Veopoz Injection Prescribing Information
Package insert / product label
Generic name: pozelimab
Dosage form: injection, solution
Drug class: Selective immunosuppressants
J Code (medical billing code): J9376 (1 mg, injection)
Medically reviewed by Drugs.com. Last updated on Mar 25, 2024.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Storage and Handling
- Patient Counseling Information
- Medication Guide
Highlights of Prescribing Information
VEOPOZ® (pozelimab-bbfg) injection, for intravenous or subcutaneous use
Initial U.S. Approval: 2023
WARNING: SERIOUS MENINGOCOCCAL INFECTIONS
See full prescribing information for complete boxed warning
- Life-threatening and fatal meningococcal infections have occurred in patients treated with complement inhibitors. Meningococcal infection may become rapidly life-threatening or fatal if not recognized and treated early. (5.1)
- Complete or update meningococcal vaccination at least 2 weeks prior to administering the first dose of VEOPOZ, unless the risks of delaying therapy outweigh the risks of developing meningococcal infection. Follow the most current Advisory Committee on Immunization Practices (ACIP) recommendations for meningococcal vaccination in patients receiving a complement inhibitor. (5.1)
- Patients receiving VEOPOZ are at increased risk for invasive disease caused by N. meningitidis, even if they develop antibodies following vaccination. Monitor patients for early signs of meningococcal infections and evaluate immediately if infection is suspected. (5.1)
Indications and Usage for Veopoz Injection
VEOPOZ is a complement inhibitor indicated for the treatment of adult and pediatric patients 1 year of age and older with CD55-deficient protein-losing enteropathy (PLE), also known as CHAPLE disease. (1)
Veopoz Injection Dosage and Administration
See the full prescribing information for meningococcal vaccine and prophylaxis recommendations prior to the first dose of VEOPOZ. (2.1)
Recommended Dosage:
- Day 1 (loading dose): Administer a single 30 mg/kg dose by intravenous infusion after dilution. (2.2)
-
Day 8 and thereafter (maintenance dosage): Inject 10 mg/kg as a subcutaneous injection once weekly starting on Day 8.
- The maintenance dosage may be increased to 12 mg/kg once weekly if there is inadequate clinical response after at least 3 weekly doses (i.e., starting from Week 4).
- The maximum maintenance dosage is 800 mg once weekly. (2.2)
- See full prescribing information for instructions on preparation and administration. (2.2, 2.3, 2.4)
Dosage Forms and Strengths
Injection: 400 mg/2 mL (200 mg/mL) in a single-dose vial. (3)
Contraindications
VEOPOZ is contraindicated in patients with unresolved Neisseria meningitidis infection. (4)
Warnings and Precautions
- Other Bacterial Infections: Interrupt treatment with VEOPOZ in patients who are undergoing treatment for a serious encapsulated bacterial infection until the infection is resolved. (5.2)
- Systemic Hypersensitivity Reactions: Interrupt infusion and institute appropriate supportive measures if signs of cardiovascular instability or respiratory compromise occur. (5.3)
- Immune Complex Formation: Transition between other complement inhibitors has resulted in decreased drug concentrations and possible hypersensitivity reactions. Consider this potential if switching complement inhibitors to VEOPOZ. (5.4)
Adverse Reactions/Side Effects
Most common adverse reactions (in two or more patients) are: upper respiratory tract infection, fracture, urticaria, and alopecia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Regeneron at 1-855-583-6769 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Intravenous Immunoglobulin: May decrease pozelimab concentrations; avoid concomitant use. If concomitant use cannot be avoided, monitor patients for worsening of clinical signs and symptoms of disease. (7.1)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 3/2024
Related/similar drugs
pozelimab
Full Prescribing Information
WARNING: SERIOUS MENINGOCOCCAL INFECTIONS
- Life-threatening and fatal meningococcal infections have occurred in patients treated with complement inhibitors. Meningococcal infection may become rapidly life-threatening or fatal if not recognized and treated early.
- Complete or update meningococcal vaccination (for serogroups A, C, W and Y, and serogroup B) at least 2 weeks prior to administering the first dose of VEOPOZ, unless the risks of delaying therapy outweigh the risk of developing a meningococcal infection. Follow the most current Advisory Committee on Immunization Practices (ACIP) recommendations for meningococcal vaccination in patients receiving a complement inhibitor.
