Paricalcitol (Monograph)
Brand name: Zemplar
Drug class: Vitamin D
ATC class: A11CC
VA class: VT509
Chemical name: (1α,3β,7E,22E)-19-Nor-9,10-secoergosta-5,7,22-triene-1α,3β,25-triol
Molecular formula: C27H44O3
CAS number: 131918-61-1
Introduction
A synthetic vitamin D analog.
Uses for Paricalcitol
Secondary Hyperparathyroidism
IV paricalcitol used for prevention and treatment of secondary hyperparathyroidism associated with stage 5 chronic kidney disease (CKD).
Oral paricalcitol used for prevention and treatment of secondary hyperparathyroidism associated with stage 3 or 4 CKD or stage 5 CHD requiring hemodialysis or peritoneal dialysis.
Paricalcitol Dosage and Administration
General
-
Individualize dosage according to serum or plasma intact parathyroid hormone (iPTH) concentrations and serum concentrations of calcium and phosphorus. Nephrology experts currently recommend using individual values for serum calcium and phosphorus (evaluated together) instead of the mathematical construct of calcium times phosphorus product to guide clinical practice.
-
Closely monitor serum calcium and phosphorus concentrations during therapy. (See Patient Monitoring under Cautions.)
Administration
Oral Administration
Administer orally once daily or 3 times weekly without regard to meals.
If paricalcitol is administered 3 times weekly, administer no more frequently than every other day.
IV Administration
Administer by direct IV injection at any time during dialysis, no more frequently than every other day.
Dosage
Nephrology experts currently state that optimal iPTH concentration for predialysis patients with stage 3a (eGFR 45–59 mL/minute per 1.73 m2) to stage 5 (eGFR <15 mL/minute per 1.73 m2) CKD is unknown, but modest elevations may represent an appropriate adaptive response to declining renal function.
For patients with stage 5 CKD undergoing dialysis, some experts suggest maintaining iPTH concentrations within a range of approximately 2–9 times the assay's ULN (may correspond to range of approximately 130–600 pg/mL for commercial assays ). PTH assays exhibit substantial variability; previously recommended range of 150–300 pg/mL for patients with stage 5 CKD requiring dialysis was based on an assay that is no longer available.
Avoid oversuppression of PTH, which may increase risk of adynamic bone disease.
Pediatric Patients
Secondary Hyperparathyroidism
Stage 3 or 4 CKD
OralPediatric patients 10–16 years of age: Initial dosage of 1 mcg 3 times weekly.
Individualize dosage based on iPTH concentration and serum calcium and phosphorus concentrations to maintain iPTH concentration within the target range.
May increase dosage in increments of 1 mcg 3 times weekly (i.e., from 1 mcg 3 times weekly to 2 mcg 3 times weekly) at intervals of 4 weeks.
May decrease dose by 1 mcg at any time during therapy.
If patient is receiving 1 mcg 3 times weekly and requires dosage reduction, withhold therapy as needed and resume when appropriate.
If hypercalcemia is observed, reduce dosage or withhold therapy until the concentration has normalized.
Stage 5 CKD (Dialysis)
OralPediatric patients 10–16 years of age: Manufacturer recommends calculating initial dose (in mcg) by dividing baseline iPTH concentration (in pg/mL) by 120. Round calculated dose down to nearest whole number and administer 3 times weekly.
Individualize dosage based on iPTH concentration and serum calcium and phosphorus concentrations to maintain iPTH concentration within the target range.
May increase dosage in increments of 1 mcg 3 times weekly (i.e., from 1 mcg 3 times weekly to 2 mcg 3 times weekly) at intervals of 4 weeks.
May decrease dose by 2 mcg at any time during therapy.
If patient is receiving 1 or 2 mcg 3 times weekly and requires dosage reduction, withhold therapy as needed and resume when appropriate.
If hypercalcemia is observed, reduce dosage or withhold therapy until the concentration has normalized.
IVChildren and adolescents 5–19 years of age: In one study, initial dosage was 0.04 mcg/kg 3 times weekly if iPTH concentration <500 pg/mL or 0.08 mcg/kg 3 times weekly if iPTH concentration ≥500 pg/mL.
Dosage in this study was adjusted in increments of 0.04 mcg/kg based on serum concentrations of iPTH, calcium, and calcium times serum phosphorus product (Ca × P). Mean dose was 4.6 mcg (range: 0.8–9.6 mcg).
Adults
Secondary Hyperparathyroidism
Stage 3 or 4 CKD
OralIf baseline iPTH concentration is ≤500 pg/mL, manufacturer recommends initial dosage of 1 mcg once daily or 2 mcg 3 times weekly. If baseline iPTH concentration is >500 pg/mL, initial dosage of 2 mcg once daily or 4 mcg 3 times weekly.
Adjust dosage at 2- to 4-week intervals based on iPTH response.
