Xolegel Prescribing Information
Package insert / product label
Generic name: ketoconazole
Dosage form: topical gel
Drug class: Topical antifungals
Medically reviewed by Drugs.com. Last updated on Jul 30, 2024.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
XOLEGEL® (ketoconazole) gel for topical use
For Topical Use Only
Initial U.S. Approval: 1981
Indications and Usage for Xolegel
Xolegel Dosage and Administration
Dosage Forms and Strengths
- Gel containing 2% ketoconazole. (3)
Contraindications
- None.
Warnings and Precautions
XOLEGEL is flammable. Avoid using near fire, flame, or smoking during and immediately following application of XOLEGEL. (5.1)
Adverse Reactions/Side Effects
- The most common treatment-related adverse reaction was application site burning (4%). (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Almirall at 1-866-665-2782 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 12/2019
Related/similar drugs
prednisone, dexamethasone, hydrocortisone topical, nystatin topical, clotrimazole topical, terbinafine, terbinafine topical
Full Prescribing Information
1. Indications and Usage for Xolegel
XOLEGEL is indicated for the topical treatment of seborrheic dermatitis in immunocompetent adults and children 12 years of age and older.
Safety and efficacy of XOLEGEL for treatment of fungal infections have not been established.
2. Xolegel Dosage and Administration
XOLEGEL is for topical use only, and not for oral, ophthalmic, or intravaginal use.
XOLEGEL should be applied once daily to the affected area for 2 weeks.
3. Dosage Forms and Strengths
XOLEGEL is a translucent to clear amber colored gel containing 2% ketoconazole.
5. Warnings and Precautions
5.1 Flammable Contents
XOLEGEL is flammable. Avoid being near fire, flame, or smoking during and immediately following application of XOLEGEL.
5.2 Systemic Effects
Hepatitis and, at high doses, lowered testosterone and ACTH induced corticosteroid serum levels have been seen with orally administered ketoconazole; these effects have not been seen with topically administered ketoconazole.
5.3 Local Effects
XOLEGEL can cause local irritation at the application site. If irritation occurs or if the disease worsens, use of the medication should be discontinued and the health care provider should be contacted [see ADVERSE REACTIONS (6.1)].
6. Adverse Reactions/Side Effects
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
In the 3 safety and efficacy trials, 65 of 933 subjects (7%) experienced at least one treatment-related adverse event. The most common treatment-related adverse reaction was application site burning (4%). Treatment-related application site reactions that were reported in < 1% of subjects were: dermatitis, discharge, dryness, erythema, irritation, pain, pruritus, and pustules. Other treatment-related adverse reactions that were reported in < 1% of subjects were: eye irritation, eye swelling, keratoconjunctivitis sicca, impetigo, pyogenic granuloma, dizziness, headache, paresthesia, acne, nail discoloration, facial swelling.
7. Drug Interactions
Formal drug interaction studies with XOLEGEL have not been performed. Coadministration of oral ketoconazole with CYP3A4 metabolized HMG-CoA reductase inhibitors such as simvastatin, lovastatin and atorvastatin, may increase the risk of skeletal muscle toxicity, including rhabdomyolysis. These effects have not been observed with topically administered ketoconazole.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
There are no available data on XOLEGEL use in pregnant women to evaluate for a drug associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes.
In animal reproduction studies with pregnant rats, structural abnormalities (syndactylia and oligodactylia) were observed following oral doses of ketoconazole during organogenesis (see Data). The available data do not allow calculation of relevant comparisons between the systemic exposure of ketoconazole observed in animal studies to the systemic exposure observed in humans after topical use of XOLEGEL.
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2%-4% and 15%-20%, respectively.
Data
Animal Data
Oral administration of ketoconazole at 80 mg/kg/day to pregnant rats during organogenesis was associated with structural abnormalities (syndactylia and oligodactylia) . However, these effects may be related to maternal toxicity, which was also seen at this and higher dose levels.
