Lamictal ODT Side Effects
Generic name: lamotrigine
Medically reviewed by Drugs.com. Last updated on Sep 3, 2024.
Note: This document provides detailed information about Lamictal ODT Side Effects associated with lamotrigine. Some dosage forms listed on this page may not apply specifically to the brand name Lamictal ODT.
Applies to lamotrigine: oral tablet, oral tablet chewable, oral tablet disintegrating, oral tablet extended release.
Important warnings
This medicine can cause some serious health issues
Oral route (tablet; tablet, chewable; tablet, disintegrating; tablet, extended release)
Cases of life-threatening serious rashes, including Stevens-Johnson syndrome and toxic epidermal necrolysis, or rash-related death have been caused by lamotrigine.
The rate of serious rash is greater in pediatric patients than in adults.
Additional factors that may increase the risk of rash include: (1) coadministration with valproate; (2) exceeding recommended initial dose of lamotrigine; or (3) exceeding recommended dose escalation for lamotrigine.
Benign rashes are also caused by lamotrigine; however, it is not possible to predict which rashes will prove to be serious or life threatening.
Lamotrigine should be discontinued at the first sign of rash, unless the rash is clearly not drug related.
Serious side effects of Lamictal ODT
Along with its needed effects, lamotrigine (the active ingredient contained in Lamictal ODT) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking lamotrigine:
More common
- blurred vision
- changes in vision
- chest pain, discomfort, or tightness
- clumsiness or unsteadiness
- decreased urine output
- dilated neck veins
- double vision
- irregular breathing
- irregular heartbeat
- nausea
- pain or discomfort in the arms, jaw, back, or neck
- poor coordination
- seizure that will not stop
- skin rash
- sweating
- swelling of the face, fingers, feet, or lower legs
- trouble breathing
- unusual tiredness or weakness
- vomiting
- weight gain
Less common
- anxiety
- chest pain
- confusion
- continuous, uncontrolled back and forth or rolling eye movements
- depression
- increase in seizures
- infection
- irritability
Rare
- blistering, peeling, or loosening of the skin
- chills
- cough
- dark urine
- diarrhea
- fever
- general feeling of discomfort or illness
- headache
- itching
- joint pain
- loss of appetite
- memory loss
- muscle cramps, pain, or weakness
- red or irritated eyes
- runny nose
- shivering
- small red or purple spots on the skin
- sore throat
- sores, ulcers, or white spots on the lips or in the mouth
- swelling of the face, mouth, hands, or feet
- swollen lymph nodes
- trouble sleeping
- unusual bleeding or bruising
- yellow eyes or skin
Incidence not known
- back, leg, or stomach pains
- bleeding gums
- bloating
- blood in the urine
- bloody, black or tarry stools
- bluish lips or skin
- constipation
- cough
- coughing or vomiting blood
- difficulty with swallowing
- fainting
- fast heartbeat
- general body swelling
- heartburn
- high fever
- hoarseness
- lightheadedness
- loss of balance control
- lower back or side pain
- mask-like face
- muscle spasms
- nosebleeds
- not breathing
- pain or burning in the throat
- painful or difficult urination
- pains in the stomach or side, possibly radiating to the back
- pale skin
- persistent bleeding or oozing from puncture sites, mouth, or nose
- rapid, shallow breathing
- redness, soreness, or itching skin
- shuffling walk
- slowed movement
- slurred speech
- sores, welting, or blisters
- stiffness of the arms and legs
- swollen or painful glands
- tic-like (jerky) movements
Get emergency help immediately if any of the following symptoms of overdose occur while taking lamotrigine:
Symptoms of overdose
- clumsiness or unsteadiness (severe)
- continuous, uncontrolled back and forth or rolling eye movements (severe)
- dizziness (severe)
- drowsiness (severe)
- dryness of the mouth (severe)
- headache (severe)
- increased heart rate
- loss of consciousness
- slurred speech (severe)
Other side effects of Lamictal ODT
Some side effects of lamotrigine may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- dizziness
- drowsiness
Less common
- indigestion
- loss of strength
- menstrual pain
- pain
- trembling or shaking
- trouble with sleeping
- unusual weight loss
For healthcare professionals
Applies to lamotrigine: oral tablet, oral tablet disintegrating, oral tablet dispersible, oral tablet extended release.