- Patients receiving VEOPOZ are at increased risk for invasive disease caused by N. meningitidis, even if they develop antibodies following vaccination. Monitor patients for early signs of meningococcal infections and evaluate immediately if infection is suspected [see Warnings and Precautions (5.1)].
1. Indications and Usage for Veopoz Injection
VEOPOZ is indicated for the treatment of adult and pediatric patients 1 year of age and older with CD55-deficient protein-losing enteropathy (PLE), also known as CHAPLE disease.
2. Veopoz Injection Dosage and Administration
2.1 Recommended Vaccination and Prophylaxis for Meningococcal Infection Prior to First Dose of VEOPOZ
- Vaccinate patients for meningococcal infection (serogroups A, C, W, and Y [MenACWY] and serogroup B [MenB]) according to current ACIP recommendations for patients receiving a complement inhibitor at least 2 weeks prior to administering the first dose of VEOPOZ [see Warnings and Precautions (5.1)].
- If urgent VEOPOZ therapy is indicated in a patient who is not up-to-date with vaccines for both MenACWY and MenB according to ACIP recommendations, administer meningococcal vaccine(s) as soon as possible and provide the patient with antibacterial drug prophylaxis. The efficacy, duration, and drug regimens for antibacterial drug prophylaxis have not been studied in patients receiving complement inhibitors, including VEOPOZ.
2.2 Recommended Dosage and Administration
The recommended dosage of VEOPOZ is as follows:
Day 1 (Loading Dose):
Administer a single 30 mg/kg dose by intravenous infusion after dilution [see Dosage and Administration (2.3)].
Day 8 and Thereafter (Maintenance Dosage):
Inject 10 mg/kg as a subcutaneous injection once weekly starting on Day 8 [see Dosage and Administration (2.4)].
- The maintenance dosage may be increased to 12 mg/kg once weekly if there is inadequate clinical response after at least 3 weekly doses (i.e., starting from Week 4).
- The maximum maintenance dosage is 800 mg once weekly.
- Doses greater than 400 mg require 2 injections.
2.3 Intravenous Infusion Loading Dose: Preparation and Administration Instructions
VEOPOZ for intravenous use must be prepared and administered by a healthcare provider.
Preparation Instructions for Intravenous Infusion Loading Dose
- Remove VEOPOZ vial(s) from refrigeration and allow the vial(s) to sit for at least 45 minutes at room temperature 20ºC to 25ºC (68ºF to 77ºF) before use.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. VEOPOZ should be a clear to slightly opalescent, colorless to pale yellow solution that is free from visible particulates. Discard the vial(s) if the solution is cloudy, discolored or contains particulate matter.
- Gently swirl the vial(s) in an upright position. Do not shake the vial(s) as this may result in foaming.
- Use a 21G stainless steel needle with Luer-Lok to withdraw the calculated volume of VEOPOZ from the vial(s). Discard any unused VEOPOZ remaining in the vial(s).
- Dilute VEOPOZ in an intravenous infusion bag of 25 mL to 250 mL of either 0.9% Sodium Chloride Injection or 5% Dextrose Injection to a final concentration of 6.7 mg/mL to 20 mg/mL.
- Mix the diluted solution by gentle inversion. Do not shake.
Administration Instructions for Intravenous Infusion Loading Dose
- Infuse through an intravenous line containing a sterile, in-line or add-on 0.2-micron to 5-micron filter.
- Infusion rate: infuse over a minimum of 1 hour; do not exceed maximum rate of 1000 mg/hour
- Do not co-administer other medications through the same intravenous line
- Observe the patient for 30 minutes following completion of the infusion [see Warnings and Precautions (5.3)].
Storage of Diluted Intravenous Solution
- Administer the diluted VEOPOZ solution immediately after preparation. If not used immediately, store at room temperature up to 25°C (77°F) for no more than 8 hours from the time of preparation to the end of the infusion or refrigerate at 2°C to 8°C (36°F to 46°F) for no more than 24 hours from the time of preparation to the end of infusion.
- If stored in the refrigerator, allow the diluted solution to come to room temperature prior to administration.
- Discard the unused VEOPOZ diluted solution after 8 hours if stored at room temperature or after 24 hours if refrigerated.
