Kalydeco: Package Insert / Prescribing Info
Package insert / product label
Generic name: ivacaftor
Dosage forms: tablet, film coated, oral granule
Drug class: CFTR potentiators
Medically reviewed by Drugs.com. Last updated on Jun 30, 2024.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Overdosage
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
KALYDECO® (ivacaftor) tablets, for oral use
KALYDECO® (ivacaftor) oral granules
Initial U.S. Approval: 2012
Recent Major Changes
Indications and Usage for Kalydeco
KALYDECO is a cystic fibrosis transmembrane conductance regulator (CFTR) potentiator indicated for the treatment of cystic fibrosis (CF) in patients age 1 month and older who have at least one mutation in the CFTR gene that is responsive to ivacaftor based on clinical and/or in vitro assay data. (12.1, 14)
If the patient's genotype is unknown, an FDA-cleared CF mutation test should be used to detect the presence of a CFTR mutation followed by verification with bi-directional sequencing when recommended by the mutation test instructions for use. (1)
Kalydeco Dosage and Administration
| Age | Weight | Dosage | Administration |
|---|---|---|---|
| 1 month to less than 2 months | 3 kg or greater | One 5.8 mg packet every 12 hours | Mixed with one teaspoon (5 ml) of soft food or liquid and administered orally with fat-containing food |
| 2 months to less than 4 months | 3 kg or greater | One 13.4 mg packet every 12 hours | |
| 4 months to less than 6 months | 5 kg or greater | One 25 mg packet every 12 hours | |
| 6 months to less than 6 years | 5 kg to less than 7 kg | One 25 mg packet every 12 hours | |
| 7 kg to less than 14 kg | One 50 mg packet every 12 hours | ||
| 14 kg or greater | One 75 mg packet every 12 hours | ||
| 6 years and older | - | One 150 mg tablet every 12 hours | Taken orally with fat-containing food |
- See full prescribing information for the recommended dosage in patients 6 months and older with moderate or severe hepatic impairment. (2.3, 8.6)
- See full prescribing information for dosage modifications due to drug interactions with KALYDECO. (2.4, 7.1)
- Not recommended in pediatric patients less than 1 month of age. (2.2, 8.4)
- Not recommended in patients 1 month to less than 6 months of age with any level of hepatic impairment and/or taking concomitant moderate or strong CYP3A inhibitors. (2.3, 2.4, 8.6)
Dosage Forms and Strengths
Contraindications
- None (4)
Warnings and Precautions
- Elevated transaminases (ALT or AST): Transaminases (ALT and AST) should be assessed prior to initiating KALYDECO, every 3 months during the first year of treatment, and annually thereafter. In patients with a history of transaminase elevations, more frequent monitoring of liver function tests should be considered. Patients who develop increased transaminase levels should be closely monitored until the abnormalities resolve. Interrupt dosing in patients with ALT or AST of greater than 5 times the upper limit of normal (ULN). Following resolution of transaminase elevations, consider the benefits and risks of resuming KALYDECO dosing. (5.1, 6)
- Hypersensitivity reactions: Anaphylaxis has been reported with KALYDECO in the postmarketing setting. Initiate appropriate therapy in the event of a hypersensitivity reaction. (5.2)
- Use with CYP3A inducers: Concomitant use with strong CYP3A inducers (e.g., rifampin, St. John's wort) substantially decreases exposure of ivacaftor, which may diminish effectiveness. Therefore, co-administration is not recommended. (5.3, 7.2, 12.3)
- Cataracts: Non-congenital lens opacities/cataracts have been reported in pediatric patients treated with KALYDECO. Baseline and follow-up examinations are recommended in pediatric patients initiating KALYDECO treatment. (5.4)
Adverse Reactions/Side Effects
The most common adverse drug reactions to KALYDECO (≥8% of patients with CF who have a G551D mutation in the CFTR gene) were headache, oropharyngeal pain, upper respiratory tract infection, nasal congestion, abdominal pain, nasopharyngitis, diarrhea, rash, nausea, and dizziness. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Vertex Pharmaceuticals Incorporated at 1-877-634-8789 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
CYP3A inhibitors: Reduce KALYDECO dose in patients aged 6 months and older when co-administered with strong CYP3A inhibitors (e.g., ketoconazole) or moderate CYP3A inhibitors (e.g., fluconazole). KALYDECO is not recommended in patients aged 1 month to less than 6 months when co-administered with strong or moderate CYP3A inhibitors. Avoid food or drink containing grapefruit. (2.4, 7.1)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 8/2023
Full Prescribing Information
1. Indications and Usage for Kalydeco
KALYDECO is indicated for the treatment of cystic fibrosis (CF) in patients age 1 month and older who have at least one mutation in the CFTR gene that is responsive to ivacaftor potentiation based on clinical and/or in vitro assay data [see Clinical Pharmacology (12.1) and Clinical Studies (14)].
If the patient's genotype is unknown, an FDA-cleared CF mutation test should be used to detect the presence of a CFTR mutation followed by verification with bi-directional sequencing when recommended by the mutation test instructions for use.
2. Kalydeco Dosage and Administration
2.1 Recommended Dosage in Adults and Pediatric Patients Aged 6 Years and Older
The recommended dosage of KALYDECO for adults and pediatric patients aged 6 years and older is 150 mg orally every 12 hours (300 mg total daily dose) with fat-containing food [see Dosage and Administration (2.5)].
2.2 Recommended Dosage in Pediatric Patients Aged 1 Month to Less than 6 Years
The recommended dosage of KALYDECO (oral granules) for pediatric patients ages 1 month to less than 6 years is weight-based provided in Table 1. Take KALYDECO orally with fat-containing food [see Dosage and Administration (2.5)].
| Age | Body Weight (kg) | KALYDECO Dosage |
|---|---|---|
| 1 month to less than 2 months*† | 3 kg or greater | One packet (containing 5.8 mg ivacaftor) every 12 hours |
| 2 months to less than 4 months*† | 3 kg or greater | One packet (containing 13.4 mg ivacaftor) every 12 hours |
| 4 months to less than 6 months† | 5 kg or greater | One packet (containing 25 mg ivacaftor) every 12 hours |
| 6 months to less than 6 years of age | 5 kg to less than 7 kg | One packet (containing 25 mg ivacaftor) every 12 hours |
| 7 kg to less than 14 kg | One packet (containing 50 mg ivacaftor) every 12 hours | |
| 14 kg or greater | One packet (containing 75 mg ivacaftor) every 12 hours | |
2.3 Recommended Dosage for Patients with Hepatic Impairment
KALYDECO is not recommended in patients less than 6 months of age with any level of hepatic impairment. The following is the recommended dosage of KALYDECO taken with fat-containing food [see Dosage and Administration (2.5)] for patients aged 6 months and older with hepatic impairment:
-
Mild Hepatic Impairment (Child-Pugh Class A):
- Less than 6 months of age: KALYDECO is not recommended.
- No dose adjustment is necessary for patients aged 6 months or older [see Clinical Pharmacology (12.3)].
-
Moderate Hepatic Impairment (Child-Pugh Class B):
- Less than 6 months of age: KALYDECO is not recommended.
- 6 months to less than 6 years of age: one packet (containing 25 mg, 50 mg, or 75 mg ivacaftor) of oral granules once daily based on dosing recommended for age and weight in Table 1 [see Dosage and Administration (2.2)].
- 6 years of age and older: 150 mg orally once daily.
-
Severe Hepatic Impairment (Child-Pugh Class C): Should not be used in patients less than 6 months of age. In patients 6 months and older should be used with caution. KALYDECO has not been studied in patients with severe hepatic impairment (Child-Pugh Class C), but exposure is expected to be higher than in patients with moderate hepatic impairment. Therefore, use with caution at a reduced dose, in patients aged 6 months or older with severe hepatic impairment after weighing the risks and benefits of treatment [see Dosage and Administration (2.1, 2.2) and Clinical Pharmacology (12.3)].
- Less than 6 months of age: KALYDECO is not recommended.
- 6 months to less than 6 years of age: one packet (containing 25 mg, 50 mg, or 75 mg ivacaftor) of oral granules once daily or less frequently based on dosing recommended for age and weight in Table 1 [see Dosage and Administration (2.2)].
- 6 years of age and older: 150 mg orally once daily or less frequently.
2.4 Dosage Modification for Patients Taking Drugs that are CYP3A Inhibitors
Concomitant use of moderate or strong CYP3A inhibitors is not recommended in patients below 6 months of age. Food or drink containing grapefruit should be avoided [see Drug Interactions (7.1), Clinical Pharmacology (12.3)]. Take KALYDECO with fat-containing food [see Dosage and Administration (2.5)].
Dosage modification for patients 6 months of age and older taking CYP3A inhibitors:
-
Moderate CYP3A inhibitors:
- Less than 6 months of age: KALYDECO is not recommended.
- 6 months to less than 6 years of age: one packet (containing 25 mg, 50 mg, or 75 mg ivacaftor) of oral granules once daily based on dosing recommended for age and weight in Table 1 [see Dosage and Administration (2.2)].
- 6 years of age and older: 150 mg orally once daily.
-
Strong CYP3A inhibitors:
- Less than 6 months of age: KALYDECO is not recommended.
- 6 months to less than 6 years of age: one packet (containing 25 mg, 50 mg, or 75 mg ivacaftor) of oral granules twice a week based on dosing recommended for age and weight in Table 1 [see Dosage and Administration (2.2)].
- 6 years of age and older: 150 mg orally twice weekly.
2.5 Administration Information
Administer KALYDECO tablets or oral granules with fat-containing food. Examples include eggs, butter, peanut butter, cheese pizza, whole-milk dairy products (such as whole milk, cheese, yogurt, breast milk, or infant formula), etc. [see Clinical Pharmacology (12.3)].
Instruction for Administration of Oral Granules
Administer each dose of KALYDECO oral granules immediately before or after ingestion of fat-containing food. Mix the entire contents of each packet of oral granules with one teaspoon (5 mL) of age-appropriate soft food or liquid that is at or below room temperature. Some examples of soft foods or liquids may include puréed fruits or vegetables, yogurt, applesauce, water, breast milk, infant formula, milk, or juice. Food or liquid should be at or below room temperature. Once mixed, the product should be completely consumed within one hour.
3. Dosage Forms and Strengths
Tablets: 150 mg, light blue, film-coated, capsule shaped tablets, with the characters "V 150" on one side and plain on the other.
Oral granules: 5.8 mg, 13.4 mg, 25 mg, 50 mg, or 75 mg, white to off-white granules, in unit-dose packets.
