Atropine (Monograph)
Brand name: AtroPen
Drug class: Antimuscarinics/Antispasmodics
Warning
- Pesticide and Chemical Warfare Agent Poisoning
-
Primary protection against exposure to chemical nerve agents and insecticide poisoning is the wearing of protective garments (e.g., specialized masks).
-
Do not rely solely on antidotes such as atropine and pralidoxime to provide complete protection from chemical nerve agents and insecticide poisoning.
-
Seek immediate medical attention after injection with an atropine auto-injector.
Introduction
Antimuscarinic; a naturally occurring tertiary amine.
Uses for Atropine
Surgery
Used as a preoperative medication to inhibit salivation and excessive secretions of the respiratory tract (antisialagogue). However, current surgical practice (e.g., using general anesthetics that do not stimulate salivary and tracheobronchial secretions) has reduced the need to control excessive respiratory secretions during surgery.
Used to prevent other cholinergic effects during surgery (e.g., cardiac arrhythmias, hypotension, bradycardia) secondary to excessive vagal stimulation, carotid sinus stimulation, or pharmacologic effect of drugs (e.g., succinylcholine).
Used to block adverse muscarinic effects of anticholinesterase agents (e.g., neostigmine, pyridostigmine) that are used after surgery to reverse the effects of neuromuscular blocking agents.
Used as a premedication for bradycardia during emergency pediatric intubation. Not routinely recommended because of lack of supporting evidence, but may be considered in situations where there is an increased risk of bradycardia (e.g., when succinylcholine is used to facilitate intubation).
Ineffective for preventing acid-aspiration pneumonitis† [off-label] during surgery.
ACLS and Bradyarrhythmias
Used in ACLS for management of symptomatic bradycardia. Reverses cholinergically mediated decreases in heart rate, systemic vascular resistance, and BP.
Considered initial drug of choice in adults with unstable bradycardia (e.g., that accompanied by altered mental status, cardiac ischemia, acute heart failure, hypotension, or other signs of shock).
In pediatric advanced life support (PALS), used for treatment of bradycardia secondary to increased vagal activity or primary AV block when bradycardia persists despite adequate oxygenation, ventilation, and CPR (if indicated).
Previously included in ACLS guidelines for treatment of asystole or pulseless electrical activity (PEA) during CPR; however, routine use during cardiac arrest no longer recommended because of lack of evidence demonstrating benefit.
May be beneficial for treatment of AV nodal block. However, not likely to be effective in patients with type II second-degree or third-degree AV block, including third-degree AV block accompanied by a new wide QRS complex where location of block is at or below the His-Purkinje level; transcutaneous pacing or rate-accelerating β-adrenergic drugs (e.g., dopamine or epinephrine) preferred in these patients until transvenous pacing can be performed.
Used in patients with MI who develop symptomatic or hemodynamically unstable sinus bradycardia. Other uses in MI setting include treatment of sustained bradycardia and hypotension associated with nitroglycerin use, and treatment of nausea and vomiting associated with morphine use.
Use cautiously in the presence of acute myocardial ischemia or MI because heart rate is a major determinant of myocardial oxygen requirements.
May be ineffective in patients who have undergone cardiac transplantation due to lack of vagal innervation in transplanted heart. Risk of paradoxical slowing of the heart rate and high-degree AV block in patients receiving atropine after cardiac transplantation.
Pesticide Poisoning
Used concomitantly with a cholinesterase reactivator (pralidoxime chloride) to reverse muscarinic effects associated with toxic exposure to organophosphate anticholinesterase pesticides.
Used to reverse muscarinic effects associated with toxic exposure to carbamate anticholinesterase pesticides. Concomitant cholinesterase reactivator (pralidoxime chloride) therapy may not be necessary.
A challenge (test) dose of atropine may be useful in diagnosing cholinergic poisoning† [off-label]. Failure of the challenge dose to elicit typical antimuscarinic effects (e.g., mydriasis, tachycardia, dry mucous membranes) strongly suggests the presence of organophosphate or carbamate poisoning.