- Do not freeze the diluted solution.
2.4 Subcutaneous Maintenance Dose: Preparation and Administration Instructions
VEOPOZ for subcutaneous use must be prepared and administered by a healthcare provider.
Preparation Instructions for Subcutaneous Maintenance Dose
- Remove VEOPOZ vial(s) from refrigeration and allow the vial(s) to sit for at least 45 minutes at room temperature 20ºC to 25ºC (68ºF to 77ºF) before use.
- Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit. VEOPOZ should be a clear to slightly opalescent, colorless to pale yellow solution that is free from visible particulates. Discard the vial(s) if the solution is cloudy, discolored or contains particulate matter.
- Gently swirl the vial(s) in an upright position. Do not shake the vial(s) as this may result in foaming.
- Use a withdrawal needle (21G needle with Luer-Lok) to withdraw the calculated dose volume of VEOPOZ from the appropriate number of vial(s). Discard any unused VEOPOZ remaining in the vial(s).
- For patients receiving a dose greater than 400 mg, preparation of 2 separate injections will be required for subcutaneous administration of the total dose volume.
- Change the needle on the syringe to an injection needle fulfilling the following criteria: 25G to 27G and 1/2 or 5/8-inch stainless steel needle with Luer-Lok.
Administration Instructions for Subcutaneous Maintenance Dose
- Inject VEOPOZ into the abdomen, thigh, or upper arm. Rotate sites. Do not inject VEOPOZ into moles, scars, or areas where the skin is tender, bruised, red, hard, or not intact. When administering more than one injection, administer consecutively, each at different injection sites.
- Observe the patient for 30 minutes following completion of the first subcutaneous injection [see Warnings and Precautions (5.3)].
2.5 Recommendations Regarding Missed Maintenance Subcutaneous Dose(s)
If a subcutaneous maintenance dose of VEOPOZ is missed, administer as soon as possible within 3 days after the missed dose. Do not administer 2 doses on the same day to make up for a missed dose. If more than 3 days have passed, skip the missed dose and administer the next dose on the regularly scheduled day. In each case, patients can then resume their regular once weekly dosing schedule.
The day of weekly administration can be changed, if necessary, as long as the time between the two doses is at least 4 days (96 hours).
3. Dosage Forms and Strengths
Injection: 400 mg/2 mL (200 mg/mL) as a clear to slightly opalescent, colorless to pale yellow solution in a single-dose vial.
4. Contraindications
VEOPOZ is contraindicated in:
- Patients with unresolved Neisseria meningitidis infection [see Warnings and Precautions (5.1)].
5. Warnings and Precautions
5.1 Serious Meningococcal Infections
Life-threatening and fatal meningococcal infections have occurred in both vaccinated and unvaccinated patients treated with complement inhibitors. The use of VEOPOZ increases a patient's susceptibility to serious and life-threatening meningococcal infections (septicemia and/or meningitis) caused by any serogroup, including nongroupable strains.
Complete or update meningococcal vaccination (for serogroups A, C, W, and Y [MenACWY] and serogroup B [MenB]) at least 2 weeks prior to administering the first dose of VEOPOZ, according to the most current Advisory Committee on Immunization Practices (ACIP) recommendations for patients receiving a complement inhibitor. Revaccinate patients in accordance with ACIP recommendations considering the duration of VEOPOZ therapy.
If urgent VEOPOZ therapy is indicated in a patient who is not up-to-date with both MenACWY and MenB vaccines according to ACIP recommendations, administer meningococcal vaccine(s) as soon as possible and provide the patient with antibacterial drug prophylaxis. The efficacy, duration, and drug regimens for antibacterial drug prophylaxis have not been studied in patients receiving complement inhibitors.
Because of inhibition of complement activity by VEOPOZ, as well as risk of infection caused by nongroupable strains of N. meningitidis, vaccination does not eliminate the risk of meningococcal infections, despite development of antibodies following vaccination.
Closely monitor patients for early signs and symptoms of meningococcal infection and evaluate patients immediately if infection is suspected. Inform patients and caregivers of these signs and symptoms and instruct patients to seek immediate medical care if these signs and symptoms occur. Meningococcal infection may become rapidly life-threatening or fatal if not recognized and treated early. Interrupt treatment with VEOPOZ in patients who are undergoing treatment for serious meningococcal infection until the infection is resolved [see Contraindications (4)].