5. Warnings and Precautions
5.1 Transaminase (ALT or AST) Elevations
Elevated transaminases have been reported in patients with CF receiving KALYDECO. ALT and AST should be assessed prior to initiating KALYDECO, every 3 months during the first year of treatment, and annually thereafter. For patients with a history of transaminase elevations, consider more frequent monitoring of liver function tests. Patients who develop increased transaminase levels should be closely monitored until the abnormalities resolve. Dosing should be interrupted in patients with ALT or AST of greater than 5 times the upper limit of normal (ULN). Following resolution of transaminase elevations, consider the benefits and risks of resuming KALYDECO [see Adverse Reactions (6) and Use in Specific Populations (8.6)].
5.2 Hypersensitivity Reactions, Including Anaphylaxis
Hypersensitivity reactions, including cases of anaphylaxis, have been reported in the postmarketing setting [see Adverse Reactions (6.2)]. If signs or symptoms of serious hypersensitivity reactions develop during treatment, discontinue KALYDECO and institute appropriate therapy. Consider the benefits and risks for the individual patient to determine whether to resume treatment with KALYDECO.
5.3 Concomitant Use with CYP3A Inducers
Use of KALYDECO with strong CYP3A inducers, such as rifampin, substantially decreases the exposure of ivacaftor, which may reduce the therapeutic effectiveness of KALYDECO. Therefore, co-administration of KALYDECO with strong CYP3A inducers (e.g., rifampin, St. John's wort) is not recommended [see Drug Interactions (7.2) and Clinical Pharmacology (12.3)].
5.4 Cataracts
Cases of non-congenital lens opacities/cataracts have been reported in pediatric patients treated with KALYDECO. Although other risk factors were present in some cases (such as corticosteroid use and/or exposure to radiation), a possible risk attributable to KALYDECO cannot be excluded. Baseline and follow-up ophthalmological examinations are recommended in pediatric patients initiating KALYDECO treatment.
6. Adverse Reactions/Side Effects
The following adverse reactions are discussed in greater detail in other sections of the labeling:
- Transaminase Elevations [see Warnings and Precautions (5.1)]
- Hypersensitivity Reactions, Including Anaphylaxis [see Warnings and Precautions (5.2)]
- Cataracts [see Warnings and Precautions (5.4)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
The overall safety profile of KALYDECO is based on pooled data from three placebo-controlled clinical trials conducted in 353 patients 6 years of age and older with CF who had a G551D mutation in the CFTR gene (Trials 1 and 2) or were homozygous for the F508del mutation (Trial 3). In addition, the following clinical trials have also been conducted [see Clinical Pharmacology (12) and Clinical Studies (14)]:
- An 8-week, crossover design trial (Trial 4) involving 39 patients between the ages of 6 and 57 years with a G1244E, G1349D, G178R, G551S, G970R, S1251N, S1255P, S549N, or S549R mutation in the CFTR gene.
- A 24-week, placebo-controlled trial (Trial 5) involving 69 patients between the ages of 6 and 68 years with an R117H mutation in the CFTR gene.
- A 24-week, open-label trial (Trial 6) in 34 patients 2 to less than 6 years of age. Patients eligible for Trial 6 were those with the G551D, G1244E, G1349D, G178R, G551S, G970R, S1251N, S1255P, S549N, or S549R mutation in the CFTR gene. Of 34 patients enrolled, 32 had the G551D mutation and 2 had the S549N mutation.
- An 8-week, crossover design trial (Trial 7) involving patients between the ages of 12 and 72 years who were heterozygous for the F508del mutation and a second CFTR mutation predicted to be responsive to ivacaftor. A total of 156 patients were randomized to and received KALYDECO.
- A 24-week open-label clinical trial in patients with CF aged less than 24 months (Trial 8) including a cohort of 19 patients aged 12 months to less than 24 months, a cohort of 11 patients aged 6 months to less than 12 months, a cohort of 6 patients aged 4 months to less than 6 months, and a cohort of 7 patients aged 1 month to less than 4 months. Patients with a gating mutation or R117H mutation were eligible for the first three cohorts of this study. Patients with any ivacaftor-responsive mutation were eligible for the cohort aged 1 to less than 4 months.
Of the 353 patients included in the pooled analyses of patients with CF who had either a G551D mutation or were homozygous for the F508del mutation in the CFTR gene, 50% of patients were female and 97% were Caucasian; 221 received KALYDECO, and 132 received placebo for 16 to 48 weeks.
The proportion of patients who prematurely discontinued study drug due to adverse reactions was 2% for KALYDECO-treated patients and 5% for placebo-treated patients. Serious adverse reactions, whether considered drug-related or not by the investigators, that occurred more frequently in KALYDECO-treated patients, included abdominal pain, increased hepatic enzymes, and hypoglycemia.
The most common adverse reactions in the 221 patients treated with KALYDECO were headache (17%), upper respiratory tract infection (16%), nasal congestion (16%), nausea (10%), rash (10%), rhinitis (6%), dizziness (5%), arthralgia (5%), and bacteria in sputum (5%).
The incidence of adverse reactions below is based upon two double-blind, placebo-controlled, 48-week clinical trials (Trials 1 and 2) in a total of 213 patients with CF ages 6 to 53 who have a G551D mutation in the CFTR gene and who were treated with KALYDECO 150 mg orally or placebo twice daily. Table 2 shows adverse reactions occurring in ≥8% of KALYDECO-treated patients with CF who have a G551D mutation in the CFTR gene that also occurred at a higher rate than in the placebo-treated patients in the two double-blind, placebo-controlled trials.
| Adverse Reaction (Preferred Term) | Incidence: Pooled 48-Week Trials | |
|---|---|---|
| KALYDECO N=109 n (%) | Placebo N=104 n (%) |
|
| Headache | 26 (24) | 17 (16) |
| Oropharyngeal pain | 24 (22) | 19 (18) |
| Upper respiratory tract infection | 24 (22) | 14 (14) |
| Nasal congestion | 22 (20) | 16 (15) |
| Abdominal pain | 17 (16) | 13 (13) |
| Nasopharyngitis | 16 (15) | 12 (12) |
| Diarrhea | 14 (13) | 10 (10) |
| Rash | 14 (13) | 7 (7) |
| Nausea | 13 (12) | 11 (11) |
| Dizziness | 10 (9) | 1 (1) |
Adverse reactions in the 48-week clinical trials that occurred in the KALYDECO group at a frequency of 4 to 7% where rates exceeded that in the placebo group include:
- Infections and infestations: rhinitis
- Investigations: aspartate aminotransferase increased, bacteria in sputum, blood glucose increased, hepatic enzyme increased
- Musculoskeletal and connective tissue disorders: arthralgia, musculoskeletal chest pain, myalgia
- Nervous system disorders: sinus headache
- Respiratory, thoracic and mediastinal disorders: pharyngeal erythema, pleuritic pain, sinus congestion, wheezing
- Skin and subcutaneous tissue disorders: acne
The safety profile for the CF patients enrolled in the other clinical trials (Trials 3-8) was similar to that observed in the 48-week, placebo-controlled trials (Trials 1 and 2).
Laboratory Abnormalities
Transaminase Elevations: In Trials 1, 2, and 3 the incidence of maximum transaminase (ALT or AST) >8, >5, or >3 × ULN was 2%, 2%, and 6% in KALYDECO-treated patients and 2%, 2%, and 8% in placebo-treated patients, respectively. Two patients (2%) on placebo and 1 patient (0.5%) on KALYDECO permanently discontinued treatment for elevated transaminases, all >8 × ULN. Two patients treated with KALYDECO were reported to have serious adverse reactions of elevated liver transaminases compared to none on placebo. Transaminase elevations were more common in patients with a history of transaminase elevations [see Warnings and Precautions (5.1)].
During the 24-week, open-label, clinical trial in 34 patients ages 2 to less than 6 years (Trial 6), where patients received either 50 mg (less than 14 kg) or 75 mg (14 kg or greater) ivacaftor granules twice daily, the incidence of patients experiencing transaminase elevations (ALT or AST) >3 × ULN was 14.7% (5/34). All 5 patients had maximum ALT or AST levels >8 × ULN, which returned to baseline levels following interruption of KALYDECO dosing. Transaminase elevations were more common in patients who had abnormal transaminases at baseline. KALYDECO was permanently discontinued in one patient [see Warnings and Precautions (5.1)].
During the 24-week, open-label, clinical trial in patients aged less than 24 months (Trial 8), the incidence of patients experiencing transaminase elevations (ALT or AST) >3, >5, and >8 × ULN in the cohort of patients aged 12 months to less than 24 months (N=19) was 27.8% (5/18), 11.1% (2/18) and 11.1% (2/18), respectively. In the cohort of patients aged 6 months to less than 12 months (N=11) one patient (9.1%) had elevated ALT of >3 to ≤5 × ULN. In the cohort of patients aged 4 months to less than 6 months (N=6), no patients had elevated ALT or AST (>3× ULN). In the cohort of patients aged 1 month to less than 4 months (N=7), 1 patient (14.3%) had maximum ALT or AST >3 × ULN (ALT >8 × ULN and AST of >3 to ≤5 × ULN); the patient discontinued ivacaftor treatment. [see Warnings and Precautions (5.1)].
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of KALYDECO. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune System Disorders: anaphylaxis
7. Drug Interactions
Potential for other drugs to affect ivacaftor
7.1 Inhibitors of CYP3A
Ivacaftor is a sensitive CYP3A substrate. Co-administration with ketoconazole, a strong CYP3A inhibitor, significantly increased ivacaftor exposure [measured as area under the curve (AUC)] by 8.5-fold. Based on simulations of these results, a reduction of the KALYDECO dose is recommended for patients 6 months and older taking concomitant strong CYP3A inhibitors, such as ketoconazole, itraconazole, posaconazole, voriconazole, telithromycin, and clarithromycin. KALYDECO is not recommended for patients less than 6 months of age taking strong CYP3A inhibitors [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3)].
Co-administration with fluconazole, a moderate inhibitor of CYP3A, increased ivacaftor exposure by 3-fold. Therefore, a reduction of the KALYDECO dose is recommended for patients 6 months and older taking concomitant moderate CYP3A inhibitors, such as fluconazole and erythromycin. KALYDECO is not recommended for patients less than 6 months of age taking moderate CYP3A inhibitors [see Dosage and Administration (2.4) and Clinical Pharmacology (12.3)].
Co-administration of KALYDECO with grapefruit juice, which contains one or more components that moderately inhibit CYP3A, may increase exposure of ivacaftor. Therefore, avoid food or drink containing grapefruit during treatment with KALYDECO [see Clinical Pharmacology (12.3)].
7.2 Inducers of CYP3A
Co-administration with rifampin, a strong CYP3A inducer, significantly decreased ivacaftor exposure (AUC) by approximately 9-fold. Therefore, co-administration with strong CYP3A inducers, such as rifampin, rifabutin, phenobarbital, carbamazepine, phenytoin, and St. John's wort is not recommended [see Warnings and Precautions (5.3) and Clinical Pharmacology (12.3)].
