Simeprevir
Medically reviewed by Drugs.com. Last updated on Feb 8, 2024.
Pronunciation
(sim E pre vir)
Index Terms
- Simeprevir Sodium
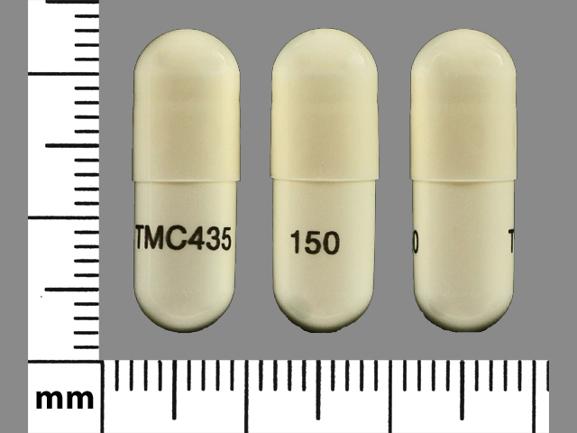
- TMC435
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Olysio: 150 mg [DSC]
Brand Names: U.S.
- Olysio [DSC]
Pharmacologic Category
- Antihepaciviral, NS3/4A Protease Inhibitor (Anti-HCV)
- NS3/4A Inhibitor
Pharmacology
Simeprevir is an inhibitor of HCV NS3/4A protease, a protease that is essential for viral replication. It is considered a direct-acting antiviral treatment for HCV, also called a specifically targeted antiviral therapy for HCV (STAT-C).
Absorption
Food enhances absorption.
Metabolism
Primarily oxidative metabolism by CYP3A4 (and possibly CYP2C8 and CYP2C19) to unchanged drug and metabolites (minor).
Excretion
Feces (~91%); urine (<1%)
Time to Peak
Serum: 4 to 6 hours
Half-Life Elimination
Plasma: 10 to 13 hours (healthy volunteers); 41 hours (HCV-infected patients)
Protein Binding
>99.9% (albumin and alpha 1-acid glycoprotein)
Special Populations: Hepatic Function Impairment
Mean steady-state AUC of simeprevir was 2.4-fold higher in HCV-uninfected subjects with moderate hepatic impairment (Child-Pugh class B) and 5.2-fold higher in HCV-uninfected subjects with severe hepatic impairment (Child-Pugh class C) compared with HCV-uninfected subjects with normal hepatic function.
Use: Labeled Indications
Chronic hepatitis C: Treatment of genotype 1 chronic hepatitis C in combination with sofosbuvir in adults without cirrhosis
Limitations of use: Not recommended for use in patients who have previously failed a simeprevir-containing regimen or another regimen containing HCV protease inhibitors.
Off Label Uses
Chronic hepatitis C, genotype 1 and 4 (post-liver transplantation)
Based on the AASLD/IDSA Recommendations for Testing, Managing, and Treating Hepatitis C guidelines, simeprevir, in combination with sofosbuvir (with or without ribavirin), is an effective and recommended alternative regimen for the treatment of chronic hepatitis C virus genotype 1 or 4 in liver transplant recipients (treatment-naive and -experienced) without cirrhosis or with compensated cirrhosis. Hepatitis C treatment guidelines are constantly changing with the advent of new treatment therapies and information; consult current clinical practice guidelines for the most recent treatment recommendations.
Contraindications
There are no contraindications listed in the manufacturer's labeling. When administered with ribavirin and peginterferon alfa, the contraindications to ribavirin and peginterferon alfa also apply. See Ribavirin and Peginterferon Alfa monographs.
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to simeprevir or any component of the formulation
Dosing: Adult
Note: Olysio tablets have been discontinued in the US for more than 1 year.