5.2 Other Bacterial Infections
VEOPOZ blocks terminal complement activation; therefore, patients may have increased susceptibility to encapsulated bacterial infections, especially infections caused by Neisseria meningitidis but also Streptococcus pneumoniae, Haemophilus influenzae, and to a lesser extent, Neisseria gonorrhoeae. Patients treated with VEOPOZ may be at increased risk of developing serious infections due to Streptococcus pneumoniae and Haemophilus influenzae type b (Hib). Administer vaccinations for the prevention of Streptococcus pneumoniae and Haemophilus influenzae type b (Hib) infections according to ACIP guidelines. Patients receiving VEOPOZ are at increased risk for infections due to these organisms, even if they develop antibodies following vaccination. Interrupt treatment with VEOPOZ in patients who are undergoing treatment for a serious encapsulated bacterial infection until the infection is resolved. Counsel patients about gonorrhea prevention and advise regular testing for patients at risk.
5.3 Systemic Hypersensitivity Reactions
Hypersensitivity reactions, including anaphylaxis, have been reported with administration of complement inhibitors. Interrupt VEOPOZ and institute appropriate supportive measures if signs of cardiovascular instability or respiratory compromise occur.
5.4 Immune Complex Formation
Immune complex formation has been reported during the transition of therapy between complement inhibitors, resulting in transient decrease in drug concentrations as well as symptoms suggestive of hypersensitivity reactions. However, this has not been studied in patients with CD55-deficient PLE switching from other complement inhibitors to pozelimab. The potential for immune complex formation should be considered if switching complement inhibitors.
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Serious Meningococcal Infections [see Warnings and Precautions (5.1)]
- Other Bacterial Infections [see Warnings and Precautions (5.2)]
- Systemic Hypersensitivity Reactions [see Warnings and Precautions (5.3)]
- Immune Complex Formation [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of VEOPOZ was evaluated in 10 patients with CD55-deficient PLE (ranging from 3 to 19 years of age) in a single-arm study [see Clinical Studies (14)]. The median duration of exposure was 104 weeks (range: 75 to 140 weeks). Adverse reactions reported in two or more patients are summarized in Table 1.
| Adverse Reactions | VEOPOZ N=10 n (%) |
|---|---|
|
|
| Upper respiratory tract infection* | 3 (30) |
| Fracture | 3 (30) |
| Urticaria | 2 (20) |
| Alopecia* | 2 (20) |
Additionally, injection site reactions (including dermatitis and erythema), metabolic acidosis, gingival bleeding, increased blood uric acid, increased liver enzymes, hematuria and proteinuria were reported in one patient each.
7. Drug Interactions
7.1 Intravenous Immunoglobulin
VEOPOZ has not been studied in combination with intravenous immunoglobulin. Intravenous immunoglobulin may interfere with the endosomal neonatal Fc receptor (FcRn) recycling mechanism of monoclonal antibodies such as pozelimab thereby decreasing serum pozelimab concentrations. Avoid concomitant use of intravenous immunoglobulin with VEOPOZ. If concomitant use cannot be avoided, monitor patients for worsening of clinical signs and symptoms of CD55-deficient PLE [see Clinical Pharmacology (12.3)].
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Although there are no data on VEOPOZ use in pregnant women to inform a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes, monoclonal antibodies can be actively transported across the placenta.
In an animal reproduction study in monkeys, pozelimab-bbfg did not adversely affect embryofetal or postnatal development when administered from pregnancy confirmation through parturition at doses that produced exposure up to 3.3 to 3.8 times the predicted clinical exposures (on an AUC basis; see Data).
The estimated background risk of major birth defects and miscarriage for the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other outcome. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
In an enhanced pre- and postnatal development study, pregnant female monkeys were subcutaneously administered pozelimab-bbfg at doses of 5 or 50 mg/kg once weekly from confirmation of pregnancy (gestation day 20) through parturition (approximately gestation day 160). No adverse effects were observed on maintenance of pregnancy, pregnancy outcome, or on the development of offspring through postnatal day 90 at doses up to 3.3-3.8 times the predicted clinical exposures.