Manufacturer recommends maintaining current dosage if decrease in iPTH concentration from baseline is ≥30% but ≤60%.
If response is inadequate (i.e., iPTH concentration increases, remains unchanged, or is reduced by <30% from baseline), manufacturer recommends increasing dosage in increments of 1 mcg daily (e.g., from 1 mcg daily to 2 mcg daily) or 2 mcg 3 times weekly (e.g., from 2 mcg 3 times weekly to 4 mcg 3 times weekly).
If iPTH concentration is decreased from baseline by >60% or declines to a value of <60 pg/mL, manufacturer recommends decreasing dosage by 1 mcg daily or by 2 mcg 3 times weekly.
If patient is receiving dosage of 1 mcg once daily and requires dosage reduction, reduce dosage to 1 mcg 3 times weekly; if further reduction is needed, withhold the drug as needed and reinitiate therapy at a lower dosage by altering dosing interval.
If hypercalcemia is observed, reduce dosage or withhold therapy until the concentration has normalized.
Stage 5 CKD (Dialysis)
OralManufacturer recommends calculating initial dose (in mcg) by dividing baseline iPTH concentration (in pg/mL) by 80; administer calculated dose 3 times weekly.
To minimize risk of hypercalcemia, initiate therapy only if adjusted baseline serum calcium concentration is ≤9.5 mg/dL.
Individualize dosage based on iPTH, serum calcium, and serum phosphorus concentrations. Manufacturer recommends calculating new dose (in mcg) by dividing most recent iPTH concentration (in pg/mL) by 80.
If hypercalcemia is observed, reduce dosage or withhold therapy until the concentration has normalized. If serum calcium concentrations are elevated, decrease dose by 2–4 mcg.
As iPTH concentration approaches target range, small individualized dose adjustments may be necessary to achieve a stable iPTH concentration.
In situations where iPTH, calcium, or phosphorus is monitored less frequently than once weekly, manufacturer states that a more modest initial and dose-titration ratio (e.g., iPTH concentration divided by 100) may be appropriate.
IVInitial dosage of 0.04–0.1 mcg/kg (2.8–7 mcg) at dialysis (no more often than every other day).
Manufacturer recommends adjusting dosage at 2- to 4-week intervals with the goal of reducing iPTH concentration to no more than 1.5–3 times ULN.
Manufacturer recommends maintaining current dosage if decrease in iPTH concentration from baseline is ≥30% but ≤60% or if iPTH concentration is 1.5–3 times the ULN.
If response is inadequate (i.e., iPTH concentration increases, remains unchanged, or is reduced by <30% from baseline), manufacturer recommends increasing dose by 2–4 mcg per dose at 2- to 4-week intervals.
If iPTH concentration is decreased from baseline by >60%, reduce dosage.
If serum calcium (in mg/dL) times serum phosphorus (in mg/dL) product (Ca × P) is >75, reduce or withhold dosage immediately until parameters are normalized; reinitiate drug at a lower dosage.
In patients receiving a calcium-containing phosphate binder, dosage of the phosphate binder may be reduced or withheld; alternatively, the patient can be switched to a non-calcium-containing phosphate binder.
Special Populations
Hepatic Impairment
Mild to moderate hepatic impairment: Dosage adjustment not required. (See Hepatic Impairment under Cautions.)
Geriatric Patients
No specific dosage recommendations. (See Geriatric Use under Cautions.)
Related/similar drugs
cinacalcet, Sensipar, doxercalciferol, Hectorol, Zemplar
Cautions for Paricalcitol
Contraindications
-
Hypercalcemia.
-
Evidence of vitamin D toxicity.
-
Known hypersensitivity to paricalcitol or any ingredient in the formulation.
Warnings/Precautions
Excessive Use
Excessive doses of vitamin D analogs (e.g., paricalcitol) may result in excessive suppression of PTH concentrations, hypercalcemia, hypercalciuria, hyperphosphatemia, and adynamic bone disease.
Hypercalcemia
Progressive hypercalcemia resulting from vitamin D overdosage may require emergency treatment measures. If clinically important hypercalcemia develops, reduce or withhold paricalcitol therapy immediately, withdraw calcium supplements, administer a low-calcium diet, and monitor closely for changes in fluid and electrolyte balance and ECG (especially in those receiving a cardiac glycoside).
Acute hypercalcemia may increase risk of cardiac arrhythmias and seizures, and potentiate toxic effects of cardiac glycosides.
Chronic hypercalcemia increases risk of soft-tissue calcification, including vascular calcification.
Concomitant use of high dosages of calcium or thiazide diuretics increases risk of hypercalcemia; high intake of calcium and phosphates may necessitate frequent patient monitoring and individualized dosage titration.
Do not use prescription-based doses of vitamin D and its analogs during paricalcitol therapy.