Note: If other concomitant treatment (sofosbuvir or peginterferon and ribavirin) is discontinued for any reason, simeprevir must also be discontinued. Do not reduce simeprevir dosage or interrupt therapy; if therapy must be interrupted due to adverse reactions or inadequate response, do not reinitiate. In patients with genotype 1a and compensated cirrhosis, screening for HCV with the NS3 Q80K polymorphism may be considered prior to starting therapy. Screening is strongly recommended prior to initiation of combination treatment with peginterferon alfa and ribavirin in patients with genotype 1a; consider alternative therapy in patients infected with HCV genotype 1a containing the Q80K polymorphism.
Chronic hepatitis C (CHC): Oral:
Genotype 1, treatment-naive or peginterferon + ribavirin treatment-experienced without cirrhosis (alternative regimen): 150 mg once daily in combination with sofosbuvir for 12 weeks (AASLD/IDSA 2018).
Genotype 1 or 4, liver transplant recipients without cirrhosis or with compensated cirrhosis (Child-Pugh class A) (alternative regimen; off-label use): 150 mg once daily in combination with sofosbuvir with or without ribavirin for 12 weeks (AASLD/IDSA 2018).
Dosage adjustment for concomitant therapy: Significant drug interactions exist, requiring dose/frequency adjustment or avoidance. Consult drug interactions database for more information.
Dosing: Geriatric
Refer to adult dosing.
Administration
Oral: Administer with food. Swallow capsules whole; do not chew, crush, break, cut, or dissolve the capsule.
Storage
Store below 30°C (86°F). Store in the original bottle. Protect from light.
Drug Interactions
Abametapir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Afatinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Afatinib. Management: If combined, administer the P-gp inhibitor simultaneously with, or after, the dose of afatinib. Monitor closely for signs and symptoms of afatinib toxicity and if the combination is not tolerated, reduce the afatinib dose by 10 mg. Consider therapy modification
Aliskiren: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Aliskiren. Monitor therapy
Alpelisib: BCRP/ABCG2 Inhibitors may increase the serum concentration of Alpelisib. Management: Avoid coadministration of BCRP/ABCG2 inhibitors and alpelisib due to the potential for increased alpelisib concentrations and toxicities. If coadministration cannot be avoided, closely monitor for increased alpelisib adverse reactions. Consider therapy modification
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Antidiabetic Agents: Direct Acting Antiviral Agents (HCV) may enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Asunaprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Asunaprevir. Avoid combination
AtorvaSTATin: Simeprevir may increase the serum concentration of AtorvaSTATin. Management: The maximum atorvastatin dose should not exceed 40 mg/day with concurrent use of simeprevir, and use of the lowest necessary atorvastatin dose is recommended. Monitor for atorvastatin toxicity with concomitant use. Consider therapy modification
Betrixaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Betrixaban. Management: Decrease adult betrixaban dose to an initial single dose of 80 mg followed by 40 mg once daily if combined with a P-gp inhibitor. Avoid concomitant use of betrixaban and P-gp inhibitors in patients with severe renal impairment (CrCL less than 30 mL/min). Consider therapy modification
Bilastine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Bilastine. Avoid combination
Celiprolol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Celiprolol. Monitor therapy
Cisapride: Simeprevir may increase the serum concentration of Cisapride. Avoid combination
Cladribine: BCRP/ABCG2 Inhibitors may increase the serum concentration of Cladribine. Management: Avoid concomitant use of BCRP inhibitors during the 4 to 5 day oral cladribine treatment cycles whenever possible. If combined, consider dose reduction of the BCRP inhibitor and separation in the timing of administration. Consider therapy modification
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CloZAPine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of CloZAPine. Monitor therapy
Colchicine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Colchicine. Colchicine distribution into certain tissues (e.g., brain) may also be increased. Management: Colchicine is contraindicated in patients with impaired renal or hepatic function who are also receiving a P-gp inhibitor. In those with normal renal and hepatic function, reduce colchicine dose as directed. See interaction monograph for details. Consider therapy modification