8.2 Lactation
Risk Summary
There are no data on the presence of pozelimab-bbfg in either human or animal milk, the effects on the breastfed infant, or the effects on milk production. Endogenous maternal IgG and monoclonal antibodies are transferred into human milk. The effects of local gastrointestinal exposure and the extent of systemic exposure in the breastfed infant to pozelimab are unknown. The development and health benefits of breastfeeding should be considered along with the mother's clinical need for VEOPOZ and any potential adverse effects on the breastfed infant from VEOPOZ or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of VEOPOZ for the treatment of CD55-deficient PLE have been established in pediatric patients 1 year of age and older. Use of VEOPOZ for this indication is supported by a single-arm study in 10 patients with active CD55-deficient PLE [see Adverse Reactions (6.1) and Clinical Studies (14)].
The safety and effectiveness of VEOPOZ have not been established in pediatric patients less than 1 year of age.
11. Veopoz Injection Description
Pozelimab-bbfg, a complement inhibitor, is a recombinant monoclonal antibody (IgG4 isotype). Pozelimab-bbfg is produced by recombinant DNA technology in Chinese Hamster Ovary (CHO) cell suspension culture and has an approximate molecular weight of 145 kDa.
VEOPOZ (pozelimab-bbfg) injection is a sterile, preservative-free, clear to slightly opalescent, colorless to pale yellow solution supplied in a single-dose glass vial, free from visible particulates, for intravenous or subcutaneous use. Each vial contains 400 mg pozelimab-bbfg in 2 mL of solution with a pH of 5.8. Each mL contains 200 mg pozelimab-bbfg, arginine hydrochloride (21 mg), histidine (1.15 mg), L-histidine hydrochloride monohydrate (2.65 mg), polysorbate 80 (1.5 mg), sucrose (20 mg), and Water for Injection, USP.
12. Veopoz Injection - Clinical Pharmacology
12.1 Mechanism of Action
Pozelimab-bbfg is a human, monoclonal immunoglobulin G4P (IgG4P) antibody directed against the terminal complement protein C5 that inhibits terminal complement activation by blocking cleavage of C5 into C5a (anaphylatoxin) and C5b, thereby blocking the formation of the membrane-attack complex (C5b-C9, a structure mediating cell lysis).
12.2 Pharmacodynamics
The effect of pozelimab-bbfg on complement activity was measured by total complement hemolytic activity test (CH50). The magnitude and duration of reduction from baseline in CH50 by pozelimab-bbfg was dose dependent.
In healthy subjects receiving a single dose of VEOPOZ 30 mg/kg administered as an intravenous infusion over approximately one hour, the complete inhibition of CH50 was achieved at the end of infusion in all subjects, was maintained for 28 days, and returned to baseline 84 days post-dose. After a single dose of VEOPOZ administered as a 600 mg subcutaneous injection, the maximum reduction from baseline in CH50 was achieved 7 days post-dose in most subjects (range: 3 to 14 days), corresponding to Tmax, and returned to baseline 56 days post-dose.
In patients with CD55-deficient PLE receiving a single 30 mg/kg dose administered as an intravenous infusion over approximately one hour followed by a weight-tiered subcutaneous injection once weekly starting at Week 1, CH50 was completely inhibited by Week 1 for most subjects and by Week 12 for all patients.
In the same study of patients with CD55-deficient PLE, serum albumin concentrations increased as early as Week 1 and reached the normal range (≥3.5 g/dL) by Week 4 for most subjects and by Week 12 for all subjects. The serum albumin concentrations were maintained within the normal range for the duration of treatment. Endogenous serum IgG concentrations were also increased from baseline at Week 1 in all patients with CD55-deficient PLE and reached a stable concentration around Week 16 [see Clinical Studies (14)].
12.3 Pharmacokinetics
In healthy subjects, single intravenous infusions of VEOPOZ over approximately one hour resulted in dose proportional increases in mean Cmax, but greater than proportional increases in mean AUCinf (>16-fold) for total pozelimab concentrations in serum between 3 mg/kg and 30 mg/kg. The mean AUCinf increased by 3.5-fold between 10 mg/kg and 30 mg/kg. In healthy subjects, single subcutaneous injections of VEOPOZ resulted in approximately 1.5-fold increase in mean Cmax and 2.2-fold increase in mean AUCinf between 300 mg and 600 mg.