Use atropine in conjunction with other protective measures (e.g., decontamination, immediate evacuation, specialized masks and clothing) and treatments (e.g., anticonvulsant for seizures).
Chemical Warfare Agent Poisoning
Used concomitantly with a cholinesterase reactivator (pralidoxime chloride) to reverse muscarinic effects associated with toxic exposure to organophosphate anticholinesterase nerve agents (e.g., sarin, soman, tabun, VX [methylphosphonothioic acid]) in the context of chemical warfare or terrorism.
Initial management of nerve agent poisoning includes aggressive airway control and ventilation (administration of nebulized β-adrenergic agonist [e.g., albuterol] and antimuscarinics [e.g., ipratropium bromide] may be necessary), and administration of atropine and pralidoxime chloride; diazepam may be needed for seizure control.
Mushroom Poisoning
Treatment of muscarinic effects associated with toxic ingestion of mushrooms containing muscarine (e.g., certain members of the Clitocybe and Inocybe genera). However, substantial toxicity is uncommon, and supportive symptomatic care (e.g., atropine) rarely is necessary.
Radiographic Uses
Has been used to facilitate hypotonic duodenography or contrast examination of the colon; however, glucagon appears to be more effective and generally is preferred in these examinations.
Has been used to increase visualization of the urinary tract in excretion urography.
Bronchospasm
Has been used by oral inhalation as a bronchodilator for short-term treatment of bronchospasm associated with bronchial asthma, bronchitis, and COPD; however, a solution for oral inhalation no longer commercially available in the US.
GI Disorders
Has been used as an adjunct in the treatment of peptic ulcer disease; however, no conclusive data that the drug promotes healing, decreases rate of recurrence, or prevents complications of peptic ulcers.
With the advent of more effective therapies for the treatment of peptic ulcer disease, antimuscarinics have only limited usefulness in this condition.
Has been used in the treatment of functional disturbances of GI motility such as irritable bowel syndrome; however, efficacy is limited. Use only if other measures (e.g., diet, sedation, counseling, amelioration of environmental factors) have been of little or no benefit.
GU Disorders
Has been used as adjunctive therapy in the management of hypermotility disorders of the lower urinary tract. May provide symptomatic relief, but the underlying cause should be determined and specifically treated.
With the exception of uninhibited or reflex neurogenic bladder, there is generally little evidence to support the use of antimuscarinics in the treatment of various GU disorders.
Biliary Disorders
Has been used in conjunction with morphine or other opiates for symptomatic relief of biliary or renal colic; however, only exerts weak biliary antispasmodic action.
Pancreatitis
Has been used to reduce pain and hypersecretions in acute pancreatitis, but little evidence of benefit.
Atropine Dosage and Administration
Administration
Administer by sub-Q, IM, or direct IV injection. IV administration preferred for treatment of severe or life-threatening muscarinic effects.
Also has been administered by intraosseous (IO) injection† in the ACLS setting, generally when IV access not readily available; onset of action and systemic concentrations are comparable to those achieved with venous administration. May be administered endotracheally; however, vascular (IV or IO) administration preferred because of more predictable drug delivery and pharmacologic effect.
Has been administered orally; however, oral dosage form no longer commercially available in US.
Has been administered via oral inhalation for bronchodilation; however, solution for inhalation no longer commercially available in US.
IV Administration
Administer by direct IV injection.
Occasionally has been administered by IV infusion† [off-label] for management of muscarinic poisoning (e.g., organophosphate pesticides).
Rate of Administration
Preferably give IV injections rapidly because slow injection may cause a paradoxical slowing of the heart rate.
IM Administration
Commercially available in a prefilled auto-injector (e.g., AtroPen) for treatment of pesticide or nerve agent poisoning.
The AtroPen auto-injector may be self-administered by the patient or caregiver in an out-of-hospital setting to facilitate the initial treatment of muscarinic poisoning (usually breathing difficulty secondary to increased secretions); however, definitive medical care should be sought immediately.