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CycloSPORINE (Systemic): Simeprevir may increase the serum concentration of CycloSPORINE (Systemic). CycloSPORINE (Systemic) may increase the serum concentration of Simeprevir. Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of Simeprevir. Avoid combination
CYP3A4 Inducers (Strong): May decrease the serum concentration of Simeprevir. Avoid combination
CYP3A4 Inhibitors (Moderate): May increase the serum concentration of Simeprevir. Avoid combination
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Simeprevir. Avoid combination
CYP3A4 Substrates (High risk with Inhibitors): Simeprevir may increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inhibitors may increase serum concentrations of the active metabolite(s) of Dabigatran Etexilate. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Delavirdine: May increase the serum concentration of Simeprevir. Avoid combination
DexAMETHasone (Systemic): May decrease the serum concentration of Simeprevir. Avoid combination
Digitoxin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Digitoxin. Monitor therapy
Digoxin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Digoxin. Management: Measure digoxin serum concentrations before initiating treatment with these P-glycoprotein (P-gp) inhibitors. Reduce digoxin concentrations by either reducing the digoxin dose by 15% to 30% or by modifying the dosing frequency. Consider therapy modification
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of DOXOrubicin (Conventional). Avoid combination
Edoxaban: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Edoxaban. Monitor therapy
Elagolix: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Elagolix. Avoid combination
Elagolix, Estradiol, and Norethindrone: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Elagolix, Estradiol, and Norethindrone. Specifically, concentrations of elagolix may be increased. Avoid combination
Eltrombopag: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Eluxadoline: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Eluxadoline. Management: Decrease the eluxadoline dose to 75 mg twice daily if combined with OATP1B1/1B3 inhibitors and monitor patients for increased eluxadoline effects/toxicities. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Erythromycin (Systemic): May increase the serum concentration of Simeprevir. Simeprevir may increase the serum concentration of Erythromycin (Systemic). Avoid combination
Escitalopram: May decrease the serum concentration of Simeprevir. Monitor therapy
Etoposide: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Etoposide. Monitor therapy
Etoposide Phosphate: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Etoposide Phosphate. Monitor therapy
Everolimus: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Everolimus. Monitor therapy
Flecainide: Simeprevir may increase the serum concentration of Flecainide. Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Gemfibrozil: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. See separate drug interaction monographs for agents listed as exceptions. Monitor therapy
Glecaprevir and Pibrentasvir: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Glecaprevir and Pibrentasvir. Monitor therapy
Grazoprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Grazoprevir. Avoid combination
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Lapatinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Lapatinib. Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Larotrectinib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Larotrectinib. Monitor therapy
Ledipasvir: Simeprevir may increase the serum concentration of Ledipasvir. Ledipasvir may increase the serum concentration of Simeprevir. Avoid combination
Lovastatin: Simeprevir may increase the serum concentration of Lovastatin. Monitor therapy
Mexiletine: Simeprevir may increase the serum concentration of Mexiletine. Monitor therapy
Midazolam: Simeprevir may increase the serum concentration of Midazolam. Monitor therapy
Milk Thistle: May increase the serum concentration of Simeprevir. Avoid combination
Morphine (Systemic): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Morphine (Systemic). Monitor therapy
Nadolol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Nadolol. Monitor therapy
Naldemedine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naldemedine. Monitor therapy
Naloxegol: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Naloxegol. Monitor therapy
Nevirapine: May decrease the serum concentration of Simeprevir. Avoid combination
OXcarbazepine: May decrease the serum concentration of Simeprevir. Avoid combination
Ozanimod: BCRP/ABCG2 Inhibitors may increase serum concentrations of the active metabolite(s) of Ozanimod. Avoid combination
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
PAZOPanib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