In patients with CD55-deficient PLE, a single dose of VEOPOZ 30 mg/kg administered as an intravenous infusion over approximately one hour resulted in median (range) total pozelimab trough concentration of 180 (52.8, 268) mg/L at Week 1. The predicted mean (SD) trough concentrations of total pozelimab at steady state are 330 (94.2) mg/L and 385 (112) mg/L for VEOPOZ 10 mg/kg or 12 mg/kg (up to a maximum 800 mg) once weekly via subcutaneous injection(s), respectively, following the intravenous loading dose.
Absorption
In healthy subjects, following subcutaneous injection of 600 mg, the bioavailability of pozelimab-bbfg is estimated as 51%. The median (range) time to reach peak concentration was 7 (3 to 7) days following a single subcutaneous injection of 300 mg or 600 mg in healthy subjects.
Distribution
In healthy adult subjects with a mean body weight of 70 kg, the mean (SD) volume of distribution following a single intravenous dose of 30 mg/kg was 3.3 (0.4) L. The mean (SD) apparent volume of distribution following a single subcutaneous injection of 300 mg and 600 mg was 6.0 (0.9) L and 8.6 (2.7) L, respectively.
Elimination
Pozelimab-bbfg is expected to be degraded into small peptides and amino acids via catabolic pathways in the same manner as endogenous IgG. Pozelimab-bbfg elimination is mediated via linear and non-linear pathways. At higher concentrations, pozelimab-bbfg elimination is primarily through the linear non-saturable proteolytic pathway, whereas at lower concentrations, the non-linear, saturable C5 target-mediated elimination predominates.
In healthy adult subjects, the median (range) terminal half-life of total pozelimab in serum was 13.5 (10.0, 17.2) days following a single 30 mg/kg dose administered as an intravenous infusion. The median (range) terminal half-life was 14.1 (8.6, 17.3) days following a single 600 mg subcutaneous injection.
In patients with CD55-deficient PLE, steady-state total pozelimab concentrations were reached at approximately 20 weeks following subcutaneous injection once weekly.
Drug Interaction Studies
Drug interaction studies have not been conducted. Intravenous Immunoglobulin (IVIg) may interfere with the endosomal neonatal Fc receptor (FcRn) recycling mechanism of monoclonal antibodies such as pozelimab-bbfg, which may decrease serum pozelimab concentrations [see Drug Interactions (7.1)].
12.6 Immunogenicity
The observed incidence of anti-drug antibodies is highly dependent on the sensitivity and specificity of the assay. Differences in assay methods preclude meaningful comparisons of the incidence of anti-drug antibodies in the study described below with the incidence of anti-drug antibodies in other studies, including those of VEOPOZ or of other pozelimab products.
Nine of the 10 patients 3 years of age and older with CD55-deficient PLE in the clinical study were evaluable for anti-pozelimab antibodies. None of these patients developed anti-pozelimab-bbfg antibodies during the 48-week treatment with pozelimab-bbfg. There is insufficient information to characterize the effect of anti-drug antibodies on the pharmacokinetics, pharmacodynamics, safety, and/or effectiveness of pozelimab.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis and Mutagenesis
Carcinogenicity studies have not been conducted with pozelimab-bbfg. The mutagenic potential of pozelimab-bbfg has not been evaluated; however, monoclonal antibodies are not expected to alter DNA or chromosomes.
Impairment of Fertility
Fertility studies have not been conducted with pozelimab-bbfg. In a 6-month toxicity study in sexually-mature male and female monkeys, pozelimab-bbfg had no adverse effects on histological or functional markers of reproductive function (e.g., estrous cyclicity, testicular volume, ejaculate amount, total sperm count per ejaculate, sperm motility and morphology, and histology of reproductive organs) at doses up to 100 mg/kg/week (11.9 to 13.9-fold the predicted exposures at the recommended clinical doses, on an AUC basis).
14. Clinical Studies
The efficacy and safety of VEOPOZ were evaluated in a single-arm study (NCT04209634) where outcomes were compared to pre-treatment data in patients with active CD55-deficient protein-losing enteropathy (PLE) who had hypoalbuminemia. Diagnosis was based on a clinical history of PLE and with a confirmed genotype of biallelic CD55 loss-of-function mutation.