For self-medication, instruct patients and caregivers carefully in proper administration techniques using auto-injector.
Inject weight-appropriate IM dose into anterolateral aspect of the thigh.
In very thin patients and small children, bunch up the thigh prior to injection to provide a thicker injection area.
AtroPen 0.5, 1, or 2 mg: Grasp prefilled auto-injector with green tip pointed downward; the yellow activation (safety) cap should be removed. Point green tip toward outer thigh and jab it firmly into outer thigh so that the auto-injector is perpendicular (90° angle) to the thigh, and hold firmly for at least 10 seconds until dose is delivered.
AtroPen 0.25 mg: Grasp prefilled auto-injector with black tip pointed downward; the grey activation (safety) cap should be removed. Point black tip toward outer thigh and jab it firmly into outer thigh so that the auto-injector is perpendicular (90° angle) to the thigh, and hold firmly for at least 10 seconds until dose is delivered.
Administer through clothing if necessary.
Massage injection area for several seconds.
Consult manufacturer's prescribing information for additional instructions on use of the auto-injectors.
Endotracheal Administration
When IV or IO† [off-label] access cannot be established, may administer by the endotracheal route.
For endotracheal administration in adults, dilute dose in 5–10 mL of 0.9% sodium chloride injection or sterile water.
In pediatric patients, flush with 5 mL of 0.9% sodium chloride injection after dose is administered.
Dosage
Individualize dosage based on indication, patient characteristics, and response (e.g., heart rate, BP); pediatric patients are more susceptible than adults to toxic effects of atropine overdosage.
Pediatric Patients
Surgery
Preoperatively for Antisialagogue or Antivagal Effects
IV, IM, or Sub-QDosing in pediatric patients not well studied.
Usual initial dose is 0.01–0.03 mg/kg, administered 30–60 minutes prior to surgery. May repeat every 4–6 hours.
Premedication for Bradycardia in Emergency Intubation
IVInfants and children: AHA recommends a preintubation dose of 0.02 mg/kg (with no minimum). Although minimum dose of 0.1 mg was previously recommended because of concerns about paradoxical bradycardia, current evidence suggests that minimum dose not necessary.
Muscarinic Blockade during Anticholinesterase Reversal of Neuromuscular Blocking Agents
Administer concurrently with (but in a separate syringe) or a few minutes before the anticholinesterase agent.
If bradycardia is present, administer before the anticholinesterase agent to increase pulse to about 80 bpm.
IVNeonates and infants: 0.02-mg/kg dose of atropine sulfate has been given concomitantly with each 0.04-mg/kg dose of neostigmine methylsulfate.
Children: 0.01- to 0.04-mg/kg dose of atropine sulfate has been given concomitantly with each 0.025- to 0.08-mg/kg dose of neostigmine methylsulfate.
PALS and Bradyarrhythmias
IV or IO† [off-label]
Infants and children with symptomatic bradycardia secondary to increased vagal activity or primary AV block: 0.02 mg/kg; repeat once if needed.
PALS guideline recommends minimum dose of 0.1 mg and maximum single dose of 0.5 mg.
Larger doses may be required in special resuscitation situations (e.g., organophosphate toxicity or exposure to nerve gas agents) and smaller doses (i.e., <0.1 mg) may cause paradoxical bradycardia.
Endotracheal
Infants and children: 0.04–0.06 mg/kg; repeat once if needed.
PALS guideline recommends minimum dose of 0.1 mg and maximum single dose of 0.5 mg.
Larger doses may be required in special resuscitation situations (e.g., organophosphate toxicity or exposure to nerve gas agents).
If CPR is in progress, stop chest compressions briefly to administer atropine; follow with a flush of at least 5 mL of 0.9% sodium chloride injection and 5 consecutive positive-pressure ventilations.
Pesticide Poisoning
Various doses and dosing intervals have been recommended; dosage requirements are based on severity of poisoning and individual patient response.