PAZOPanib: BCRP/ABCG2 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Phosphodiesterase 5 Inhibitors: Simeprevir may increase the serum concentration of Phosphodiesterase 5 Inhibitors. Monitor therapy
Pitavastatin: Simeprevir may increase the serum concentration of Pitavastatin. Monitor therapy
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Pravastatin: Simeprevir may increase the serum concentration of Pravastatin. Monitor therapy
Propafenone: Simeprevir may increase the serum concentration of Propafenone. Monitor therapy
Protease Inhibitors: May increase the serum concentration of Simeprevir. Simeprevir may increase the serum concentration of Protease Inhibitors. Avoid combination
Ranolazine: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Ranolazine. Monitor therapy
Revefenacin: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase serum concentrations of the active metabolite(s) of Revefenacin. Avoid combination
RifAXIMin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of RifAXIMin. Monitor therapy
Rimegepant: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Rimegepant. Avoid combination
RisperiDONE: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of RisperiDONE. Monitor therapy
RomiDEPsin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of RomiDEPsin. Monitor therapy
Rosuvastatin: Simeprevir may increase the serum concentration of Rosuvastatin. Management: Limit initial rosuvastatin dose to 5 mg/day when being started in a patient who is also being treated with simeprevir. The maximum rosuvastatin dose should not exceed 10 mg/day with concurrent use of simeprevir. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Silodosin: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Silodosin. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simvastatin: Simeprevir may increase the serum concentration of Simvastatin. Monitor therapy
St John's Wort: May decrease the serum concentration of Simeprevir. Avoid combination
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tacrolimus (Systemic): Simeprevir may decrease the serum concentration of Tacrolimus (Systemic). Tacrolimus (Systemic) may increase the serum concentration of Simeprevir. Monitor therapy
Talazoparib: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Talazoparib. Monitor therapy
Talazoparib: BCRP/ABCG2 Inhibitors may increase the serum concentration of Talazoparib. Monitor therapy
Tegaserod: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Tegaserod. Monitor therapy
Teniposide: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Teniposide. Monitor therapy
Tenofovir Disoproxil Fumarate: May decrease the serum concentration of Simeprevir. Simeprevir may increase the serum concentration of Tenofovir Disoproxil Fumarate. Monitor therapy
Teriflunomide: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Theophylline Derivatives: CYP1A2 Inhibitors (Weak) may increase the serum concentration of Theophylline Derivatives. Monitor therapy
TiZANidine: CYP1A2 Inhibitors (Weak) may increase the serum concentration of TiZANidine. Management: Avoid these combinations when possible. If combined use is necessary, initiate tizanidine at an adult dose of 2 mg and increase in 2 to 4 mg increments based on patient response. Monitor for increased effects of tizanidine, including adverse reactions. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tolvaptan: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Tolvaptan. Monitor therapy
Topotecan: BCRP/ABCG2 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Topotecan: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Triazolam: Simeprevir may increase the serum concentration of Triazolam. Monitor therapy
Ubrogepant: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 50 mg and second dose (at least 2 hours later if needed) of 50 mg when used with a P-gp inhibitor. Consider therapy modification
Venetoclax: P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of Venetoclax. Management: Reduce the venetoclax dose by at least 50% in patients requiring concomitant treatment with P-glycoprotein (P-gp) inhibitors. Resume the previous venetoclax dose 2 to 3 days after discontinuation of a P-gp inhibitor. Consider therapy modification
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inhibitors may increase the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vitamin K Antagonists (eg, warfarin): Direct Acting Antiviral Agents (HCV) may diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Voxilaprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Voxilaprevir. Avoid combination
Adverse Reactions
The following adverse drug reactions and incidences are derived from product labeling unless otherwise specified.
Percentages reported for combination therapy with peginterferon alfa and ribavirin (Peg-IFN-alfa and RBV) unless otherwise noted.