7.3 Ciprofloxacin
Co-administration of KALYDECO with ciprofloxacin had no effect on the exposure of ivacaftor. Therefore, no dose adjustment is necessary during concomitant administration of KALYDECO with ciprofloxacin [see Clinical Pharmacology (12.3)].
Potential for ivacaftor to affect other drugs
7.4 CYP2C9 Substrates
Ivacaftor may inhibit CYP2C9; therefore, monitoring of the international normalized ratio (INR) during co-administration of KALYDECO with warfarin is recommended. Other therapeutic products for which exposure may be increased by KALYDECO include glimepiride and glipizide; these therapeutic products should be used with caution [see Clinical Pharmacology (12.3)].
7.5 CYP3A and/or P-gp Substrates
Ivacaftor and its M1 metabolite have the potential to inhibit CYP3A and P-gp. Co-administration with oral midazolam, a sensitive CYP3A substrate, increased midazolam exposure 1.5-fold, consistent with weak inhibition of CYP3A by ivacaftor. Co-administration with digoxin, a sensitive P-gp substrate, increased digoxin exposure by 1.3-fold, consistent with weak inhibition of P-gp by ivacaftor. Administration of KALYDECO may increase systemic exposure of drugs that are substrates of CYP3A and/or P-gp, which may increase or prolong their therapeutic effect and adverse events. Therefore, caution and appropriate monitoring are recommended when co-administering KALYDECO with sensitive CYP3A and/or P-gp substrates, such as digoxin, cyclosporine, and tacrolimus [see Clinical Pharmacology (12.3)].
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
There are limited and incomplete human data from clinical trials and postmarketing reports on use of KALYDECO in pregnant women. In animal reproduction studies, oral administration of ivacaftor to pregnant rats and rabbits during organogenesis demonstrated no teratogenicity or adverse effects on fetal development at doses that produced maternal exposures up to approximately 5 (rats) and 11 (rabbits) times the exposure at the maximum recommended human dose (MRHD). No adverse developmental effects were observed after oral administration of ivacaftor to pregnant rats from organogenesis through lactation at doses that produced maternal exposures approximately 3 times the exposures at the MRHD, respectively (see Data).
The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects is 2% to 4% and miscarriage is 15% to 20% in clinically recognized pregnancies.
Data
Animal Data
In an embryo-fetal development study in pregnant rats dosed during the period of organogenesis from gestation days 7-17, ivacaftor was not teratogenic and did not affect fetal survival at exposures up to 5 times the MRHD (based on summed AUCs for ivacaftor and its metabolites at maternal oral doses up to 200 mg/kg/day). In an embryo-fetal development study in pregnant rabbits dosed during the period of organogenesis from gestation days 7-19, ivacaftor was not teratogenic and did not affect fetal development or survival at exposures up to 11 times the MRHD (on an ivacaftor AUC basis at maternal oral doses up to 100 mg/kg/day). In a pre- and post-natal development study in pregnant female rats dosed from gestation day 7 through lactation day 20, ivacaftor had no effects on delivery or growth and development of offspring at exposures up to 3 times the MRHD (based on summed AUCs for ivacaftor and its metabolites at maternal oral doses up to 100 mg/kg/day). Decreased fetal body weights were observed at a maternally toxic dose that produced exposures 5 times the MRHD (based on summed AUCs for ivacaftor and its metabolites at a maternal oral dose of 200 mg/kg/day). Placental transfer of ivacaftor was observed in pregnant rats and rabbits.
8.2 Lactation
Risk Summary
There is no information regarding the presence of ivacaftor in human milk, the effects on the breastfed infant, or the effects on milk production. Ivacaftor is excreted into the milk of lactating rats; however, due to species-specific differences in lactation physiology, animal lactation data may not reliably predict levels in human milk (see Data). The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for KALYDECO, and any potential adverse effects on the breastfed child from KALYDECO or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of KALYDECO for the treatment of CF have been established in pediatric patients 1 month to 17 years of age who have at least one mutation in the CFTR gene that is responsive to ivacaftor potentiation based on clinical and/or in vitro assay data [see Clinical Pharmacology (12.1) and Clinical Studies (14)].
The use of KALYDECO for this indication is supported by evidence from placebo-controlled clinical trials in the following pediatric patients with CF:
- 6 to 17 years of age with a G551D, G1244E, G1349D, G178R, G551S, S1251N, S1255P, S549N, S549R, or R117H mutation in the CFTR gene [see Adverse Reactions (6) and Clinical Studies (14)].
- 12 to 17 years of age who are heterozygous for the F508del mutation and a second mutation predicted to be responsive to ivacaftor [see Adverse Reactions (6) and Clinical Studies (14)].
The effectiveness of KALYDECO in patients aged 2 to less than 6 years was extrapolated from patients 6 years of age and older with support from population pharmacokinetic analyses showing similar drug exposure levels in adults and pediatric patients 2 to less than 6 years of age [see Clinical Pharmacology (12.3)]. Safety of KALYDECO in this population was derived from a 24-week, open-label clinical trial in 34 patients ages 2 to less than 6 years (mean age 3 years) administered either 50 mg or 75 mg of ivacaftor granules twice daily (Trial 6). The type and frequency of adverse reactions in this trial were similar to those in patients 6 years and older. Transaminase elevations were more common in patients who had abnormal transaminases at baseline [see Warnings and Precautions (5.1) and Adverse Reactions (6.1)].
The effectiveness of KALYDECO in patients aged 1 month to less than 24 months was extrapolated from patients 6 years of age and older with support from population pharmacokinetic analyses showing that the exposure of ivacaftor in pediatric patients 1 month to less than 24 months of age is within the range of exposure in adults and pediatric patients 6 years of age and older [see Clinical Pharmacology (12.3)]. Safety of KALYDECO in this population was derived from a cohort of 7 patients aged 1 month to less than 4 months (mean age 1.9 months at baseline), a cohort of 6 patients aged 4 months to less than 6 months (mean age 4.5 months at baseline), a cohort of 11 patients aged 6 months to less than 12 months (mean age 9.0 months at baseline), and a cohort of 19 patients aged 12 months to less than 24 months (mean age 15.2 months at baseline) in a 24-week, open-label clinical trial, administered 5.8 mg, 11.4 mg, 17.1 mg, 22.8 mg, 25 mg, 50 mg, or 75 mg (11.4 mg, 17.1 mg, and 22.8 mg are not recommended dosages) of ivacaftor granules twice daily (Trial 8). The safety profile of patients in this trial was similar to that observed in patients 2 years and older.
The safety and effectiveness of KALYDECO in pediatric patients with CF younger than 1 month of age have not been established.
Juvenile Animal Toxicity Data
In a juvenile toxicology study in which ivacaftor was administered to rats from postnatal days 7 to 35, cataracts were observed at all dose levels, ranging from 0.1 to 0.8 times the MRHD (based on summed AUCs for ivacaftor and its metabolites at oral doses of 10-50 mg/kg/day). This finding has not been observed in older animals.
8.5 Geriatric Use
CF is largely a disease of children and young adults. Clinical trials of KALYDECO did not include sufficient numbers of patients 65 years of age and over to determine whether they respond differently from younger patients.
8.6 Hepatic Impairment
- Mild Hepatic Impairment (Child-Pugh Class A): No dose adjustment is necessary for patients aged 6 months or older [see Clinical Pharmacology (12.3)].
- Moderate Hepatic Impairment (Child-Pugh Class B): A reduced dose is recommended in patients aged 6 months or older [see Dosage and Administration (2.3) and Clinical Pharmacology (12.3)].
- Severe Hepatic Impairment (Child-Pugh Class C): Studies have not been conducted in patients with severe hepatic impairment (Child-Pugh Class C), but exposure is expected to be higher than in patients with moderate hepatic impairment. Therefore, use with caution at a reduced dose, in patients aged 6 months or older with severe hepatic impairment after weighing the risks and benefits of treatment [see Dosage and Administration (2.3) and Clinical Pharmacology (12.3)].
Due to variability in maturation of cytochrome (CYP) enzymes involved in ivacaftor metabolism, treatment with KALYDECO is not recommended in patients aged 1 month to less than 6 months with any level of hepatic impairment [see Dosage and Administration (2.3)].
8.7 Renal Impairment
KALYDECO has not been studied in patients with mild, moderate, or severe renal impairment or in patients with end-stage renal disease. No dose adjustment is necessary for patients with mild to moderate renal impairment; however, caution is recommended while using KALYDECO in patients with severe renal impairment (creatinine clearance less than or equal to 30 mL/min) or end-stage renal disease.
10. Overdosage
There have been no reports of overdose with KALYDECO.
No specific antidote is available for overdose with KALYDECO. Treatment of overdose with KALYDECO consists of general supportive measures including monitoring of vital signs and observation of the clinical status of the patient.
11. Kalydeco Description
The active ingredient in KALYDECO tablets and oral granules is ivacaftor, a cystic fibrosis transmembrane conductance regulator potentiator, which has the following chemical name: N-(2,4-di-tert-butyl-5-hydroxyphenyl)-1,4-dihydro-4-oxoquinoline-3-carboxamide. Its molecular formula is C24H28N2O3 and its molecular weight is 392.49. Ivacaftor has the following structural formula:
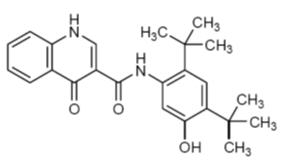
Ivacaftor is a white to off-white powder that is practically insoluble in water (<0.05 microgram/mL).
KALYDECO is available as a light blue, capsule shaped, film-coated tablet for oral administration containing 150 mg of ivacaftor. Each KALYDECO tablet contains 150 mg of ivacaftor and the following inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hypromellose acetate succinate, lactose monohydrate, magnesium stearate, microcrystalline cellulose, and sodium lauryl sulfate. The tablet film coat contains carnauba wax, FD&C Blue #2, PEG 3350, polyvinyl alcohol, talc, and titanium dioxide. The printing ink contains ammonium hydroxide, iron oxide black, propylene glycol, and shellac.
KALYDECO is also available as white to off-white granules for oral administration (sweetened but unflavored) and enclosed in a unit-dose packet containing 5.8 mg of ivacaftor, 13.4 mg of ivacaftor, 25 mg of ivacaftor, 50 mg of ivacaftor, or 75 mg of ivacaftor. Each unit-dose packet of KALYDECO oral granules contains 5.8 mg of ivacaftor, 13.4 mg of ivacaftor, 25 mg of ivacaftor, 50 mg of ivacaftor, or 75 mg of ivacaftor and the following inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hypromellose acetate succinate, lactose monohydrate, magnesium stearate, mannitol, sucralose, and sodium lauryl sulfate.
