance disorder, amnesia, abnormal thinking
- Frequency not reported: Restlessness
Advanced Parkinson's disease:
- Very common (10% or more): Dyskinesia (up to 47%), extrapyramidal syndrome (28%), dizziness (up to 26%),
- Common (1% to 10%): Somnolence, dystonia, gait abnormalities, hypertonia, headache
Restless Legs Syndrome:
- Very common (10% or more): Augmentation (12%), headache (17%)
- Common (1% to 10%): Worsening of Restless Legs Syndrome, somnolence
- Uncommon (0.1% to 1%): Dyskinesia
- Postmarketing reports: Amnesia, hyperkinesia[Ref]
In a 26-week clinical trial, worsening of Restless Legs Syndrome (RLS) occurred in 10% of patients suddenly withdrawn from pramipexole (the active ingredient contained in Mirapex ER) 0.75 mg once a day compared to 2% of placebo patients; the RLS symptoms were generally considered mild. Augmentation was reported in 12% and 9% of patients receiving pramipexole 0.75 mg once a day and placebo, respectively. The incidence of augmentation increased with increasing duration of exposure.[Ref]
Psychiatric
Parkinson's disease:
- Very common (10% or more): Hallucinations (17%), insomnia (27%), dream abnormalities (11%), confusion (10%)
- Common (1% to 10%): Paranoid reaction, delusions, confusion, sleep attacks, sleep disorder, depression
- Uncommon (0.1% to 1%): Hypersexuality, pathological gambling, delirium
- Rare (less than 0.1%): Mania
- Frequency not reported: Impulse control/compulsive behaviors
- Postmarketing reports: New or worsening mental status and behavioral changes, binge eating, compulsive shopping
Restless Legs Syndrome:
- Very common (10% or more): Insomnia (up to 13%)
- Common (1% to 10%): Abnormal dreams
- Uncommon (0.1% to 1%): Hypersexuality, pathological gambling, delirium
- Rare (less than 0.1%): Mania
- Frequency not reported: Impulse control/compulsive behaviors
- Postmarketing reports: New or worsening mental status and behavioral changes, binge eating, compulsive shopping[Ref]
Gastrointestinal
- Very common (10% or more): Nausea (28%), constipation (14%)
- Common (1% to 10%): Dysphagia, dry mouth, diarrhea, dyspepsia, vomiting, upper abdominal pain, abdominal discomfort, salivary hypersecretion
- Uncommon (0.1% to 1%): Hiccup
- Frequency not reported: Hyperphagia
- Postmarketing reports: Peritoneal fibrosis[Ref]
Nausea and vomiting were commonly reported early in therapy and resolved with continued therapy. While there have been postmarketing reports of fibrotic complications including peritoneal fibrosis, pleural fibrosis, and pulmonary fibrosis, the evidence is not sufficient to establish a causal relationship with use of this drug; however a contribution of treatment cannot be completely ruled out.[Ref]
Cardiovascular
- Very common (10% or more): Postural hypotension (up to 53%)
- Common (1% to 10%): Chest pain, general edema
- Postmarketing reports: Cardia failure, syncope[Ref]
Cardiovascular side effects have included orthostatic hypotension, with or without symptoms, although the overall incidence was not significantly different from that in placebo-treated patients. In advanced Parkinson's disease trials, postural hypotension was reported in 53% (n=260) of patients receiving immediate-release pramipexole compared with 48% (n=264) of patients receiving placebo. In fixed-dose trials in early Parkinson's disease, orthostatic hypotension was shown to be dose related with a frequency 2-fold greater than placebo for doses greater than 1.5 mg/day. Among patients with advanced Parkinson's disease treated concomitantly with levodopa, orthostatic hypotension was reported much more frequently than in those with early disease and not receiving levodopa.
In a pharmacoepidemiology study, pramipexole use was associated with an increased risk of cardiac failure compared with non-use (observed risk ratio: 1.86; 95% confidence interval, 1.21 to 2.85).[Ref]
Genitourinary
- Common (1% to 10%): Urinary frequency, urinary tract infection, urinary incontinence, impotence[Ref]
Musculoskeletal
- Common (1% to 10%): Arthritis, twitching, bursitis, myasthenia, extremity pain, back pain, muscle spasms, increased creatine phosphokinase
- Very rare (less than 0.01%): Rhabdomyolysis
- Postmarketing reports: Postural deformity[Ref]
One case of rhabdomyolysis occurred in a 49- year old male patient with advanced Parkinson's disease receiving pramipexole (the active ingredient contained in Mirapex ER). His creatinine phosphokinase level was elevated to 10,631 IU/L. His symptoms resolved with discontinuation of the medication.[Ref]
Ocular
- Common (1% to 10%): Vision abnormalities, accommodation abnormalities, diplopia,
- Frequency not reported: Blurred vision[Ref]
Dermatologic
- Common (1% to 10%): Skin disorders
- Frequency not reported: Pruritus
- Postmarketing reports: Skin reactions (including erythema, rash, pruritus, urticaria)[Ref]
Respiratory
- Common (1% to 10%): Dyspnea, rhinitis, pneumonia, nasal congestion, cough
- Uncommon (0.1% to 1%): Pneumonia
- Postmarketing reports: Pleural fibrosis, pulmonary fibrosis[Ref]
There have been postmarketing reports of fibrotic complications including peritoneal fibrosis, pleural fibrosis, and pulmonary fibrosis, the evidence is not sufficient to establish a causal relationship with use of this drug; however a contribution of treatment cannot be completely ruled out.[Ref]
Metabolic
- Common (1% to 10%): Decreased weight, increased appetite, anorexia
- Postmarketing reports: Increased weight[Ref]
Other
- Very common (10% or more): Asthenia (up to 14%)
- Common (1% to 10%): Malaise, fever, vertigo[Ref]
Endocrine
- Frequency not reported: Libido disorders
- Postmarketing reports: Inappropriate antidiuretic hormone secretion (SIADH)[Ref]
Hypersensitivity
- Frequency not reported: Rash and other hypersensitivity reactions[Ref]
Immunologic
- Common (1% to 10%): Influenza[Ref]
References
1. (2001) "Product Information. Mirapex (pramipexole)." Boehringer Ingelheim
2. Cerner Multum, Inc. "UK Summary of Product Characteristics."
3. Cerner Multum, Inc. "Australian Product Information."
4. (2015) "Product Information. Mirapex ER (pramipexole)." Boehringer Ingelheim
More about Mirapex ER (pramipexole)
- Check interactions
- Compare alternatives
- Reviews (8)
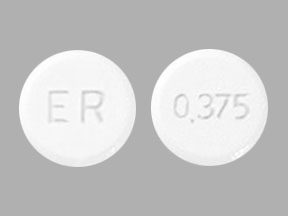
- Drug images
- Dosage information
- During pregnancy
- Drug class: dopaminergic antiparkinsonism agents
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Mirapex ER side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.