Active CD55-deficient PLE was defined as hypoalbuminemia (serum albumin concentration of ≤3.2 g/dL) with one or more of the following signs or symptoms within the last six months: abdominal pain, diarrhea, peripheral edema, or facial edema.
Patients received a single 30 mg/kg loading dose of VEOPOZ administered by intravenous infusion over approximately one hour, followed by a once weekly weight-tiered maintenance dosage, administered as a subcutaneous injection starting one week after the loading dose.
All patients received meningococcal vaccination prior to treatment with VEOPOZ and antibacterials for prophylaxis of meningococcal infection. Patients were permitted to receive additional therapies as part of standard of care. Use of other complement inhibitors was prohibited.
Ten patients ranging from 3 to 19 years of age (median of 8.5 years) were assessed for efficacy. Six patients identified as female; seven patients as White, two patients as Asian, and one patient reported race as other. The mean baseline serum albumin concentration was 2.2 g/dL with a range of 1.1 to 2.9 g/dL.
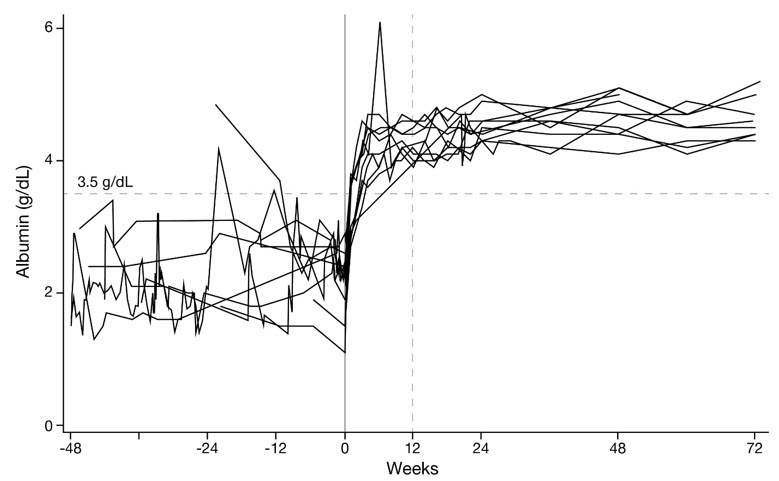
Serum Albumin Concentrations
The median time for serum albumin to reach at least 3.5 g/dL was 15.5 days (N=10; 95% CI: 8 to 28). All 10 patients achieved normalization by Week 12 and maintained serum albumin concentrations within the normal range through at least 72 weeks of treatment (Figure 1).
Figure 1: Serum Albumin Concentrations from 48 Weeks Pre-Treatment Through 72 Weeks on VEOPOZ in Ten Patients with CD55-Deficient PLE
Albumin Transfusions
Five of the 10 patients received a total of 60 transfusions in the 48 weeks prior to treatment. In the 48 weeks after starting treatment, one patient received one albumin transfusion.
16. How is Veopoz Injection supplied
VEOPOZ (pozelimab-bbfg) injection is a clear to slightly opalescent, colorless to pale yellow solution. It is supplied in a carton containing one single-dose glass vial of:
- 400 mg/2 mL (200 mg/mL) (NDC 61755-014-01).
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Inform patients that they will be given a Patient Safety Card for VEOPOZ that they should carry with them at all times. This card describes symptoms of meningococcal, or other infection, which, if experienced, should prompt the patient to seek immediate medical evaluation.
Meningococcal Infection
- Advise patients of the risk of meningococcal, and other bacterial infections.
- Inform patients of the need to complete or update meningococcal vaccination for both MenACWY and MenB at least 2 weeks prior to receiving the first dose of VEOPOZ and to be revaccinated according to current ACIP recommendations for meningococcal vaccines while on VEOPOZ therapy.
- Inform patients that vaccination may not prevent meningococcal infection.
- Inform patients of the signs and symptoms of meningococcal infection and advise patients to seek immediate medical attention if any signs or symptoms of infection occur [see Warnings and Precautions (5.1)].
Other Bacterial Infections, Including Gonococcal Infection
- Inform patients of the increased risk of other bacterial infections, particularly those due to encapsulated bacteria.