General
The more commonly reported adverse reactions have included dizziness, headache, diplopia, ataxia, nausea, blurred vision, somnolence, and rash.[Ref]
Immunologic
- Postmarketing reports: Progressive immunosuppression, Lupus-like reaction, vasculitis, drug reaction with eosinophilia and systemic symptoms (DRESS), hemophagocytic lymphohistiocytosis (HLH)[Ref]
In cases of hemophagocytic lymphohistiocytosis (HLH), patients have presented with signs of systemic inflammation (fever, rash, hepatosplenomegaly, and organ system dysfunction) and blood dyscrasias. Symptoms have been reported within 8 to 24 days.[Ref]
Hypersensitivity
- Uncommon (0.1% to 1%): Allergic reaction, chills, malaise[Ref]
Nervous system
- Very common (10% or more): Dizziness (38%), headache (29%), ataxia (22%), somnolence (14%)
- Common (1% to 10%): Seizure exacerbation, incoordination, insomnia, tremor, speech disorder, amnesia, hypoesthesia, pain, gait abnormality, vertigo, dyspraxia, confusion, paresthesia
- Uncommon (0.1% to 1%): Akathisia, aphasia, central nervous system depression, dysarthria, dyskinesia, hyperkinesia, hypertonia, movement disorder, myoclonus, sudden unexplained death in Epilepsy (SUDEP)
- Rare (less than 0.1%): Choreoathetosis, dystonia, extrapyramidal syndrome, faintness, grand mal seizures, hemiplegia, hyperalgesia, hyperesthesia, hypokinesia, hypotonia, neuralgia, muscle spasm, neuralgia, paralysis, peripheral neuritis
- Very rare (less than 0.01%): Muscle spasm, paralysis, peripheral neuritis
- Postmarketing reports: Exacerbation of Parkinsonian symptoms in patients with pre-existing Parkinson's disease, tics[Ref]
Sudden unexplained death in epilepsy (SUDEP) was reported in 20 of 4700 patients with epilepsy during premarketing development. While this exceeds the expected rate in healthy populations, it is within the range for patients with epilepsy.[Ref]
Psychiatric
- Common (1% to 10%): Depression, anxiety, irritability, disturbance of concentration, emotional lability, abnormal thinking, nervousness
- Uncommon (0.1% to 1%): Apathy, euphoria, hallucinations, hostility, depersonalization, memory decrease, mind racing, panic attack, paranoid reaction, personality disorder, psychosis, sleep disorder, stupor, suicidal ideation
- Rare (less than 0.1%): Delirium, delusions, dysphoria, manic depression reaction, neurosis
- Postmarketing reports: Aggression, nightmares[Ref]
Antiepileptic drugs (AEDs) increase the risk of suicidal thoughts or behavior. Pooled analyses of 199 placebo-controlled clinical trials of 11 different AEDs (monotherapy or adjunctive therapy) showed twice the risk compared with placebo patients; an estimated incidence of 0.43% (n=27,863) in AED-treated patients compared to 0.24% (n=16,029) in placebo. The median treatment duration was 12 weeks. There were 4 suicides in AED-treated patients (placebo=0). The risk of suicidal thoughts or behavior was considered similar among the drugs studied despite their varying mechanisms of action suggesting the risk applies to all AEDs used for any indication. Additionally, the risk did not vary substantially by age.[Ref]
Ocular
- Very common (10% or more): Diplopia (28%), blurred vision (16%)
- Common (1% to 10%): Vision abnormality, nystagmus, photosensitivity, amblyopia
- Uncommon (0.1% to 1%): Abnormality of accommodation, conjunctivitis, dry eyes, photophobia
- Rare (less than 0.1%): Lacrimation disorder, oscillopsia, ptosis, strabismus, uveitis, visual field defect[Ref]
Gastrointestinal
- Very common (10% or more): Vomiting (20%), nausea (19%), diarrhea (10%)
- Common (1% to 10%): Abdominal pain, vomiting, dyspepsia, constipation, anorexia, dry mouth, rectal hemorrhage, peptic ulcer, flatulence
- Uncommon (0.1% to 1%): Dysphagia, eructation, gastritis, gingivitis, increased appetite, increased salivation, mouth ulceration
- Rare (less than 0.1%): Gastrointestinal hemorrhage, glossitis, gum hemorrhage, gum hyperplasia, hematemesis, hemorrhagic colitis, melena, stomach ulcer, stomatitis, tongue edema
- Very rare (less than 0.01%): Pancreatitis, esophagitis[Ref]
Respiratory
- Very common (10% or more): Rhinitis (14%)
- Common (1% to 10%): Pharyngitis, increased cough, epistaxis, dyspnea, bronchitis, sinusitis, bronchospasm
- Uncommon (0.1% to 1%): Yawn
- Rare (less than 0.1%): Hiccup, hyperventilation
- Postmarketing reports: Apnea[Ref]
Dermatologic
- Very common (10% or more): Rash (14%)
- Common (1% to 10%): Contact dermatitis, dry skin, sweating, eczema, pruritus
- Uncommon (0.1% to 1%): Acne, alopecia, hirsutism, maculopapular rash, skin discoloration, urticaria
- Rare (less than 0.1%): Angioedema, erythema, exfoliative dermatitis, fungal dermatitis, herpes zoster, leukoderma, multiforme erythema, petechial rash, pustular rash, Stevens-Johnson syndrome, vesiculobullous rash[Ref]
In adult patients (n=3348), serious rash associated with hospitalization and discontinuation was reported in 0.3% of patients in premarketing epilepsy trials. In bipolar trials, serious rash occurred in 0.08% of patients receiving this drug as initial monotherapy and 0.13% of patients receiving this drug as adjunctive therapy. In worldwide postmarketing experience, rash-related death has been reported, but the numbers are too few to permit a precise estimate of rate.