12. Kalydeco - Clinical Pharmacology
12.1 Mechanism of Action
Ivacaftor is a potentiator of the CFTR protein. The CFTR protein is a chloride channel present at the surface of epithelial cells in multiple organs. Ivacaftor facilitates increased chloride transport by potentiating the channel open probability (or gating) of CFTR protein located at the cell surface. The overall level of ivacaftor-mediated CFTR chloride transport is dependent on the amount of CFTR protein at the cell surface and how responsive a particular mutant CFTR protein is to ivacaftor potentiation.
CFTR Chloride Transport Assay in Fisher Rat Thyroid (FRT) cells expressing mutant CFTR
The chloride transport response of mutant CFTR protein to ivacaftor was determined in Ussing chamber electrophysiology studies using a panel of FRT cell lines transfected with individual CFTR mutations. Ivacaftor increased chloride transport in FRT cells expressing CFTR mutations that result in CFTR protein being delivered to the cell surface.
The in vitro CFTR chloride transport response threshold was designated as a net increase of at least 10% of normal over baseline because it is predictive or reasonably expected to predict clinical benefit. For individual mutations, the magnitude of the net change over baseline in CFTR-mediated chloride transport in vitro is not correlated with the magnitude of clinical response. A patient must have at least one CFTR mutation responsive to ivacaftor to be indicated.
Note that splice site mutations cannot be studied in the FRT assay. Evidence of clinical efficacy exists for non-canonical splice mutations 2789+5G→A, 3272-26A→G, 3849+10kbC→T, 711+3A→G and E831X and these are listed in Table 3 below [see also Clinical Studies (14.4)]. The G970R mutation causes a splicing defect resulting in little-to-no CFTR protein at the cell surface that can be potentiated by ivacaftor [see Clinical Studies (14.2)].
Ivacaftor also increased chloride transport in cultured human bronchial epithelial (HBE) cells derived from CF patients who carried F508del on one CFTR allele and either G551D or R117H-5T on the second CFTR allele.
Table 3 lists mutations that are responsive to ivacaftor based on 1) a positive clinical response and/or 2) in vitro data in FRT cells indicating that ivacaftor increases chloride transport to at least 10% over baseline (% of normal).
|
||||
| 711+3A→G * | F311del | I148T | R75Q | S589N |
| 2789+5G→A * | F311L | I175V | R117C * | S737F |
| 3272-26A→G * | F508C | I807M | R117G | S945L * |
| 3849+10kbC→T * | F508C;S1251N † | I1027T | R117H * | S977F * |
| A120T | F1052V | I1139V | R117L | S1159F |
| A234D | F1074L | K1060T | R117P | S1159P |
| A349V | G178E | L206W * | R170H | S1251N * |
| A455E * | G178R * | L320V | R347H * | S1255P * |
| A1067T | G194R | L967S | R347L | T338I |
| D110E | G314E | L997F | R352Q * | T1053I |
| D110H | G551D * | L1480P | R553Q | V232D |
| D192G | G551S * | M152V | R668C | V562I |
| D579G * | G576A | M952I | R792G | V754M |
| D924N | G970D | M952T | R933G | V1293G |
| D1152H * | G1069R | P67L * | R1070Q | W1282R |
| D1270N | G1244E * | Q237E | R1070W * | Y1014C |
| E56K | G1249R | Q237H | R1162L | Y1032C |
| E193K | G1349D * | Q359R | R1283M | |
| E822K | H939R | Q1291R | S549N * | |
| E831X * | H1375P | R74W | S549R * | |
12.2 Pharmacodynamics
Sweat Chloride Evaluation
Changes in sweat chloride (a biomarker) response to KALYDECO were evaluated in seven clinical trials [see Clinical Studies (14)]. In a two-part, randomized, double-blind, placebo-controlled, crossover clinical trial in patients with CF who had a G1244E, G1349D, G178R, G551S, G970R, S1251N, S1255P, S549N, or S549R mutation in the CFTR gene (Trial 4), the treatment difference in mean change in sweat chloride from baseline through 8 weeks of treatment was -49 mmol/L (95% CI -57, -41). The mean changes in sweat chloride for the mutations for which KALYDECO is indicated ranged from -51 to -8, whereas the range for individual subjects with the G970R mutation was -1 to -11 mmol/L. In an open-label clinical trial in 34 patients ages 2 to less than 6 years administered either 50 mg or 75 mg of ivacaftor twice daily (Trial 6), the mean absolute change from baseline in sweat chloride through 24 weeks of treatment was -45 mmol/L (95% CI -53, -38) [see Use in Specific Populations (8.4)]. In a randomized, double-blind, placebo-controlled, 2-period, 3-treatment, 8-week crossover study in patients with CF age 12 years and older who were heterozygous for the F508del mutation and with a second CFTR mutation predicted to be responsive to ivacaftor (Trial 7), the treatment difference in mean change in sweat chloride from study baseline to the average of Week 4 and Week 8 of treatment for KALYDECO treated patients was -4.5 mmol/L (95% CI -6.7, -2.3). In a 24-week, open-label clinical trial in patients with CF aged less than 24 months administered 5.8 mg, 11.4 mg, 17.1 mg, 22.8 mg, 25 mg, 50 mg, or 75 mg (11.4 mg, 17.1 mg, and 22.8 mg are not recommended dosages) of ivacaftor twice daily (Trial 8), the mean absolute change from baseline in sweat chloride for patients aged 12 months to less than 24 months (n=10) was -73.5 mmol/L (95% CI -86.0, -61.0) at Week 24, the mean absolute change from baseline in sweat chloride for patients aged 6 months to less than 12 months (n=6) was -58.6 mmol/L (95% CI -75.9, -41.3) at Week 24, and the mean absolute change from baseline in sweat chloride for patients aged 4 months to less than 6 months (n=3) was -50 mmol/L (95% CI -93.1, -6.9) at Week 24. The mean absolute change from baseline in sweat chloride through 24 weeks for patients aged 1 month to less than 4 months (n=5) was -40.3 mmol/L (95% CI -76.6, -4.1) [see Use in Specific Populations (8.4)].
There was no direct correlation between decrease in sweat chloride levels and improvement in lung function (FEV1).
Cardiac Electrophysiology
The effect of multiple doses of ivacaftor 150 mg and 450 mg twice daily on QTc interval was evaluated in a randomized, placebo- and active-controlled (moxifloxacin 400 mg) four-period crossover thorough QT study in 72 healthy subjects. In a study with demonstrated ability to detect small effects, the upper bound of the one-sided 95% confidence interval for the largest placebo adjusted, baseline-corrected QTc based on Fridericia's correction method (QTcF) was below 10 ms, the threshold for regulatory concern.
12.3 Pharmacokinetics
The pharmacokinetics of ivacaftor is similar between healthy adult volunteers and patients with CF.
After oral administration of a single 150 mg dose to healthy volunteers in a fed state, peak plasma concentrations (Tmax) occurred at approximately 4 hours, and the mean (±SD) for AUC and Cmax were 10600 (5260) ng*hr/mL and 768 (233) ng/mL, respectively.
After every 12-hour dosing, steady-state plasma concentrations of ivacaftor were reached by days 3 to 5, with an accumulation ratio ranging from 2.2 to 2.9.
Absorption
The exposure of ivacaftor increased approximately 2.5- to 4-fold when given with food that contains fat. Therefore, KALYDECO should be administered with fat-containing food. Examples of fat-containing foods include eggs, butter, peanut butter, cheese pizza, whole-milk dairy products (such as whole milk, cheese, yogurt, breast milk, and infant formula), etc. The median (range) Tmax is approximately 4.0 (3.0; 6.0) hours in the fed state.
KALYDECO granules (2 × 75 mg) had similar bioavailability as the 150 mg tablet when given with fat-containing food in adult subjects. The effect of food on ivacaftor absorption is similar for KALYDECO granules and the 150 mg tablet formulation.
Distribution
Ivacaftor is approximately 99% bound to plasma proteins, primarily to alpha 1-acid glycoprotein and albumin. Ivacaftor does not bind to human red blood cells.
After oral administration of 150 mg every 12 hours for 7 days to healthy volunteers in a fed state, the mean (±SD) for apparent volume of distribution was 353 (122) L.
Elimination
The apparent terminal half-life was approximately 12 hours following a single dose. The mean apparent clearance (CL/F) of ivacaftor was similar for healthy subjects and patients with CF. The CL/F (SD) for the 150 mg dose was 17.3 (8.4) L/hr in healthy subjects.
Metabolism
Ivacaftor is extensively metabolized in humans. In vitro and clinical studies indicate that ivacaftor is primarily metabolized by CYP3A. M1 and M6 are the two major metabolites of ivacaftor in humans. M1 has approximately one-sixth the potency of ivacaftor and is considered pharmacologically active. M6 has less than one-fiftieth the potency of ivacaftor and is not considered pharmacologically active.
Excretion
Following oral administration, the majority of ivacaftor (87.8%) is eliminated in the feces after metabolic conversion. The major metabolites M1 and M6 accounted for approximately 65% of the total dose eliminated with 22% as M1 and 43% as M6. There was negligible urinary excretion of ivacaftor as unchanged parent.
Specific Populations
Pediatric Patients
The following conclusions about exposures between adults and the pediatric population are based on population PK analyses:
| Age Group | Dose | AUCss (ng∙h/mL) |
|---|---|---|
|
||
| 1 to less than 2 months (≥3 kg) * | 5.8 mg q12h | 5490 (1310) |
| 2 to less than 4 months (≥3 kg) * | 13.4 mg q12h | 6730 (3650) † |
| 4 to less than 6 months (≥5 kg) * | 25 mg q12h | 6480 (2520) ‡ |
| 6 to less than 12 months (5 kg to <7 kg) § | 25 mg q12h | 5360 ‡ |
| 6 to less than 12 months (7 kg to <14 kg) | 50 mg q12h | 9390 (3120) ‡ |
| 12 to less than 24 months (7 kg to <14 kg) | 50 mg q12h | 9050 (3050) |
| 12 to less than 24 months (≥14 kg to <25 kg) | 75 mg q12h | 9600 (1800) |
| 2 to less than 6 years (<14 kg) | 50 mg q12h | 10500 (4260) |
| 2 to less than 6 years (≥14 kg to <25 kg) | 75 mg q12h | 11300 (3820) |
| 6 to less than 12 years | 150 mg q12h | 20000 (8330) |
| 12 to less than 18 years | 150 mg q12h | 9240 (3420) |
| Adults (≥18 years) | 150 mg q12h | 10700 (4100) |
Patients with Hepatic Impairment
Adult subjects with moderately impaired hepatic function (Child-Pugh Class B, score 7 -9) had similar ivacaftor Cmax, but an approximately two-fold increase in ivacaftor AUC0-∞ compared with healthy subjects matched for demographics. Based on simulations of these results, a reduced KALYDECO dose to one tablet or packet of granules once daily is recommended for patients with moderate hepatic impairment aged 6 months and older. The impact of mild hepatic impairment (Child-Pugh Class A) on the pharmacokinetics of ivacaftor has not been studied, but the increase in ivacaftor AUC0-∞ is expected to be less than two-fold. Therefore, no dose adjustment is necessary for patients with mild hepatic impairment aged 6 months and older. The impact of severe hepatic impairment (Child-Pugh Class C, score 10-15) on the pharmacokinetics of ivacaftor has not been studied. The magnitude of increase in exposure in these patients is unknown but is expected to be substantially higher than that observed in patients with moderate hepatic impairment. When benefits are expected to outweigh the risks, KALYDECO should be used with caution in patients with severe hepatic impairment aged 6 months and older at a dose of one tablet or one packet of granules given once daily or less frequently [see Dosage and Administration (2.3) and Use in Specific Populations (8.6)]. KALYDECO is not recommended in patients aged 1 month to less than 6 months with any level of hepatic impairment.