- Inform patients of the need to receive vaccinations according to the ACIP recommendations.
- Advise patients to report any new signs and symptoms of infection.
- Counsel patients about gonorrhea prevention and advise patients at risk (e.g., sexually active) to seek regular testing [see Warnings and Precautions (5.2)].
Systemic Hypersensitivity Reactions
Advise patients to notify the healthcare provider and seek immediate medical attention if they experience any symptoms of systemic hypersensitivity reactions [see Warnings and Precautions (5.3)].
Manufactured by:
Regeneron Pharmaceuticals, Inc.
777 Old Saw Mill River Road
Tarrytown, NY 10591-6707
U.S. License No. 1760
Marketed by:
Regeneron Pharmaceuticals, Inc. (Tarrytown, NY 10591)
©2024 Regeneron Pharmaceuticals, Inc.
All rights reserved.
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: March 2024 | |||
| MEDICATION GUIDE VEOPOZ® (VEE-oh-poz) (pozelimab-bbfg) injection, for intravenous or subcutaneous use |
||||
| What is the most important information I should know about VEOPOZ? VEOPOZ is a medicine that affects your immune system. VEOPOZ can lower the ability of your immune system to fight infections.
|
||||
|
||||
|
|
|||
| Your healthcare provider will give you a Patient Safety Card about the symptoms of meningococcal, or other infection. Carry it with you at all times during treatment and for 3 months after your last VEOPOZ dose. Your risk of meningococcal infection may continue for several weeks after your last dose of VEOPOZ. It is important to show this card to any healthcare provider who treats you. This will help them diagnose and treat you quickly. VEOPOZ may also increase the risk of other types of serious bacterial infections.
|
||||
| What is VEOPOZ?
VEOPOZ is a prescription medicine called a monoclonal antibody. VEOPOZ is used to treat adults and children 1 year of age and older with a disease called CD55-deficient protein-losing enteropathy (PLE), also known as CHAPLE disease. It is not known if VEOPOZ is safe and effective in children younger than 1 year of age. |
||||
Do not receive VEOPOZ if you:
|
||||
Before you receive VEOPOZ, tell your healthcare provider about all of your medical conditions, including if you:
It is important that you:
Especially tell your healthcare provider if you take Intravenous Immunoglobulin (IVIg). Know the medicines you take and the vaccines you receive. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine. |
||||
How should I receive VEOPOZ?
|
||||
| What are the possible side effects of VEOPOZ? VEOPOZ can cause serious side effects including:
|
||||
|
|
|||
| The most common side effects of VEOPOZ are: | ||||
|
|
|
||
| Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all of the possible side effects of VEOPOZ. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | ||||
| General information about the safe and effective use of VEOPOZ.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. You can ask your pharmacist or healthcare provider for information about VEOPOZ that is written for health professionals. |
||||
| What are the ingredients in VEOPOZ?
Active ingredient: pozelimab-bbfg. Inactive ingredients: arginine hydrochloride, histidine, L-histidine hydrochloride monohydrate, polysorbate 80, sucrose, and Water for Injection. Manufactured by: Regeneron Pharmaceuticals, Inc., Tarrytown, NY 10591 U.S. License No. 1760 © 2024 Regeneron Pharmaceuticals, Inc. All rights reserved. For more information about VEOPOZ, go to www.VEOPOZ.com or call 1-855-5VEOPOZ (1-855-583-6769). |
||||
PRINCIPAL DISPLAY PANEL - 2 mL Vial Carton
NDC 61755-014-01
Rx only
Veopoz®
(pozelimab-bbfg)
Injection
400 mg/2 mL (200 mg/mL)
For Intravenous Infusion after Dilution or
Subcutaneous Use
Dispense the enclosed Medication Guide to each patient.
Must dilute before intravenous infusion.
Single-Dose Vial. Discard Unused Portion.
One 2 mL Vial
REGENERON
| VEOPOZ
pozelimab injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Regeneron Pharmaceuticals, Inc. (194873139) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Regeneron Pharmaceuticals, Inc. | 945589711 | API MANUFACTURE(61755-014) , ANALYSIS(61755-014) | |
More about Veopoz (pozelimab)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: selective immunosuppressants
- En español