Cardiac Glycoside Toxicity
Hypercalcemia increases risk of cardiac glycoside toxicity; use concomitantly with caution. (See Specific Drugs and Foods under Interactions.)
Patient Monitoring
In patients receiving oral paricalcitol, monitor serum calcium, serum phosphorus, and serum or plasma iPTH concentrations at least every 2 weeks for 3 months after initiation of therapy or following any dosage adjustment, then monthly for 3 months, and every 3 months thereafter.
In patients with stage 5 CKD receiving IV paricalcitol, monitor serum calcium and phosphorus concentrations frequently (e.g., twice weekly) during initial dosage adjustment and after subsequent dosage adjustments; once dosage has been established, monitor at least monthly. Monitor serum or plasma iPTH concentrations every 3 months; more frequent monitoring may be required during dosage adjustments.
Predialysis Patients
Vitamin D analogs (e.g., paricalcitol, calcitriol) may increase Scr and therefore decrease eGFR in predialysis patients.
Aluminum Toxicity
Avoid long-term concomitant use of aluminum-containing preparations (e.g., antacids, phosphate binders); risk of increased blood aluminum concentrations and aluminum bone toxicity.
Specific Populations
Pregnancy
Category C.
Limited data on paricalcitol use in pregnant women.
Slight increase in embryofetal loss observed in animals; increased stillbirths and newborn mortality observed in animals at maternally toxic doses.
CKD increases maternal risk for hypertension, spontaneous abortion, preterm labor, and preeclampsia and increases fetal risk for intrauterine growth restriction, prematurity, polyhydramnios, stillbirth, and low birth weight.
Lactation
Distributed into milk in rats; not known whether paricalcitol distributes into human milk, affects milk production, or affects nursing infants.
Avoid nursing during paricalcitol therapy.
Pediatric Use
Safety and efficacy of oral paricalcitol not established in pediatric patients <10 years of age.
Safety and efficacy of IV paricalcitol not established in pediatric patients <5 years of age.
Geriatric Use
No substantial differences in safety and efficacy in those ≥65 years of age relative to younger adults, but increased sensitivity cannot be ruled out.
Hepatic Impairment
Not studied in patients with severe hepatic impairment.
Mild or moderate hepatic impairment does not alter pharmacokinetics.
Common Adverse Effects
Oral administration in patients with stage 3 or 4 CKD: Diarrhea, hypertension, viral infection, edema, hypersensitivity, nausea, arthritis, dizziness, headache, hypotension, vertigo, vomiting.
Oral administration in patients with stage 5 CKD: Diarrhea, nasopharyngitis, dizziness, vomiting, constipation, fluid overload, insomnia, peritonitis.
IV administration in patients with stage 5 CKD: Nausea, vomiting, edema, arthralgia, chills, GI hemorrhage, influenza, pneumonia, pyrexia, sepsis.
Drug Interactions
Partially metabolized by CYP3A.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Potent CYP3A inhibitors: Potential pharmacokinetic interaction (increased plasma paricalcitol concentrations).
CYP substrates: Does not appear to inhibit clearance of drugs metabolized by CYP isoenzymes 1A2, 2A6, 2B6, 2C8, 2C9, 2C19, 2D6, 2E1, or 3A, or induce clearance of drugs metabolized by CYP isoenzymes 2B6, 2C9, or 3A.
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Antifungals, azoles (itraconazole, ketoconazole, posaconazole, voriconazole) |
Possible increased plasma paricalcitol concentrations Ketoconazole: Increased paricalcitol AUC and half-life |
Dosage adjustment of paricalcitol may be needed Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing therapy with a potent CYP3A4 inhibitor |
|
Bile acid sequestrants cholestyramine, colestipol) |
Intestinal absorption of paricalcitol may be decreased |
Allow as long a time interval as possible between ingestion of paricalcitol and bile acid sequestrant Cholestyramine: Administer oral paricalcitol >1 hour before or 4–6 hours after cholestyramine (or at longest possible interval) |
|
Cardiac glycosides |
Possible cardiac arrhythmias |
Use concomitantly with caution |
|
Clarithromycin |
Possible increased plasma paricalcitol concentrations |
Dosage adjustment of paricalcitol may be needed Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing clarithromycin therapy |
|
Conivaptan |
Possible increased plasma paricalcitol concentrations |
Dosage adjustment of paricalcitol may be needed Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing conivaptan therapy |
|
Grapefruit juice |
Possible increased plasma paricalcitol concentrations |
Dosage adjustment of paricalcitol may be needed Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing use of a potent CYP3A4 inhibitor |
|
HIV protease inhibitors (atazanavir, indinavir, lopinavir/ritonavir, nelfinavir, ritonavir, saquinavir) |
Possible increased plasma paricalcitol concentrations |
Dosage adjustment of paricalcitol may be needed Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing therapy with an HIV protease inhibitor |
|
Mineral oil |
May interfere with intestinal absorption of vitamin D analogs |
Administer oral paricalcitol >1 hour before or 4–6 hours after mineral oil (or at longest possible interval) |
|
Nefazodone |
Possible increased plasma paricalcitol concentrations |
Dosage adjustment of paricalcitol may be needed Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing nefazodone therapy |
|
Omeprazole |
No apparent effect on paricalcitol pharmacokinetics |
|
|
Telithromycin |
Possible increased plasma paricalcitol concentrations |
Dosage adjustment of paricalcitol may be needed Closely monitor iPTH and serum calcium concentrations when initiating or discontinuing telithromycin therapy |
|
Thiazide diuretics |
Possible increased risk of hypercalcemia |
Paricalcitol Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration; absolute bioavailability is about 72–86%.