>10%:
Central nervous system: Headache (with sofosbuvir 7% to 49%), fatigue (with sofosbuvir 10% to 47%), insomnia (with sofosbuvir 14%), dizziness (with sofosbuvir 5% to 10%)
Dermatologic: Skin photosensitivity (with sofosbuvir ≤5% to ≤34%; grade 3: ≤1%; with Peg-IFN-alfa and RBV ≤28%; grade 3: <1%), skin rash (with sofosbuvir ≤5% to ≤34%; grade 3: ≤1%; with Peg-IFN-alfa and RBV ≤28%; including erythema, eczema, maculopapular rash, urticaria, toxic skin eruption, dermatitis exfoliative, cutaneous vasculitis; grade 3: ≤1%), pruritus (with Peg-IFN-alfa and RBV 22%; with sofosbuvir 11%)
Endocrine & metabolic: Increased amylase (with sofosbuvir)
Gastrointestinal: Nausea (with sofosbuvir 4% to 40%; with Peg-IFN-alfa and RBV 22%), diarrhea (with sofosbuvir 5% to 18%)
Hepatic: Increased serum bilirubin (<66%), hyperbilirubinemia (with sofosbuvir)
Neuromuscular & skeletal: Myalgia (16%)
Respiratory: Dyspnea (12%)
1% to 10%:
Gastrointestinal: Increased serum lipase (with sofosbuvir)
Hepatic: Increased serum alkaline phosphatase
<1%, postmarketing, and/or case reports: Hepatic failure, liver decompensation, reactivation of HBV (FDA Safety Alert Dec. 8, 2016)
ALERT: U.S. Boxed Warning
Hepatitis B virus reactivation:Test all patients for evidence of current or prior hepatitis B virus (HBV) infection before initiating treatment with simeprevir. HBV reactivation has been reported in hepatitis C virus (HCV)/HBV co-infected patients who were undergoing or had completed treatment with HCV direct-acting antivirals and were not receiving HBV antiviral therapy. Some cases have resulted in fulminant hepatitis, hepatic failure, and death. Monitor HCV/HBV co-infected patients for hepatitis flare or HBV reactivation during HCV treatment and post-treatment follow-up. Initiate appropriate patient management for HBV infection as clinically indicated.
Warnings/Precautions
Concerns related to adverse effects:
• Hepatic decompensation/failure: Hepatic decompensation and failure (including fatal cases) have been reported in patients treated with simeprevir in combination with peginterferon alfa and ribavirin or sofosbuvir. Most cases occurred in patients with advanced and/or decompensated cirrhosis. Modest bilirubin level increases, not impacting hepatic function, have been reported; however, postmarketing cases of hepatic decompensation with markedly elevated bilirubin levels have also been reported. Monitor hepatic function at baseline and as clinically indicated; closely monitor patients who experience an increase in total bilirubin >2.5 times the ULN. Discontinue treatment if elevated bilirubin accompanied by liver transaminase increases or clinical signs or symptoms of hepatic decompensation (eg, fatigue, weakness, lack of appetite, nausea and vomiting, jaundice, discolored feces) occur.
• Photosensitivity: Photosensitivity reactions, including serious reactions resulting in hospitalization, have been reported when used in combination with peginterferon alfa and ribavirin. May present as an exaggerated sunburn reaction (burning, erythema, exudation, blistering, and edema), usually to areas exposed to light (face, “v” area of the neck, extensor surfaces of the forearms, dorsa of the hands); most frequently occurs within the first 4 weeks of treatment. Avoid excessive sunlight, tanning devices, and take precautions to limit exposure (eg, loose fitting clothing, sunscreen). Discontinue use if photosensitivity occurs and monitor until the reaction resolves. If therapy is to be continued in a patient who has experienced photosensitivity, expert consultation is advised.
• Skin reactions: Rash has been typically observed within first 4 weeks of therapy initiation, but can occur at any time during treatment. Severe rashes and rash requiring discontinuation have occurred in combination with peginterferon alfa and ribavirin. If a patient experiences a mild to moderate rash, follow for progression and/or development of mucosal signs (eg, oral lesions, conjunctivitis) or systemic symptoms. If rash becomes severe, discontinue simeprevir and monitor for rash resolution.