Patients with Renal Impairment
KALYDECO has not been studied in patients with mild, moderate, or severe renal impairment (creatinine clearance less than or equal to 30 mL/min) or in patients with end-stage renal disease. No dose adjustments are recommended for mild and moderate renal impairment patients because of minimal elimination of ivacaftor and its metabolites in urine (only 6.6% of total radioactivity was recovered in the urine in a human PK study); however, caution is recommended when administering KALYDECO to patients with severe renal impairment or end-stage renal disease.
Male and Female Patients
The effect of gender on KALYDECO pharmacokinetics was evaluated using population pharmacokinetics of data from clinical studies of KALYDECO. No dose adjustments are necessary based on gender.
Drug Interaction Studies
Drug interaction studies were performed with KALYDECO and other drugs likely to be co-administered or drugs commonly used as probes for pharmacokinetic interaction studies [see Drug Interactions (7)].
Dosing recommendations based on clinical studies or potential drug interactions with KALYDECO are presented below.
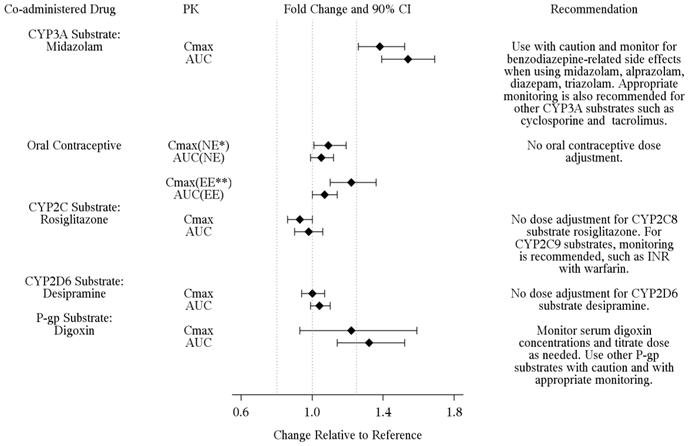
Potential for Ivacaftor to Affect Other Drugs
Based on in vitro results, ivacaftor and metabolite M1 have the potential to inhibit CYP3A and P-gp. Clinical studies showed that KALYDECO is a weak inhibitor of CYP3A and P-gp, but not an inhibitor of CYP2C8. In vitro studies suggest that ivacaftor and M1 may inhibit CYP2C9. In vitro, ivacaftor, M1, and M6 were not inducers of CYP isozymes. Dosing recommendations for co-administered drugs with KALYDECO are shown in Figure 2.
| Figure 2: Impact of KALYDECO on Other Drugs |
|---|
| Note: The data obtained with substrates but without co-administration of KALYDECO are used as reference. * NE: Norethindrone; ** EE: Ethinyl Estradiol The vertical lines are at 0.8, 1.0, and 1.25, respectively. |
|
|
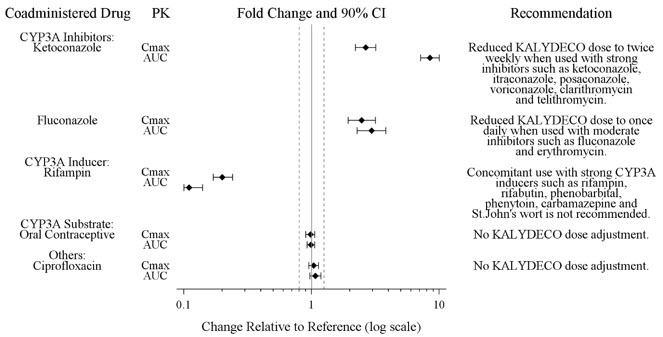
Potential for Other Drugs to Affect Ivacaftor
In vitro studies showed that ivacaftor and metabolite M1 were substrates of CYP3A enzymes (i.e., CYP3A4 and CYP3A5). Exposure to ivacaftor is reduced by concomitant CYP3A inducers and increased by concomitant CYP3A inhibitors [see Dosage and Administration (2.4) and Drug Interactions (7)]. KALYDECO dosing recommendations for co-administration with other drugs are shown in Figure 3.
| Figure 3: Impact of Other Drugs on KALYDECO |
|---|
| Note: The data obtained for KALYDECO without co-administration of inducers or inhibitors are used as reference. The vertical lines are at 0.8, 1.0, and 1.25, respectively. |
|
|
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Two-year studies were conducted in CD-1 mice and Sprague-Dawley rats to assess carcinogenic potential of KALYDECO. No evidence of tumorigenicity was observed in mice or rats at ivacaftor oral doses up to 200 mg/kg/day and 50 mg/kg/day, respectively (approximately equal to 1 and 4 times the MRHD based on summed AUCs of ivacaftor and its metabolites).
Ivacaftor was negative for genotoxicity in the following assays: Ames test for bacterial gene mutation, in vitro chromosomal aberration assay in Chinese hamster ovary cells, and in vivo mouse micronucleus test.
Ivacaftor impaired fertility and reproductive performance indices in male and female rats at 200 mg/kg/day (yielding exposures approximately 8 and 5 times, respectively, the MRHD based on summed AUCs of ivacaftor and its major metabolites). Increases in prolonged diestrus were observed in females at 200 mg/kg/day. Ivacaftor also increased the number of females with all nonviable embryos and decreased corpora lutea, implantations, and viable embryos in rats at 200 mg/kg/day (approximately 5 times the MRHD based on summed AUCs of ivacaftor and its major metabolites) when dams were dosed prior to and during early pregnancy. These impairments of fertility and reproductive performance in male and female rats at 200 mg/kg/day were attributed to severe toxicity. No effects on male or female fertility and reproductive performance indices were observed at ≤100 mg/kg/day (yielding exposures approximately 6 and 3 times, respectively, the MRHD based on summed AUCs of ivacaftor and its major metabolites).
14. Clinical Studies
14.1 Trials in Patients with CF who have a G551D Mutation in the CFTR Gene
Dose Ranging:
Dose ranging for the clinical program consisted primarily of one double-blind, placebo-controlled, crossover trial in 39 adult (mean age 31 years) Caucasian patients with CF who had FEV1 ≥40% predicted. Twenty patients with median predicted FEV1 at baseline of 56% (range: 42% to 109%) received KALYDECO 25, 75, 150 mg, or placebo every 12 hours for 14 days and 19 patients with median predicted FEV1 at baseline of 69% (range: 40% to 122%) received KALYDECO 150, 250 mg, or placebo every 12 hours for 28 days. The selection of the 150 mg every 12 hours dose was primarily based on nominal improvements in lung function (pre-dose FEV1) and changes in pharmacodynamic parameters (sweat chloride and nasal potential difference). The twice-daily dosing regimen was primarily based on an apparent terminal plasma half-life of approximately 12 hours.
Efficacy:
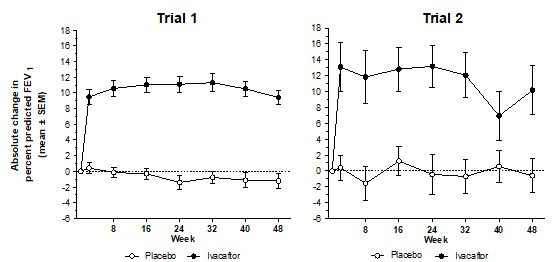
The efficacy of KALYDECO in patients with CF who have a G551D mutation in the CFTR gene was evaluated in two randomized, double-blind, placebo-controlled clinical trials in 213 clinically stable patients with CF (109 receiving KALYDECO 150 mg twice daily). All eligible patients from these trials were rolled over into an open-label extension study.
Trial 1 evaluated 161 patients with CF who were 12 years of age or older (mean age 26 years) with FEV1 at screening between 40-90% predicted [mean FEV1 64% predicted at baseline (range: 32% to 98%)]. Trial 2 evaluated 52 patients who were 6 to 11 years of age (mean age 9 years) with FEV1 at screening between 40-105% predicted [mean FEV1 84% predicted at baseline (range: 44% to 134%)]. Patients who had persistent Burkholderia cenocepacia, Burkholderia dolosa, or Mycobacterium abscessus isolated from sputum at screening and those with abnormal liver function defined as 3 or more liver function tests (ALT, AST, AP, GGT, total bilirubin) ≥3 times the ULN were excluded.
Patients in both trials were randomized 1:1 to receive either 150 mg of KALYDECO or placebo every 12 hours with fat-containing food for 48 weeks in addition to their prescribed CF therapies (e.g., tobramycin, dornase alfa). The use of inhaled hypertonic saline was not permitted.
The primary efficacy endpoint in both studies was improvement in lung function as determined by the mean absolute change from baseline in percent predicted pre-dose FEV1 through 24 weeks of treatment.