In oral peri- and postnatal development studies in rats, maternal toxicity, prolonged gestation, embryolethality and fetotoxicity were observed at ketoconazole doses of 40 mg/kg/day and higher.
8.2 Lactation
Risk Summary
There are no data available on the presence of ketoconazole in human milk, its effects on the breastfed infant, or its effects on milk production. After topical application, ketoconazole concentrations in plasma are low and therefore concentrations in human breast milk are likely to be low [see Clinical Pharmacology (12.3)].
The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for XOLEGEL and any potential adverse effects on the breastfed infant from XOLEGEL or from the underlying maternal condition.
Clinical Considerations
Advise breastfeeding women not to apply XOLEGEL directly to the nipple and areola to avoid direct infant exposure.
8.4 Pediatric Use
Safety and effectiveness in pediatric subjects below the age of 12 have not been established.
8.5 Geriatric Use
Of the 933 subjects in the three safety and efficacy trials, 193 (20.7%) were 65 and older, while 61 (6.5%) were 75 and older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects but greater sensitivity of some older individuals cannot be ruled out.
11. Xolegel Description
XOLEGEL contains the antifungal agent ketoconazole USP at 2% in a topical anhydrous gel vehicle for topical administration.
Chemically, ketoconazole is (±)-cis-1-Acetyl-4-[p-[[2-(2,4-dichlorophenyl)-2-(1H-imidazol-1-ylmethyl)-1,3-dioxolan-4-yl]methoxy]phenyl]piperazine, with the molecular formula C26H28Cl2N4O4 and a molecular weight of 531.43.
Figure 1
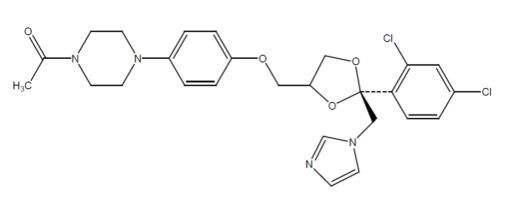
Each gram contains: 20 mg ketoconazole USP, dehydrated alcohol (34%), ascorbic acid, butylated hydroxytoluene, citric acid monohydrate, glycerin, hydroxypropyl cellulose, polyethylene glycol 400, PPG-15 stearyl ether, propylene glycol, FD&C yellow No. 6, and FD&C yellow No. 10.
XOLEGEL is a smooth, translucent to clear, amber gel.
12. Xolegel - Clinical Pharmacology
12.1 Mechanism of Action
The mechanism of action of ketoconazole in the treatment of seborrheic dermatitis is unknown.
12.3 Pharmacokinetics
In a pharmacokinetic absorption trial, eighteen subjects, both males and females, with severe seborrheic dermatitis (range 1-14% of body surface area) applied XOLEGEL once daily for 2 weeks. The median total amount of gel applied was 4.6 g (range 1.65–46.3 g). Daily doses ranged from 0.05 to 3.47 g. Mean (± standard deviation [SD]) peak plasma levels were 1.35 (± 3.18) ng/mL on Day 7 (range from <0.1 ng/mL, to 13.9 ng/mL), and 0.80 (± 1.22) ng/mL on Day 14 (range from <0.1 ng/mL to 5.4 ng/mL). Median Tmax was 8 hours on Day 7 and 7 hours on Day 14. Mean (± SD) AUC0-24 values were 20.8 (± 44.7) ng∙h/mL and 15.6 (± 26.4) ng∙h/mL on Day 7 and 14, respectively.
The plasma levels from an oral dose of 200 mg ketoconazole taken with a meal are approximately 250 times higher than the resulting plasma levels of ketoconazole following topical application of XOLEGEL.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
A 2-year dermal carcinogenicity study conducted in mice with topical administration of ketoconazole gel at doses up to 80 mg ketoconazole/kg/day exhibited no evidence of carcinogenic activity. A long-term feeding study in mice and in rats showed no evidence of carcinogenic activity.