Food
High-fat meal increased time to peak plasma concentration of paricalcitol capsules by about 2 hours but did not affect AUC or peak concentration.
Special Populations
Hemodialysis does not appear to affect plasma concentrations.
Distribution
Distributed into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
≥99.8%.
Elimination
Metabolism
Extensively metabolized (about 98%) by multiple hepatic and nonhepatic enzymes (e.g., CYP24, CYP3A4, uridine diphosphate-glucuronosyltransferase [UGT] 1A4).
Elimination Route
Paricalcitol and its metabolites eliminated principally in feces via biliary excretion.
Excreted in feces mainly (about 63–70%) as metabolites (2% as unchanged drug), and in urine as metabolites (18–19%).
Half-Life
In healthy individuals: 4–7 hours.
Special Populations
Pharmacokinetic profile of oral paricalcitol in patients with stage 5 CKD undergoing hemodialysis or peritoneal dialysis similar to that in patients with stage 3 or 4 CKD.
Half-life following oral administration: 14–20 hours in patients with stage 3 or 4 CKD or stage 5 CKD undergoing hemodialysis or peritoneal dialysis.
Half-life following IV administration: 13.9 hours in patients with stage 5 CKD undergoing hemodialysis and 15.4 hours in those with stage 5 CKD undergoing peritoneal dialysis.
Mild or moderate hepatic impairment does not alter pharmacokinetics.
Stability
Storage
Oral
Capsules
25°C (may be exposed to 15–30°C).
Parenteral
Injection
25°C (may be exposed to 15–30°C).
Multidose vial: Stable at room temperature for up to 7 days after initial use.
Actions
-
A synthetic vitamin D analog of calcitriol (the metabolically active form of vitamin D).
-
In patients with CKD, decreased metabolic activation of vitamin D in the kidneys results in secondary hyperparathyroidism, characterized by increased PTH concentrations and disturbances in calcium and phosphorus homeostasis. These effects may affect bone turnover rate and may result in renal osteodystrophy.
-
Biologic actions of paricalcitol are mediated through binding of the vitamin D receptor, which results in selective activation of vitamin D responsive pathways.
-
Paricalcitol reduces serum or plasma PTH concentrations in patients with CKD. Appears to be as effective as calcitriol in suppressing PTH secretion.
Advice to Patients
-
Importance of adherence to diet and calcium supplementation regimen.
-
Importance that patients with CKD use appropriate types of phosphate-binding compounds to control serum phosphate concentrations; importance of avoiding excessive use of aluminum-containing compounds.
-
Importance of laboratory monitoring (e.g., serum calcium, phosphorus, and iPTH) during paricalcitol therapy.
-
Importance of reporting potential manifestations of hypercalcemia (e.g., tiredness, difficulty thinking, loss of appetite, nausea, vomiting, constipation, increased thirst, increased urination, weight loss).
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, and dietary or herbal supplements.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
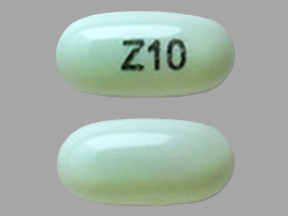
Oral |
Capsules, liquid-filled |
1 mcg* |
Paricalcitol Capsules |
|
|
Zemplar |
AbbVie |
|||
|
2 mcg* |
Paricalcitol Capsules |
|||
|
Zemplar |
AbbVie |
|||
|
4 mcg* |
Paricalcitol Capsules |
|||
|
Parenteral |
Injection, for IV use only |
2 mcg/mL* |
Paricalcitol Injection |
|
|
Zemplar |
AbbVie |
|||
|
5 mcg/mL* |
Paricalcitol Injection |
|||
|
Zemplar |
AbbVie |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions February 11, 2019. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about paricalcitol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: vitamins
- En español
Patient resources
- Paricalcitol drug information
- Paricalcitol (Intravenous) (Advanced Reading)
- Paricalcitol (Oral) (Advanced Reading)