In both studies, treatment with KALYDECO resulted in a significant improvement in FEV1. The treatment difference between KALYDECO and placebo for the mean absolute change in percent predicted FEV1 from baseline through Week 24 was 10.6 percentage points (P<0.0001) in Trial 1 and 12.5 percentage points (P<0.0001) in Trial 2 (Figure 4). These changes persisted through 48 weeks. Improvements in percent predicted FEV1 were observed regardless of age, disease severity, sex, and geographic region.
| Figure 4: Mean Absolute Change from Baseline in Percent Predicted FEV1 * |
|---|
|
|
|
Other efficacy variables included absolute change from baseline in sweat chloride [see Clinical Pharmacology (12.2)], time to first pulmonary exacerbation (Trial 1 only), absolute change from baseline in weight, and improvement from baseline in Cystic Fibrosis Questionnaire Revised (CFQ-R) respiratory domain score, a measure of respiratory symptoms relevant to patients with CF such as cough, sputum production, and difficulty breathing. For the purpose of the study, a pulmonary exacerbation was defined as a change in antibiotic therapy (IV, inhaled, or oral) as a result of 4 or more of 12 pre-specified sino-pulmonary signs/symptoms. Patients treated with KALYDECO demonstrated statistically significant improvements in risk of pulmonary exacerbations, CF symptoms (in Trial 1 only), and gain in body weight (Table 5). Weight data, when expressed as body mass index normalized for age and sex in patients <20 years of age, were consistent with absolute change from baseline in weight.
| Trial 1 | Trial 2 | |||
|---|---|---|---|---|
| Endpoint | Treatment difference *
(95% CI) | P value | Treatment difference *
(95% CI) | P value |
| CI: confidence interval; NA: not analyzed due to low incidence of events. | ||||
| Mean absolute change from baseline in CFQ-R respiratory domain score (points) | ||||
| Through Week 24 | 8.1 (4.7, 11.4) | <0.0001 | 6.1 (-1.4, 13.5) | 0.1092 |
| Through Week 48 | 8.6 (5.3, 11.9) | <0.0001 | 5.1 (-1.6, 11.8) | 0.1354 |
| Relative risk of pulmonary exacerbation | ||||
| Through Week 24 | 0.40 † | 0.0016 | NA | NA |
| Through Week 48 | 0.46 † | 0.0012 | NA | NA |
| Mean absolute change from baseline in body weight (kg) | ||||
| At Week 24 | 2.8 (1.8, 3.7) | <0.0001 | 1.9 (0.9, 2.9) | 0.0004 |
| At Week 48 | 2.7 (1.3, 4.1) | 0.0001 | 2.8 (1.3, 4.2) | 0.0002 |
| Absolute change in sweat chloride (mmol/L) | ||||
| Through Week 24 | -48 (-51, -45) | <0.0001 | -54 (-62, -47) | <0.0001 |
| Through Week 48 | -48 (-51, -45) | <0.0001 | -53 (-61, -46) | <0.0001 |
14.2 Trial in Patients with a G1244E, G1349D, G178R, G551S, G970R, S1251N, S1255P, S549N, or S549R Mutation in the CFTR Gene
The efficacy and safety of KALYDECO in patients with CF who have a G1244E, G1349D, G178R, G551S, G970R, S1251N, S1255P, S549N, or S549R mutation in the CFTR gene were evaluated in a two-part, randomized, double-blind, placebo-controlled, crossover design clinical trial in 39 patients with CF (Trial 4). Patients who completed Part 1 of this trial continued into the 16-week open-label Part 2 of the study. The mutations studied were G178R, S549N, S549R, G551S, G970R, G1244E, S1251N, S1255P, and G1349D. See Clinical Studies (14.1) for efficacy in patients with a G551D mutation.
Patients were 6 years of age or older (mean age 23 years) with FEV1 ≥40% at screening [mean FEV1 at baseline 78% predicted (range: 43% to 119%)]. Patients with evidence of colonization with Burkholderia cenocepacia, Burkholderia dolosa, or Mycobacterium abscessus and those with abnormal liver function defined as 3 or more liver function tests (ALT, AST, AP, GGT, total bilirubin) ≥3 times the ULN at screening were excluded.
Patients were randomized 1:1 to receive either 150 mg of KALYDECO or placebo every 12 hours with fat-containing food for 8 weeks in addition to their prescribed CF therapies during the first treatment period and crossed over to the other treatment for the second 8 weeks. The two 8-week treatment periods were separated by a 4- to 8-week washout period. The use of inhaled hypertonic saline was not permitted.
The primary efficacy endpoint was improvement in lung function as determined by the mean absolute change from baseline in percent predicted FEV1 through 8 weeks of treatment. Other efficacy variables included absolute change from baseline in sweat chloride through 8 weeks of treatment [see Clinical Pharmacology (12.2)], absolute change from baseline in body mass index (BMI) at 8 weeks of treatment (including body weight at 8 weeks), and improvement in CFQ-R respiratory domain score through 8 weeks of treatment. For the overall population of the 9 mutations studied, treatment with KALYDECO compared to placebo resulted in significant improvement in percent predicted FEV1 [10.7 through Week 8 (P<0.0001)], BMI [0.66 kg/m2 at Week 8 (P<0.0001)], and CFQ-R respiratory domain score [9.6 through Week 8 (P=0.0004)]; however, there was a high degree of variability of efficacy responses among the 9 mutations (Table 6).
| Mutation (n) | Absolute change in percent predicted FEV1 | BMI (kg/m2) | CFQ-R Respiratory Domain Score (Points) | Absolute Change in Sweat Chloride (mmol/L) |
||
|---|---|---|---|---|---|---|
| At Week 2 | At Week 4 | At Week 8 | At Week 8 | At Week 8 | At Week 8 | |
|
||||||
| All patients (n=39) Results shown as mean (95% CI) change from baseline KALYDECO vs. placebo-treated patients: |
||||||
| 8.3 (4.5, 12.1) | 10.0 (6.2, 13.8) | 13.8 (9.9, 17.6) | 0.66 * (0.34, 0.99) | 12.8 (6.7, 18.9) | -50 (-58, -41) † | |
| Patients grouped under mutation types (n)
Results shown as mean (minimum, maximum) for change from baseline for KALYDECO-treated patients ‡: |
||||||
| G1244E (5) | 11 (-5, 25) | 6 (-5, 13) | 8 (-1, 18) | 0.63 (0.34, 1.32) | 3.3 (-27.8, 22.2) | -55 (-75, -34) |
| G1349D (2) | 19 (5, 33) | 18 (2, 35) | 20 (3, 36) | 1.15 (1.07, 1.22) | 16.7 (-11.1, 44.4) | -80 (-82, -79) |
| G178R (5) | 7 (1, 17) | 10 (-2, 21) | 8 (-1, 18) | 0.85 (0.33, 1.46) | 20.0 (5.6, 50.0) | -53 (-65, -35) |
| G551S (2) | 0 (-5, 5) | 0.3 (-5, 6) | 3 § | 0.16 § | 16.7 § | -68 § |
| G970R (4) | 7 (1, 13) | 7 (1, 14) | 3 (-1, 5) | 0.48 (-0.38, 1.75) | 1.4 (-16.7, 16.7) | -6 (-16, -2) |
| S1251N (8) | 2 (-23, 20) | 8 (-13, 26) | 9 (-20, 21) | 0.73 (0.08, 1.83) | 23.3 (5.6, 50.0) | -54 (-84, -7) |
| S1255P (2) | 11 (8, 14) | 9 (5, 13) | 3 (-1, 8) | 1.62 (1.39, 1.84) | 8.3 (5.6, 11.1) | -78 (-82, -74) |
| S549N (6) | 11 (5, 16) | 8 (-9, 19) | 11 (-2, 20) | 0.79 (0.00, 1.91) | 8.8 (-8.3, 27.8) | -74 (-93, -53) |
| S549R (4) | 3 (-4, 8) | 4 (-4, 10) | 5 (-3, 13) | 0.53 (0.33, 0.80) | 6.9 (0.0, 11.1) | -61 ¶ (-71, -54) |
14.3 Trial in Patients with CF who have an R117H Mutation in the CFTR Gene
The efficacy and safety of KALYDECO in patients with CF who have an R117H mutation in the CFTR gene were evaluated in a randomized, double-blind, placebo-controlled, parallel-group clinical trial (Trial 5). Fifty-nine of 69 patients completed 24 weeks of treatment. Two patients discontinued and 8 patients did not complete treatment due to study termination. Trial 5 evaluated 69 clinically stable patients with CF who were 6 years of age or older (mean age 31 years). Patients who were 12 years and older had FEV1 at screening between 40-90% predicted, and patients who were 6-11 years of age had FEV1 at screening between 40-105% predicted. The overall mean FEV1 was 73% predicted at baseline (range: 33% to 106%). The patients had well preserved BMIs (mean overall: 23.76 kg/m2) and a high proportion were pancreatic sufficient as assessed by a low rate of pancreatic enzyme replacement therapy use (pancreatin: 11.6%; pancrelipase: 5.8%). Patients who had persistent Burkholderia cenocepacia, Burkholderia dolosa, or Mycobacterium abscessus isolated from sputum at screening, and those with abnormal liver function defined as 3 or more liver function tests (ALT, AST, AP, GGT, total bilirubin) ≥3 times the ULN, were excluded.
Patients were randomized 1:1 to receive either 150 mg of KALYDECO (n=34) or placebo (n=35) every 12 hours with fat-containing food for 24 weeks in addition to their prescribed CF therapies.
The primary efficacy endpoint was improvement in lung function as determined by the mean absolute change from baseline in percent predicted FEV1 through 24 weeks of treatment. The treatment difference for absolute change in percent predicted FEV1 through Week 24 was 2.1 percentage points (analysis conducted with the full analysis set which included all 69 patients) and did not reach statistical significance (Table 7).
Other efficacy variables that were analyzed included absolute change in sweat chloride from baseline through Week 24, improvement in cystic fibrosis respiratory symptoms through Week 24 as assessed by the CFQ-R respiratory domain score (Table 7), absolute change in body mass index (BMI) at Week 24, and time to first pulmonary exacerbation. The overall treatment difference for the absolute change from baseline in BMI at Week 24 was 0.3 kg/m2 and the calculated hazard ratio for time to first pulmonary exacerbation was 0.93, which were not statistically significant.