• Sulfa allergy: Contains a sulfonamide moiety. In patients with a history of sulfa allergy, no increased incidence of rash or photosensitivity has been reported, although the risk of reaction (or potential severity) cannot be excluded. Discontinue if signs of hypersensitivity are noted.
Disease-related concerns:
• Diabetes: Rapid reduction in hepatitis C viral load during direct-acting antiviral (DAA) therapy for hepatitis C may lead to improvement in glucose metabolism in patients with diabetes, potentially resulting in symptomatic hypoglycemia if antidiabetic agents are continued at the same dose. Monitor for changes in glucose tolerance and inform patients of the risk of hypoglycemia during DAA therapy, particularly within the first 3 months. Modification of antidiabetic therapy may be necessary (Ciancio 2018; Dawood 2017; Hum 2017).
• Hepatic impairment: Not recommend in patients with moderate or severe hepatic impairment (Child-Pugh class B or C).
• Hepatitis B virus reactivation: [US Boxed Warning]: Hepatitis B virus (HBV) reactivation has been reported in hepatitis C virus (HCV)/HBV co-infected patients who were receiving or had completed treatment with HCV direct-acting antivirals and were not receiving HBV antiviral therapy; some cases have resulted in fulminant hepatitis, hepatic failure, and death. Test all patients for evidence of current or prior HBV infection prior to initiation of simeprevir; monitor HCV/HBV co-infected patients for hepatitis flare or HBV reactivation during treatment and post-treatment follow-up. Initiate treatment for HBV infection as clinically indicated. HBV reactivation has been reported in HBsAg positive patients and in patients with serologic evidence of resolved HBV infection (ie, HBsAg negative and anti-HBc positive) and is characterized by an abrupt increase in HBV replication manifested as a rapid increase in serum HBV DNA level; reappearance of HBsAg may occur in patients with resolved HBV infection. Risk of HBV reactivation may be increased in patients receiving certain immunosuppressants or chemotherapeutic agents.
Concurrent drug therapy issues:
• Amiodarone: Symptomatic bradycardia (some requiring pacemaker intervention) has occurred in patients receiving amiodarone and sofosbuvir in combination with another direct acting antiviral, including simeprevir. Fatal cardiac arrest occurred in a patient receiving a sofosbuvir (eg, ledipasvir/sofosbuvir) combination product. Bradycardia generally occurred within hours to days following coadministration; however, some cases have occurred 2 weeks following the initiation of HCV treatment. The risk of bradycardia may be increased in patients taking beta blockers or patients with underlying cardiac comorbidities and/or advanced liver disease. Bradycardia generally resolves following discontinuation of HCV treatment. Coadministration of amiodarone with simeprevir and sofosbuvir in combination is not recommended. However, if patients have no treatment alternatives, patients should be counseled about the interaction and have in-patient cardiac monitoring for the first 48 hours of coadministration followed by daily outpatient or self-monitoring of heart rate for at least the first 2 weeks of treatment. Due to the long half-life of amiodarone, cardiac monitoring (as described) is also recommended if amiodarone was discontinued just prior to beginning treatment with sofosbuvir and simeprevir. Patients should seek medical attention immediately if they experience fainting or near-fainting, dizziness, lightheadedness, malaise, weakness, excessive tiredness, shortness of breath, chest pains, confusion, or memory problems.
Other warnings/precautions:
• Appropriate use: Do not use as monotherapy; use only as part of a multiple-drug regimen for treatment of HCV; consult current HCV treatment guidelines for guidance (AASLD/IDSA 2018).
• Resistance: Reduced sustained virologic response (SVR) rates of simeprevir in combination with sofosbuvir were observed in patients infected with hepatitis C genotype 1a with an NS3 Q80K polymorphism compared to patients without the polymorphism; consider alternative therapy in these patients. Patients with compensated cirrhosis and hepatitis C genotype 1a should be evaluated for the presence of the Q80K polymorphism; alternative regimens should be used if Q80K variant is present (Lawitz 2016).