Ketoconazole produced no evidence of mutagenicity in the dominant lethal mutation test in male and female mice at single oral doses up to 80 mg/kg. When tested in the Ames assay, ketoconazole was not mutagenic to Salmonella typhimurium in the presence or absence of metabolic activation. Ketoconazole, in combination with another drug, gave equivocal results in the mouse micronucleus test.
At oral doses of 75 mg/kg/day, ketoconazole impaired the reproductive performance in female (decreased pregnancy and implantation rates) and male (increased abnormal sperm and decreased sperm motility) rats.
14. Clinical Studies
Study 1 was a multicenter, double-blind, randomized, vehicle-controlled trial which enrolled 459 subjects 12 years of age and older with moderate to severe seborrheic dermatitis. A total of 229 subjects were treated with XOLEGEL, and 230 subjects were treated with vehicle. All subjects were treated once daily for 14 days, and efficacy was assessed at Day 28 (i.e., 2 weeks after end of treatment). Effective Treatment was defined as:
- an Investigator's Global Assessment score of ≤ 1 (completely clear or almost clear) and
- erythema and scaling scores of 0 (none) if the baseline score was 2, or 1 (mild) if the baseline score was 3.
The proportion of subjects effectively treated is shown in Table 1.
| XOLEGEL
N=229 | Vehicle
N=230 |
|
| Number and proportion of subjects effectively treated | 58 (25.3%) | 32 (13.9%) |
Two additional double-blind, randomized, vehicle-controlled, parallel, and multicenter trials that included a total of 316 subjects treated with XOLEGEL provided supportive evidence of the efficacy of XOLEGEL for treatment of seborrheic dermatitis. Subjects applied either XOLEGEL or vehicle study treatment to the affected area(s) once daily for 14 days and were followed through Day 28. Efficacy was assessed by the proportion of subjects who were completely clear at Day 28.
The contribution to efficacy of individual components of the vehicle has not been established.
16. How is Xolegel supplied
17. Patient Counseling Information
[See FDA-Approved Patient Labeling (Patient Information)]
- This medication is to be used as directed by the health care provider. It is for external use only.
- XOLEGEL may be irritating to mucus membranes. Contact with the eyes, nostrils, and mouth should be avoided.
- As with any topical medication, patients should wash their hands after application.
- Advise breastfeeding women not to apply XOLEGEL directly to the nipple and areola to avoid direct infant exposure.
- This medication should not be used for any disorder other than that for which it has been prescribed.
- Patients should report any signs of adverse reactions to their health care provider.
PATIENT INFORMATION
XOLEGEL® (Xol-a-gel)
(ketoconazole) Gel, 2%
Read the Patient Information that comes with XOLEGEL carefully before you start using it and each time you get a refill. There may be new information. This leaflet does not take the place of talking with your health care provider. If you have any questions about XOLEGEL, ask your health care provider.
What is XOLEGEL?
XOLEGEL is a prescription medicine used on the skin to treat a skin condition called seborrheic dermatitis.
Patients with seborrheic dermatitis can have areas of dry, flaky skin on the scalp, face, ears, chest, or upper back. XOLEGEL is only to be used in adults and in children older than 12 years of age who have a normal (healthy) immune system. XOLEGEL has not been studied in children below the age of 12.
It is not known whether XOLEGEL can be used to treat fungal infections.
XOLEGEL is a translucent to clear, amber colored gel.
What should I tell my health care provider before using XOLEGEL?
- Tell your health care provider about all of your medical conditions, including if you are pregnant or planning to become pregnant, or are breastfeeding or planning to breastfeed. XOLEGEL should be used during pregnancy and breastfeeding only if needed.
- Tell your health care provider about all of the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Keep a list of your medicines and show it to your health care provider and pharmacist. Tell your health care provider and pharmacist when you get a new medicine. It is not known if XOLEGEL and other medicines can interact with each other.
How should I use XOLEGEL?
- Use XOLEGEL exactly as prescribed. Talk to your health care provider if your condition gets worse or does not get better by the end of your treatment.