Statistically significant improvements in clinical efficacy (FEV1, CFQ-R respiratory domain score) were seen in several subgroup analyses and decreases in sweat chloride were observed in all subgroups. The mean baseline sweat chloride for all patients was 70 mmol/L. Subgroups analyzed included those based on age, lung function, and poly-T status (Table 7).
| Absolute Change through Week 24 *- All Randomized Patients | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % Predicted FEV1
(Percentage Points) | CFQ-R Respiratory Domain Score (Points) | Sweat Chloride (mmol/L) |
||||||||
| Subgroup Parameter | Study Drug | n | Mean | Treatment Difference (95% CI) | n | Mean | Treatment Difference (95% CI) | n | Mean | Treatment Difference (95% CI) |
| R117H–All Patients | ||||||||||
| Placebo KALYDECO | 35 34 | 0.5 2.6 | 2.1 (-1.1, 5.4) | 34 33 | -0.8 7.6 | 8.4 (2.2, 14.6) | 35 32 | -2.3 -26.3 | -24.0 (-28.0, -19.9) |
|
| Subgroup by Age | ||||||||||
| 6-11 | Placebo KALYDECO | 8 9 | 3.5 -2.8 | -6.3 (-12.0, -0.7) | 7 8 | -1.6 -7.7 | -6.1 (-15.7, 3.4) | 8 8 | 1.0 -26.6 | -27.6 (-37.2, -18.1) |
| 12-17 | Placebo KALYDECO | 1 1 | --- | --- | 1 1 | --- | --- | 1 1 | --- | --- |
| ≥18 | Placebo KALYDECO | 26 24 | -0.5 4.5 | 5.0 (1.1, 8.8) | 26 24 | -0.5 12.2 | 12.6 (5.0, 20.3) | 26 23 | -4.0 -25.9 | -21.9 (-26.5, -17.3) |
| Subgroup by Poly-T Status † | ||||||||||
| 5T | Placebo KALYDECO | 24 14 | 0.7 6.0 | 5.3 (1.3, 9.3) | 24 14 | -0.6 14.7 | 15.3 (7.7, 23.0) | 24 13 | -4.6 -28.7 | -24.2 (-30.2, -18.2) |
| 7T | Placebo KALYDECO | 5 11 | -0.9 -0.7 | 0.2 (-8.1, 8.5) | 5 11 | -6.0 -0.7 | 5.2 (-13.0, 23.4) | 5 10 | 3.9 -20.2 | -24.1 (-33.9, -14.3) |
| Subgroup by Baseline FEV1 % Predicted | ||||||||||
| <70% | Placebo KALYDECO | 15 13 | 0.4 4.5 | 4.0 (-2.1, 10.1) | 15 13 | 3.0 14.4 | 11.4 (1.2, 21.6) | 15 12 | -3.8 -29.3 | -25.5 (-31.8, -19.3) |
| 70-90% | Placebo KALYDECO | 14 14 | 0.2 2.8 | 2.6 (-2.3, 7.5) | 13 14 | -3.6 5.2 | 8.8 (-2.6, 20.2) | 14 14 | -3.1 -23.0 | -20.0 (-26.9, -12.9) |
| >90% | Placebo KALYDECO | 6 7 | 2.2 -2.1 | -4.3 (-9.9, 1.3) | 6 6 | -2.5 -3.2 | -0.7 (-10.4, 9.0) | 6 6 | 1.0 -25.9 | -26.8 (-39.5, -14.1) |
14.4 Trial in Patients with CF Heterozygous for the F508del Mutation and a Second Mutation Predicted to be Responsive to ivacaftor
The efficacy and safety of KALYDECO and an ivacaftor-containing combination product in 246 patients with CF was evaluated in a randomized, double-blind, placebo-controlled, 2-period, 3-treatment, 8-week crossover design clinical trial (Trial 7). Mutations predicted to be responsive to ivacaftor were selected for the study based on the clinical phenotype (pancreatic sufficiency), biomarker data (sweat chloride), and in vitro responsiveness to ivacaftor.
Eligible patients were heterozygous for the F508del mutation with a second mutation predicted to be responsive to ivacaftor. Of the 244 patients included in the efficacy analysis, who were randomized and dosed, 146 patients had a splice mutation and 98 patients had a missense mutation, as the second allele. 156 patients received KALYDECO and 161 patients received placebo. Patients were aged 12 years and older (mean age 35 years [range 12-72]) and had a percent predicted FEV1 at screening between 40-90 [mean ppFEV1 at study baseline 62 (range: 35 to 94)]. Patients with evidence of colonization with organisms associated with a more rapid decline in pulmonary status (e.g., Burkholderia cenocepacia, Burkholderia dolosa, or Mycobacterium abscessus) and those with abnormal liver function at screening were excluded. Abnormal liver function was defined as 2 or more liver function tests (ALT, AST, ALP, GGT) ≥3 times the ULN or total bilirubin ≥2 times the ULN, or a single increase in ALT/AST ≥5 times the ULN.
The primary efficacy endpoint was the mean absolute change from study baseline in percent predicted FEV1 averaged at Weeks 4 and 8 of treatment. The key secondary efficacy endpoint was absolute change in CFQ-R respiratory domain score from study baseline averaged at Weeks 4 and 8 of treatment. For the overall population, treatment with KALYDECO compared to placebo resulted in significant improvement in ppFEV1 [4.7 percent points from study baseline to average of Week 4 and Week 8 (P<0.0001)] and CFQ-R respiratory domain score [9.7 points from study baseline to average of Week 4 and Week 8 (P<0.0001)]. Statistically significant improvements compared to placebo were also observed in the subgroup of patients with splice mutations and missense mutations (Table 8).
| Mutation (n) | Absolute Change in percent predicted FEV1 *† | Absolute Change in CFQ-R Respiratory Domain Score (Points) *‡ | Absolute Change in Sweat Chloride (mmol/L) *‡ |
|---|---|---|---|
| Splice mutations (n=94 for IVA and n=97 for PBO) Results shown as difference in mean (95% CI) change from study baseline for KALYDECO vs. placebo-treated patients: |
|||
| 5.4 (4.1, 6.8) | 8.5 (5.3, 11.7) | -2.4 (-5.0, 0.3) |
|
| By individual splice mutation (n). Results shown as mean (minimum, maximum) for change from study baseline for KALYDECO-treated patients | |||
| 2789+5G→A (28) | 5.1 (-7.1, 17.0) | 8.6 (-5.6, 27.8) | 0.4 (-7.5, 8.8) |
| 3272-26A→G (23) | 3.5 (-9.1, 16.0) | 8.0 (-11.1, 27.8) | -2.3 (-25.0, 11.8) |
| 3849+10kbC→T (40) | 5.1 (-6.8, 16.2) | 7.5 (-30.6, 55.6) | -4.6 (-80.5, 23.0) |
| 711+3A→G (2) | 9.2 (8.9, 9.6) | -8.3 (-13.9, -2.8) | -9.9 (-13.5, -6.3) |
| E831X (1) | 7.1 (7.1, 7.1) | 0.0 (0.0, 0.0) | -7.8 (-7.8, -7.8) |
| Missense mutations (n=62 for IVA and n=63 for PBO) Results shown as difference in mean (95% CI) change from study baseline for KALYDECO vs. placebo-treated patients: |
|||
| 3.6 (1.9, 5.2) | 11.5 (7.5, 15.4) | -7.8 (-11.2, -4.5) |
|
| By individual missense mutation (n). Results shown as mean (minimum, maximum) for change from study baseline for KALYDECO-treated patients | |||
| D579G (2) | 13.3 (12.4, 14.1) | 15.3 (-2.8, 33.3) | -30.8 (-36.0, -25.5) |
| D1152H (15) | 2.4 (-5.0, 10.2) | 13.7 (-16.7, 50.0) | -4.8 (-22.0, 3.0) |
| A455E (14) | 3.7 (-6.6, 19.7) | 6.8 (-13.9, 33.3) | 7.5 (-16.8, 16.0) |
| L206W (2) | 4.2 (2.5, 5.9) | 12.5 (-5.6, 30.6) | 3.9 (-8.3, 16.0) |
| P67L (12) | 4.3 (-2.5, 25.7) | 10.8 (-12.5, 36.1) | -10.5 (-34.8, 9.8) |
| R1070W (1) | 2.9 (2.9, 2.9) | 44.4 (44.4, 44.4) | 0.3 (0.3, 0.3) |
| R117C (1) | 3.5 (3.5, 3.5) | 22.2 (22.2, 22.2) | -36.0 (-36.0, -36.0) |
| R347H (3) | 2.5 (-0.6, 6.9) | 6.5 (5.6, 8.3) | -19.2 (-25.8, -7.0) |
| R352Q (2) | 4.4 (3.5, 5.3) | 9.7 (8.3, 11.1) | -21.9 (-45.5, 1.8) |
| S945L (9) | 8.8 (-0.2, 20.5) | 10.6 (-25.0, 27.8) | -30.8 (-50.8, -17.3) |
| S977F (1) | 4.3 (4.3, 4.3) | -2.8 (-2.8, -2.8) | -19.5 (-19.5, -19.5) |
In an analysis of BMI at Week 8, an exploratory endpoint, patients treated with KALYDECO had a mean improvement of 0.28 kg/m2 [95% CI (0.14, 0.43)], 0.24 kg/m2 [95% CI (0.06, 0.43)], and 0.35 kg/m2 [95% CI (0.12, 0.58)] versus placebo for the overall, splice, and missense mutation populations of patients, respectively.
14.5 Trial in Patients Homozygous for the F508del Mutation in the CFTR Gene
Trial 3 was a 16-week, randomized, double-blind, placebo-controlled, parallel-group trial in 140 patients with CF age 12 years and older who were homozygous for the F508del mutation in the CFTR gene and who had FEV1 ≥40% predicted. Patients were randomized 4:1 to receive KALYDECO 150 mg (n=112) every 12 hours or placebo (n=28) in addition to their prescribed CF therapies. The mean age of patients enrolled was 23 years and the mean baseline FEV1 was 79% predicted (range 40% to 129%). As in Trials 1 and 2, patients who had persistent Burkholderia cenocepacia, Burkholderia dolosa, or Mycobacterium abscessus isolated from sputum at screening and those with abnormal liver function defined as 3 or more liver function tests (ALT, AST, AP, GGT, total bilirubin) ≥3 times the ULN were excluded. The use of inhaled hypertonic saline was not permitted.
The primary endpoint was improvement in lung function as determined by the mean absolute change from baseline through Week 16 in percent predicted FEV1. The treatment difference from placebo for the mean absolute change in percent predicted FEV1 through Week 16 in patients with CF homozygous for the F508del mutation in the CFTR gene was 1.72 percentage points (1.5% and -0.2% for patients in the KALYDECO and placebo-treated groups, respectively) and did not reach statistical significance (Table 9).