Monitoring Parameters
Baseline (within 12 weeks prior to treatment initiation) CBC, INR, hepatic function (albumin, total and direct bilirubin, ALT, AST, alkaline phosphatase), calculated GFR; baseline (obtain any time prior to treatment initiation) hepatitis C virus (HCV) genotype and subtype, quantitative HCV viral load. During treatment, monitor CBC, serum creatinine, calculated GFR, hepatic function panel (after 4 weeks of therapy and as clinically indicated); quantitative HCV viral load testing (after 4 weeks of therapy and at 12 weeks after completion of therapy). If quantitative HCV viral load is detectable at treatment week 4, repeat testing is recommended after 2 additional weeks of treatment (treatment week 6) (AASLD/IDSA 2018). Screen patients infected with HCV genotype 1a for the presence of virus with the NS3 Q80K polymorphism prior to the initiation of treatment.
Hepatitis B surface antigen and hepatitis B core antibody prior to initiation; in patients with serologic evidence of hepatitis B virus (HBV) infection, monitor for clinical and laboratory signs of hepatitis flare or HBV reactivation during treatment and during posttreatment follow-up.
Reproductive Considerations
HCV-infected females of childbearing potential should consider postponing pregnancy until therapy is complete to reduce the risk of HCV transmission (AASLD/IDSA 2018).
Simeprevir is not used as monotherapy; when used in combination with ribavirin, all warnings related to the use of ribavirin and contraception should be followed. Also refer to the ribavirin monograph for additional information.
Pregnancy Considerations
Simeprevir is not used as monotherapy; combination therapy with ribavirin is contraindicated in pregnant females and males whose female partners are pregnant. If used in combination with ribavirin, all warnings related to the use of ribavirin and pregnancy should be followed. Also refer to the ribavirin monograph for additional information.
Treatment of hepatitis C is not currently recommended to treat maternal infection or to decrease the risk of mother-to-child transmission during pregnancy (Tran 2016). When HCV infection is detected during pregnancy, treatment should be deferred until after delivery. Direct-acting antiviral medications should not be used in pregnant females outside of clinical trials until safety and efficacy information is available (SMFM [Hughes 2017]).
Patient Education
What is this drug used for?
• It is used to treat long-term hepatitis C infections.
All drugs may cause side effects. However, many people have no side effects or only have minor side effects. Call your doctor or get medical help if any of these side effects or any other side effects bother you or do not go away:
• Itching
• Nausea
• Muscle pain
• Diarrhea
• Dizziness
• Headache
• Loss of strength and energy
• Trouble sleeping
WARNING/CAUTION: Even though it may be rare, some people may have very bad and sometimes deadly side effects when taking a drug. Tell your doctor or get medical help right away if you have any of the following signs or symptoms that may be related to a very bad side effect:
• Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
• Shortness of breath
• Severe skin irritation
• Red, blistered, or swollen skin
• Mouth sores
• Eye irritation
• Signs of an allergic reaction, like rash; hives; itching; red, swollen, blistered, or peeling skin with or without fever; wheezing; tightness in the chest or throat; trouble breathing, swallowing, or talking; unusual hoarseness; or swelling of the mouth, face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a limited summary of general information about the medicine's uses from the patient education leaflet and is not intended to be comprehensive. This limited summary does NOT include all information available about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not intended to provide medical advice, diagnosis or treatment and does not replace information you receive from the healthcare provider. For a more detailed summary of information about the risks and benefits of using this medicine, please speak with your healthcare provider and review the entire patient education leaflet.
Frequently asked questions
More about simeprevir
- Check interactions
- Compare alternatives
- Reviews (4)
- Side effects
- Dosage information
- During pregnancy
- Drug class: protease inhibitors
- Breastfeeding
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.