In a prospectively followed cohort of pediatric patients 2 to 17 years old, the incidence of serious rash was approximately 0.3% to 0.8%. In a prospectively followed cohort of patients 2 to 16 years old (n=1983), 1 rash-related death occurred in a patient with epilepsy taking this drug as adjunctive therapy.
Evidence has show the inclusion of valproate in a multidrug regimen increases the risk of serious, potentially life-threatening rash in both adult and pediatric patients. In pediatric patients who used valproate concomitantly for epilepsy, 1.2% (6 of 482) experienced a serious rash (placebo=0.6%). In adults, 1% of patients of patients receiving this drug in combination with valproate (n=584) experienced a rash (placebo=0.16%).[Ref]
Genitourinary
- Common (1% to 10%): Dysmenorrhea, vaginitis, amenorrhea, libido increase, urinary tract infection (both male and female), urinary frequency
- Uncommon (0.1% to 1%): Libido decreased, abnormal ejaculation, hematuria, impotence, menorrhagia, polyuria, urinary incontinence
- Rare (less than 0.1%): Anorgasmia, breast abscess, breast neoplasm, creatinine increase, cystitis, dysuria, epididymitis, female lactation, nocturia, urinary retention, urinary urgency[Ref]
Other
- Very common (10% or more): Fever (15%), accidental injury (14%)
- Common (1% to 10%): Fatigue
- Uncommon (0.1% to 1%): Ear pain, taste perversion, tinnitus
- Rare (less than 0.1%): Alcohol intolerance, deafness, taste loss, parosmia, taste loss[Ref]
Metabolic
- Common (1% to 10%): Weight decrease, weight gain, peripheral edema, facial edema
- Rare (less than 0.1%): Bilirubinemia, general edema, gamma glutamyl transpeptidase increase, hyperglycemia[Ref]
Musculoskeletal
- Common (1% to 10%): Neck pain, arthralgia, myalgia, decreased reflexes, back pain, increased reflexes, asthenia
- Uncommon (0.1% to 1%): Arthritis, leg cramps, myasthenia, twitching
- Rare (less than 0.1%): Bursitis, muscle atrophy, pathological fracture, tendinous contracture
- Postmarketing reports: Rhabdomyolysis (among patients experiencing hypersensitivity reactions)[Ref]
Cardiovascular
- Common (1% to 10%): Chest pain, migraine
- Uncommon (0.1% to 1%): Flushing, hot flashes, hypertension, palpitations, postural hypotension, syncope, tachycardia, vasodilation[Ref]
Hematologic
- Uncommon (0.1% to 1%): Leukopenia
- Rare (less than 0.1%): Anemia, eosinophilia, fibrin decrease, fibrinogen decrease, iron deficiency anemia, leukocytosis, lymphocytosis, macrocytic anemia, ecchymosis, thrombocytopenia
- Postmarketing reports: Agranulocytosis, hemolytic anemia, lymphadenopathy not associated with hypersensitivity disorder[Ref]
Hepatic
- Common (1% to 10%): Lymphadenopathy
- Uncommon (0.1% to 1%): Liver function tests abnormal, aspartate transaminase (AST) increased
- Rare (less than 0.1%): Hepatitis, alanine transaminase ALT) increased, acute kidney failure, kidney failure, kidney pain[Ref]