Other efficacy variables that were analyzed included absolute change in sweat chloride from baseline through Week 16, change in cystic fibrosis respiratory symptoms through Week 16 as assessed by the CFQ-R respiratory domain score (Table 9), change in weight through Week 16, and rate of pulmonary exacerbation. The overall treatment difference for change from baseline in weight through Week 16 was -0.16 kg (95% CI -1.06, 0.74); the rate ratio for pulmonary exacerbation was 0.677 (95% CI 0.33, 1.37).
| Absolute Change through Week 16 *- Full Analysis Set | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % Predicted FEV1
(Percentage Points) | CFQ-R Respiratory Domain Score (Points) | Sweat Chloride (mmol/L) |
||||||||
| Subgroup Parameter | Study Drug | n | Mean | Treatment Difference (95% CI) | n | Mean | Treatment Difference (95% CI) | n | Mean | Treatment Difference (95% CI) |
|
||||||||||
| F508del homozygous | ||||||||||
| Placebo KALYDECO | 28 111 | -0.2 1.5 | 1.72 (-0.6, 4.1) | 28 111 | -1.44 -0.12 | 1.3 (-2.9, 5.6) | 28 109 | 0.13 -2.74 | -2.9 (-5.6, -0.2) |
|
16. How is Kalydeco supplied
KALYDECO (ivacaftor) tablets are supplied as light blue, film-coated, capsule-shaped tablets containing 150 mg of ivacaftor. Each tablet is printed with the characters "V 150" on one side and plain on the other, and is packaged as follows:
| 56-count carton (contains 4 individual blister cards of 14 tablets per card) | NDC 51167-200-01 | |
| 60-count bottle | NDC 51167-200-02 |
KALYDECO (ivacaftor) oral granules are supplied as small, white to off-white granules and enclosed in unit-dose packets as follows:
| 56-count carton (contains 56 unit-dose packets of 5.8 mg ivacaftor per packet) | NDC 51167-785-01 | |
| 56-count carton (contains 56 unit-dose packets of 13.4 mg ivacaftor per packet) | NDC 51167-770-01 | |
| 56-count carton (contains 56 unit-dose packets of 25 mg ivacaftor per packet) | NDC 51167-600-01 | |
| 56-count carton (contains 56 unit-dose packets of 50 mg ivacaftor per packet) | NDC 51167-300-01 | |
| 56-count carton (contains 56 unit-dose packets of 75 mg ivacaftor per packet) | NDC 51167-400-01 |
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Transaminase (ALT or AST) Elevations and Monitoring
Inform patients that elevation in liver tests have occurred in patients treated with KALYDECO. Liver function tests will be performed prior to initiating KALYDECO, every 3 months during the first year of treatment and annually thereafter. More frequent monitoring of liver function tests should be considered in patients with a history of transaminase elevations [see Warnings and Precautions (5.1)].
Hypersensitivity Reactions, Including Anaphylaxis
Hypersensitivity reactions including anaphylaxis are possible with use of KALYDECO. Inform patients of the early signs of hypersensitivity reactions including rash, hives, itching, facial swelling, tightness of the chest and wheezing. Advise patients to discontinue use of KALYDECO immediately and contact their physician or go to the emergency department if these symptoms occur.
Drug Interactions with CYP3A Inducers and Inhibitors
Ask patients to tell you all the medications they are taking including any herbal supplements or vitamins. Co-administration of KALYDECO with strong CYP3A inducers (e.g., rifampin, St. John's wort) is not recommended, as they may reduce the therapeutic effectiveness of KALYDECO. Dose reduction is recommended when patients aged 6 months and older are taking concomitant strong CYP3A inhibitors, such as ketoconazole, or moderate CYP3A inhibitors, such as fluconazole [see Dosage and Administration (2.4), Drug Interactions (7.1)]. Treatment with KALYDECO is not recommended in patients aged 1 month to less than 6 months who are taking concomitant moderate or strong CYP3A inhibitors. Food or drink containing grapefruit should be avoided [see Drug Interactions (7.1, 7.2) and Clinical Pharmacology (12.3)].
Use in Patients with Hepatic Impairment
Inquire and/or assess whether patients have liver impairment. Reduce the dose of KALYDECO in patients aged 6 months and older with moderately impaired hepatic function (Child-Pugh Class B, score 7-9) to one tablet or one packet of granules once daily. KALYDECO has not been studied in patients with severe hepatic impairment (Child-Pugh Class C, score 10-15); however, exposure is expected to be substantially higher than that observed in patients with moderate hepatic impairment. When benefits are expected to outweigh the risks, KALYDECO should be used with caution in patients aged 6 months and older with severe hepatic impairment at a reduced dose [see Dosage and Administration (2.3)]. Treatment with KALYDECO is not recommended in patients aged 1 month to less than 6 months with any signs of hepatic impairment. No dose adjustment is recommended for patients 6 months and older with mild hepatic impairment (Child-Pugh Class A, score 5-6) [see Use in Specific Populations (8.6)].
Driving and Operating Machinery
Dizziness has been reported in patients receiving KALYDECO, which could influence the ability to drive or operate machines [see Adverse Reactions (6.1)]. Advise patients not to drive or operate machines if they experience dizziness until symptoms abate.
Administration
KALYDECO (ivacaftor) tablets 150 mg
Inform patients that KALYDECO tablet is best absorbed by the body when taken with food that contains fat. A typical CF diet will satisfy this requirement. Examples include eggs, butter, peanut butter, cheese pizza, whole-milk dairy products (such as whole milk, cheese, and yogurt), etc.
KALYDECO (ivacaftor) oral granules 5.8 mg, 13.4 mg, 25 mg, 50 mg, or 75 mg
Inform patients and caregivers that KALYDECO oral granules should be mixed with one teaspoon (5 mL) of age-appropriate soft food or liquid and completely consumed to ensure delivery of the entire dose. Food or liquid should be at or below room temperature. Once mixed, the product has been shown to be stable for one hour, and therefore should be consumed during this period. Some examples of appropriate soft foods or liquids may include puréed fruits or vegetables, yogurt, applesauce, water, breast milk, infant formula, milk, or juice.
Inform patients and caregivers that KALYDECO is best absorbed by the body when taken with food that contains fat; therefore, KALYDECO oral granules should be taken just before or just after consuming food that contains fat. A typical CF diet will satisfy this requirement. Examples include eggs, butter, peanut butter, cheese pizza, whole-milk dairy products (such as whole milk, cheese, yogurt, breast milk, and infant formula), etc.
Patients should be informed about what to do in the event they miss a dose of KALYDECO:
- In case a dose of KALYDECO is missed within 6 hours of the time it is usually taken, patients should be instructed to take the prescribed dose of KALYDECO with fat-containing food as soon as possible.
- If more than 6 hours have passed since KALYDECO is usually taken, the missed dose should NOT be taken, and the patient should resume the usual dosing schedule.
- Patients should be advised to contact their healthcare provider if they have questions.
Cataracts
Inform patients that abnormality of the eye lens (cataract) has been noted in some children and adolescents receiving KALYDECO. Baseline and follow-up ophthalmological examinations should be performed in pediatric patients initiating KALYDECO treatment [see Warnings and Precautions (5.4)].
Manufactured for
Vertex Pharmaceuticals Incorporated
50 Northern Avenue
Boston, MA 02210
KALYDECO, VERTEX, and the VERTEX triangle logo are registered trademarks of Vertex Pharmaceuticals Incorporated.
All other trademarks referenced herein are the property of their respective owners.
©2023 Vertex Pharmaceuticals Incorporated
ALL RIGHTS RESERVED
| This Patient Information has been approved by the U.S. Food and Drug Administration. | Revised: 08/2023 | ||
| Patient Information KALYDECO® (kuh-LYE-deh-koh) (ivacaftor) tablets, for oral use (ivacaftor) oral granules |
|||
What is KALYDECO?
|
|||
Before taking KALYDECO, tell your doctor about all of your medical conditions, including if you:
KALYDECO may affect the way other medicines work, and other medicines may affect how KALYDECO works. Ask your doctor or pharmacist for a list of these medicines if you are not sure. Especially tell your doctor if you take:
|
|||
How should I take KALYDECO?
|
|||
What should I avoid while taking KALYDECO?
|
|||
| What are the possible side effects of KALYDECO? KALYDECO can cause serious side effects, including:
|
|||
| The most common side effects of KALYDECO include: | |||
|
|
||
| Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of KALYDECO. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
|||
How should I store KALYDECO?
|
|||
| General information about the safe and effective use of KALYDECO.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use KALYDECO for a condition for which it was not prescribed. Do not give KALYDECO to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or doctor for information about KALYDECO that is written for health professionals. |
|||
| What are the ingredients in KALYDECO? Ivacaftor tablets: Active ingredients: ivacaftor. Inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hypromellose acetate succinate, lactose monohydrate, magnesium stearate, microcrystalline cellulose, and sodium lauryl sulfate. The tablet film coat contains: carnauba wax, FD&C Blue #2, PEG 3350, polyvinyl alcohol, talc, and titanium dioxide. The printing ink contains: ammonium hydroxide, iron oxide black, propylene glycol, and shellac. Ivacaftor oral granules: Active ingredients: ivacaftor. Inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hypromellose acetate succinate, lactose monohydrate, magnesium stearate, mannitol, sucralose, and sodium lauryl sulfate. Manufactured for: Vertex Pharmaceuticals Incorporated, 50 Northern Avenue, Boston, MA 02210 KALYDECO, VERTEX, and the VERTEX triangle logo are registered trademarks of Vertex Pharmaceuticals Incorporated. All other trademarks referenced herein are the property of their respective owners. ©2023 Vertex Pharmaceuticals Incorporated For more information, go to www.kalydeco.com or call 1-877-752-5933. |
|||
PRINCIPAL DISPLAY PANEL - 150 mg Tablet Blister Card Carton
NDC 51167-200-01
Rx only
kalydeco®
(ivacaftor) tablets
150 mg per tablet
Carton contains
4 individual blister cards
of 14 tablets per card.
56 tablets
PRINCIPAL DISPLAY PANEL - 150 mg Tablet Bottle Carton
NDC 51167-200-02
Rx only
kalydeco™
(ivacaftor) tablets
150 mg
60 tablets
PRINCIPAL DISPLAY PANEL - 50 mg Granule Packet Carton
Rx only
NDC 51167-300-01
kalydeco®
(ivacaftor) oral granules
50 mg
56 packets
Each packet contains 50 mg ivacaftor
Carton contains: 4 individual wallets
with 14 packets per wallet
Lift here to open
PRINCIPAL DISPLAY PANEL - 75 mg Granule Packet Carton
Rx only
NDC 51167-400-01
kalydeco®
(ivacaftor) oral granules
75 mg
56 packets
Each packet contains 75 mg ivacaftor
Carton contains: 4 individual wallets
with 14 packets per wallet
Lift here to open
PRINCIPAL DISPLAY PANEL - 25 mg Granule Packet Carton
Rx only
NDC 51167-600-01
kalydeco®
(ivacaftor) oral granules
25 mg
56 packets
Each packet contains 25 mg ivacaftor
Carton contains: 4 individual wallets
wtih 14 packets per wallet
Lift here to open
| KALYDECO
ivacaftor tablet, film coated |
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
| KALYDECO
ivacaftor granule |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| KALYDECO
ivacaftor granule |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| KALYDECO
ivacaftor granule |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| KALYDECO
ivacaftor granule |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| KALYDECO
ivacaftor granule |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Vertex Pharmaceuticals Incorporated (602478257) |
Frequently asked questions
- How does Kalydeco work?
- What is the difference between Symdeko and Orkambi?
- What is the difference between Symdeko and Kalydeco?
- What is an orphan drug?
More about Kalydeco (ivacaftor)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: CFTR potentiators
- Breastfeeding