- Wash your hands before and after applying XOLEGEL.
- Spread a thin layer of XOLEGEL evenly on the affected skin with your fingertips. Be sure to cover all affected areas.
- Do not wash the areas where you applied XOLEGEL for at least 3 hours after you apply it.
- Wait at least 20 minutes after you spread XOLEGEL on your skin before you put makeup or sunscreens on the affected areas.
- Use XOLEGEL once daily for 2 weeks.
What should I avoid while using XOLEGEL?
- XOLEGEL is only to be used on the skin. It is not for eye, mouth, or vaginal use.
- Do not touch your eyes, nose, or mouth while you are applying XOLEGEL. Wash your hands well after you apply it. Irritation may occur if you get XOLEGEL in your eyes, nose, or mouth.
- If used during breastfeeding and XOLEGEL is applied on the chest, take care to avoid accidental ingestion of XOLEGEL by the baby.
- XOLEGEL is flammable (it can catch fire). Stay away from heat, flame, or smoking while you are applying XOLEGEL and right after you apply it.
- This medication should not be used for any disorder other than that for which it has been prescribed.
What are the possible side effects of XOLEGEL?
- The effects of XOLEGEL during pregnancy, including whether XOLEGEL can harm your unborn baby, are not known.
- It is not known if XOLEGEL can pass into your breastmilk or if it can harm your breastfed baby.
- Stop using XOLEGEL and talk to your health care provider if you develop itching, a rash, or any skin irritation after using XOLEGEL.
- Stop using XOLEGEL and talk to your health care provider if your skin condition (seborrheic dermatitis) gets worse.
- The most common side effect is a burning feeling where XOLEGEL is applied.
- Report any side effects to your health care provider to receive immediate medical attention. You can also report suspected side effects by calling the US Food and Drug Administration at 1-800-FDA-1088, or reporting via the internet at www.fda.gov/medwatch.
These are not all of the side effects of XOLEGEL. For more information, ask your health care provider or pharmacist.
How should I store XOLEGEL?
- Store XOLEGEL at 59°F to 86°F (15° to 30°C).
- Keep XOLEGEL and all medicines out of the reach of children.
- Contents are flammable. Avoid storing XOLEGEL near heat or flame.
General information about XOLEGEL
Medicines are sometimes prescribed for conditions that are not mentioned in Patient Information leaflets. Do not use XOLEGEL for a condition for which it was not prescribed. Do not give XOLEGEL to other people, even if they have the same symptoms that you have. It may harm them.
This Patient Information leaflet summarizes the most important information about XOLEGEL. If you would like more information, talk with your health care provider. You can also ask your pharmacist or health care provider for information about XOLEGEL that is written for health professionals.
What are the ingredients in XOLEGEL?
Active ingredient: ketoconazole, USP
Inactive ingredients: dehydrated alcohol, ascorbic acid, butylated hydroxytoluene, citric acid monohydrate, glycerin, hydroxypropyl cellulose, polyethylene glycol 400, PPG-15 stearyl ether, propylene glycol, FD&C yellow No. 6, and FD&C Yellow No. 10.
This Patient Information leaflet has been approved by the U.S. Food and Drug Administration.
The Patient Information leaflet was last revised: May 2012.
Manufactured for Almirall, LLC
101 Lindenwood Drive, Suite 400, Malvern, PA 19355
Revised 12/2019
XOLEGEL is a registered trademark of Almirall, LLC.
© 2019 Almirall, LLC
Almirall, LLC
| XOLEGEL
ketoconazole gel |
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
| Labeler - Almirall, LLC (605425912) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| DPT Laboratories, Ltd. | 832224526 | ANALYSIS(16110-080) , LABEL(16110-080) , MANUFACTURE(16110-080) | |
More about Xolegel (ketoconazole topical)
- Compare alternatives
- Reviews (8)
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: topical antifungals
- Breastfeeding
Patient resources
Professional resources
Other brands
Nizoral Shampoo, Extina, Ketodan