References
1. (2018) "Product Information. LaMICtal XR (lamotrigine)." GlaxoSmithKline
2. (2001) "Product Information. Lamictal (lamotrigine)." Glaxo Wellcome
3. Cerner Multum, Inc. "UK Summary of Product Characteristics."
4. Pharmaceutical Society of Australia (2006) APPGuide online. Australian prescription products guide online. http://www.appco.com.au/appguide/default.asp
5. Wadelius M, Karlsson T, Wadelius C (1996) "Lamotrigine and toxic epidermal necrolysis." Lancet, 348, p. 1041
6. Chaffin JJ, Davis SM (1997) "Suspected lamotrigine-induced toxic epidermal necrolysis." Ann Pharmacother, 31, p. 720-3
7. Sachs B, Ronnau AC, Ruzicka T, Gleichmann E, Schuppe HC (1996) "Lamotrigine and toxic epidermal necrolysis." Lancet, 348, p. 1597
8. Page RL, ONeil MG, Yarbrough DR, Conradi S (1998) "Fatal toxic epidermal necrolysis related to lamotrigine administration." Pharmacotherapy, 18, p. 392-8
9. Hilas O, Charneski L (2007) "Lamotrigine-induced Stevens-Johnson syndrome." Am J Health Syst Pharm, 64, p. 273-275
10. Mikati MA, Schachter SC, Schomer DL, Keally M, Osborne-Shafer P, Seaman CA, Sheridan PH, Ashworth M, Kupferberg H, Valakas A, et al. (1989) "Long-term tolerability, pharmacokinetic and preliminary efficacy study of lamotrigine in patients with resistant partial seizures." Clin Neuropharmacol, 12, p. 312-21
11. Boot B (2009) "Recurrent lamotrigine-induced aseptic meningitis." Epilepsia, 50, p. 968-9
12. Margolese HC, Beauclair L, Szkrumelak N, Chouinard G (2003) "Hypomania Induced by Adjunctive Lamotrigine." Am J Psychiatry, 160, p. 183-184
13. Mueller TH, Beeber AR (2004) "Delirium From Valproic Acid With Lamotrigine." Am J Psychiatry, 161, p. 1128-1129
14. Uher R, Jones HM (2006) "Hallucinations during lamotrigine treatment of bipolar disorder." Am J Psychiatry, 163, p. 749-50
15. Desarkar P, Sinha VK (2006) "Lamotrigine-induced severe manic switch." Aust N Z J Psychiatry, 40, p. 718
16. Verma A, Miller P, Carwile ST, Husain AM, Radtke (1999) "Lamotrigine-induced blepharospam." Pharmacotherapy, 19, p. 877-80
17. Saravanan N, Musibay Otaiku O, Namushi Namushi R (2005) "Interstitial pneumonitis during lamotrigine therapy." Br J Clin Pharmacol, 60, p. 666-7
18. Hillemacher T, Bleich S, Kornhuber J, Frieling H (2006) "Hair loss as a side effect of lamotrigine treatment." Am J Psychiatry, 163, p. 1451
19. Schwartz R, Avello E, Palisson F (2008) "Lamotrigine-induced toxic epidermal necrolysis treated with intravenous immunoglobulin and amniotic membranes." Arch Dermatol, 144, p. 724-6
20. Avoni P, Contin M, Riva R, Albani F, Liguori R, Baruzzi A (2001) "Dysgeusia in epileptic patients treated with lamotrigine: Report of three cases." Neurology, 57, p. 1521
21. Bowden CL, Calabrese JR, Ketter TA, Sachs GS, White RL, Thompson TR (2006) "Impact of lamotrigine and lithium on weight in obese and nonobese patients with bipolar I disorder." Am J Psychiatry, 163, p. 1199-201
22. FDA. U.S Food & Drug Administration (2018) FDA Drug Safety Communication: FDA warns of serious immune system reaction with seizure and mental health medicine lamotrigine (Lamictal) https://www.fda.gov/Drugs/DrugSafety/ucm605470.htm?utm_campaign=New%20FDA%20Drug%20Safety%20Communication%20on%20Lam
23. Esfahani FE, Dasheiff RM (1997) "Anemia associated with lamotrigine." Neurology, 49, p. 306-7
24. Fadul CE, Meyer LP, Jobst BC, Cornell CJ, Lewis LD (2002) "Agranulocytosis Associated with Lamotrigine in a Patient with Low-grade Glioma." Epilepsia, 43, p. 199-200
25. Moeller KE, Wei L, Jewell AD, Carver LA (2008) "Acute hepatotoxicity associated with lamotrigine." Am J Psychiatry, 165, p. 539-40
26. Ouellet G, Tremblay L, Marleau D (2009) "Fulminant hepatitis induced by lamotrigine." South Med J, 102, p. 82-4
Frequently asked questions
- Is it better to take lamotrigine at night?
- What should I do if I develop a rash while taking lamotrigine?
- If you are taking lamotrigine how long does it take to get out of your system?
More about Lamictal ODT (lamotrigine)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (4)
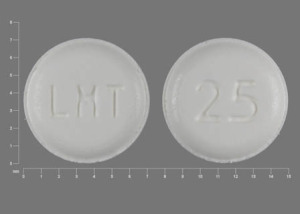
- Drug images
- Latest FDA alerts (6)
- Dosage information
- During pregnancy
- Generic availability
- Drug class: triazine anticonvulsants
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Other formulations
Related treatment guides
Further information
Lamictal ODT side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Some side effects may not be reported. You may report them to the FDA.