Droxidopa (Monograph)
Brand name: Northera
Drug class: alpha- and beta-Adrenergic Agonists
Chemical name: (βR)-β,3-Dihydroxy-l-tyrosine
Molecular formula: C9H11NO5
CAS number: 23651-95-8
Warning
- Supine Hypertension
-
May cause or exacerbate supine hypertension in patients with neurogenic orthostatic hypotension (NOH). Risk of cardiovascular events may be increased in patients with uncontrolled supine hypertension.
-
Monitor supine BP prior to and during treatment and more frequently when increasing doses. To reduce the risk of supine hypertension, advise patients to elevate the head of the bed when sleeping or resting. Reduce dosage of droxidopa or discontinue drug if supine hypertension persists.
Introduction
Synthetic amino acid analog and prodrug of norepinephrine.
Uses for Droxidopa
Symptomatic Neurogenic Orthostatic Hypotension (NOH)
Management of orthostatic dizziness, lightheadedness, or the “feeling that you are about to black out” in patients with symptomatic NOH caused by primary autonomic failure (Parkinson's disease, multiple system atrophy, or pure autonomic failure), dopamine β-hydroxylase deficiency, or non-diabetic autonomic neuropathy.
Has been designated an orphan drug by FDA for treatment of symptomatic NOH in patients with primary autonomic failure, dopamine β-hydroxylase deficiency, or nondiabetic autonomic neuropathy.
Efficacy in symptomatic NOH beyond 2 weeks not established; reassess continued benefit periodically during therapy.
Droxidopa Dosage and Administration
General
Restricted Distribution
-
Available only through a specialty pharmacy. For more information, contact manufacturer at 844-601-0101 or [Web].
Administration
Oral Administration
Administer orally 3 times daily: upon arising in the morning, at midday, and in the late afternoon at least 3 hours before bedtime. Take consistently, either with food or without food. Swallow capsules whole.
Monitor supine BP prior to initiating droxidopa, periodically during treatment, and after dosage increases. (See Supine Hypertension under Cautions.)
If a dose is missed, skip the dose and take the next dose at the regularly scheduled time.
Dosage
Adults
Symptomatic NOH
Oral
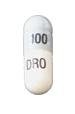
Initially, 100 mg 3 times daily. May increase dosage based on symptomatic response and tolerance in increments of 100 mg 3 times daily at intervals of 24–48 hours.
Efficacy beyond 2 weeks not established; periodically reassess continued benefit.
Prescribing Limits
Adults
Symptomatic NOH
Oral
600 mg 3 times daily (1.8 g daily).
Special Populations
Renal Impairment
Mild or moderate renal impairment when GFR >30 mL/minute: Dosage adjustment not necessary.
Limited experience in patients with severe renal impairment (GFR <30 mL/minute); no dosage recommendations provided by manufacturer.
Geriatric Patients
Manufacturer makes no special dosage recommendations.
Related/similar drugs
midodrine, phenylephrine, norepinephrine, ephedrine, Levophed, ProAmatine
Cautions for Droxidopa
Contraindications
-
None.
Warnings/Precautions
Warnings
Supine Hypertension
May cause or exacerbate supine hypertension. Risk of cardiovascular events may be increased in patients with uncontrolled supine hypertension.
Instruct patients to elevate the head of the bed when sleeping or resting to reduce risk of supine hypertension.
Monitor BP prior to initiating droxidopa, periodically during treatment, and more frequently when increasing dosage; measure BP both in the supine position and the recommended head-elevated sleeping position.
If supine hypertension persists, reduce dosage or discontinue droxidopa.
Sensitivity Reactions
Tartrazine Sensitivity
Preparations contain tartrazine (FD&C yellow No. 5), which may cause allergic reactions including bronchial asthma in susceptible individuals. Although the incidence of tartrazine sensitivity is low, it frequently occurs in aspirin-sensitive individuals.
General Precautions
Neuroleptic Malignant Syndrome (NMS)-like Reactions
Potentially life-threatening NMS-like reactions reported with droxidopa.
Symptoms may include hyperpyrexia, muscle rigidity, altered mental status (e.g., confusion), and autonomic instability. Monitor patients receiving droxidopa for the development of NMS-like symptoms; early diagnosis important for appropriate management.
Ischemic Heart Disease, Arrhythmias, and Congestive Heart Failure
May exacerbate ischemic heart disease, arrhythmias, and CHF. Consider risk in patients with these conditions when contemplating droxidopa therapy.
Specific Populations
Pregnancy
Category C.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Geriatric Use
No overall differences in safety or efficacy in geriatric patients compared with younger adults, but increased sensitivity cannot be ruled out.
Renal Impairment
Frequency of adverse events not affected by mild or moderate renal impairment when GFR >30 mL/minute. Insufficient experience in patients with severe renal impairment (GFR <30 mL/minute).
Common Adverse Effects
Headache, dizziness, nausea, hypertension. Longer-term open label studies: falls, urinary tract infections, headache, syncope, dizziness.
Drug Interactions
Metabolized via catecholamine pathway by catechol-O-methyltransferase (COMT), aromatic L-amino acid decarboxylase, and dihydroxyphenylserine (DOPS) aldolase.
Not metabolized by CYP isoenzymes.
Drugs Affecting Hepatic Microsomal Enzymes
No formal drug interaction studies to date. No interactions expected.
Drugs that Increase Blood Pressure
Possible increased risk for supine hypertension; use concomitantly with caution.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Amantadine derivatives |
No effect on droxidopa clearance |
No dosage adjustment required |
|
Aromatic L-amino acid decarboxylase inhibitors (e.g., carbidopa) |
May prevent conversion of droxidopa to norepinephrine outside the CNS Carbidopa: Decreased clearance of droxidopa and attenuated rises in plasma norepinephrine and BP reported |
Dosage adjustment of droxidopa may be required |
|
Dopamine agonists |
No effect on droxidopa clearance |
No dosage adjustment required |
|
MAO-B inhibitors |
No effect on droxidopa clearance |
No dosage adjustment required |
|
Serotonin type 1 (5-HT1) receptor agonists (triptans) |
Possible increased risk for supine hypertension |
Use concomitantly with caution |
Droxidopa Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentrations attained in approximately 1–4 hours (mean: about 2 hours) following oral administration. Plasma norepinephrine concentrations peak within 3–4 hours of oral administration but have no consistent relationship to droxidopa dosage.
Food
Administration with a high-fat meal delays absorption approximately 2 hours; peak plasma concentration and overall AUC decreased by 35 and 20%, respectively.
Distribution
Extent
Thought to cross the blood-brain barrier.
Distributed into milk in rats; not known whether distributed into human milk.
Plasma Protein Binding
75% plasma protein bound at 100 ng/mL and 26% at 10,000 ng/mL.
Elimination
Metabolism
Metabolized via catecholamine pathway by catechol-O-methyltransferase (COMT), dopa-decarboxylase, and DOPS aldolase.
Elimination Route
Following oral administration of radiolabeled dose in animals, approximately 75% of total radioactivity recovered in urine within 24 hours.
Half-life
Approximately 2.5 hours.
Stability
Storage
Oral
Capsules
25°C (may be exposed to 15–30°C).
Actions
-
Converted to norepinephrine by aromatic L-amino acid decarboxylase.
-
Precise mechanism of action not known, thought to be through action of norepinephrine, which causes peripheral vasoconstriction and increases BP.
Advice to Patients
-
Risk of increased BP and supine hypertension, which may lead to strokes, heart attacks, and death. Importance of advising patients to sleep in a position with upper body elevated and to monitor BP prior to initiating droxidopa, periodically during therapy, and during dosage increases. Importance of taking the late-afternoon dose of droxidopa at least 3 hours before bedtime.
-
Importance of instructing patients to take droxidopa in a consistent manner, either with or without food.
-
If a dose is missed, the dose should be skipped and the next dose taken at the regularly scheduled time. Importance of advising patients not to take 2 doses of the drug at the same time.
-
Importance of advising patients to notify their clinician if they are allergic to tartrazine (FD&C yellow No. 5) or aspirin.
-
Importance of advising patients to notify their clinician if any signs or symptoms of an allergic reaction (e.g., rash, hives, swelling, difficulty breathing) develop during droxidopa therapy.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs or herbal supplements that may have an additive effect with droxidopa, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Distribution of droxidopa is restricted. (See Restricted Distribution under Dosage and Administration.)
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
100 mg |
Northera |
Lundbeck |
|
200 mg |
Northera |
Lundbeck |
||
|
300 mg |
Northera |
Lundbeck |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions July 15, 2015. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
More about droxidopa
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (7)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: vasopressors
- En español