Organophosphate Anticholinesterase Pesticides
Preferably should be administered IV, especially the initial dose.
A cholinesterase reactivator (pralidoxime) is administered concomitantly.
Some degree of atropinism should be maintained for at least 48 hours; prolonged therapy (e.g., for several weeks) may be necessary in severe cases.
IV or IMChildren: 0.05–0.1 mg/kg every 5–10 minutes until muscarinic signs and symptoms disappear.
Alternatively, infuse IV† at a rate of 0.025 mg/kg per hour; continuous infusions have been maintained for up to several weeks in severe cases.
IM Self-administrationFor self-administration using a prefilled auto-injector (e.g., AtroPen), dose is based on body weight and symptom severity.
Mild symptoms include miosis, blurred vision, tearing, runny nose, hypersalivation, drooling, wheezing, muscle fasciculations, nausea/vomiting.
Severe symptoms include behavioral changes, severe breathing difficulty, severe respiratory secretions, severe muscle twitching, involuntary defecation or urination, seizures, unconsciousness.
Children <7 kg: Inject 0.25 mg IM initially for mild symptoms. If severe symptoms develop, inject 2 additional 0.25-mg IM doses in rapid succession 10 minutes after the initial dose.
Children <7 kg who present with severe symptoms or are unconscious: Inject three 0.25-mg IM doses in rapid succession.
Children <7 kg: Additional doses (i.e., >3) should only be administered under the supervision of trained medical personnel.
Children 7–18 kg: Inject 0.5 mg IM initially for mild symptoms. If severe symptoms develop, inject 2 additional 0.5-mg IM doses in rapid succession 10 minutes after the initial dose.
Children 7–18 kg who present with severe symptoms or are unconscious: Inject three 0.5-mg IM doses in rapid succession.
Children 7–18 kg: Additional doses (i.e., >3) should only be administered under the supervision of trained medical personnel.
Children 18–41 kg: Inject 1 mg IM initially for mild symptoms. If severe symptoms develop, inject 2 additional 1-mg IM doses in rapid succession 10 minutes after the initial dose.
Children 18–41 kg who present with severe symptoms or are unconscious: Inject three 1-mg IM doses in rapid succession.
Children 18–41 kg: Additional doses (i.e., >3) should only be administered under the supervision of trained medical personnel.
Children >41 kg: Inject 2 mg IM initially for mild symptoms. If severe symptoms develop, inject 2 additional 2-mg IM doses in rapid succession 10 minutes after the initial dose.
Children >41 kg who present with severe symptoms or are unconscious: Inject three 2-mg IM doses in rapid succession.
Children >41 kg: Additional doses (i.e., >3) should only be administered under the supervision of trained medical personnel.
EndotrachealChildren: 0.05–0.1 mg/kg every 5–10 minutes until muscarinic signs and symptoms disappear.
Dilute in 1–2 mL of 0.9% sodium chloride injection for endotracheal administration.
Carbamate Anticholinesterase Pesticides
Carbamate poisoning is treated with the same doses of atropine sulfate as for organophosphate poisoning and IM self-administration can be employed when necessary. (See Organophosphate Anticholinesterase Pesticides under Dosage.)
Concomitant cholinesterase reactivator (pralidoxime chloride) therapy may not be necessary and atropine therapy generally is less prolonged (e.g., only 1 or 2 days) and symptoms usually do not recur once asymptomatic.
Chemical Warfare Agent Poisoning
Various doses and dosing intervals have been recommended; dosage requirements are based on severity of poisoning and individual patient response.
Organophosphate Anticholinesterase Nerve Agents
Administer IM in out-of-hospital setting or emergency department.
A cholinesterase reactivator (pralidoxime chloride) is administered concomitantly.
Give diazepam for seizure control.
Total atropine sulfate doses usually are much less than those required for organophosphate anticholinesterase pesticide poisoning.
IMMinimum dose in children is 0.1 mg.
Children 0–2 years of age with mild to moderate symptoms: Usual initial IM dose is 0.05 mg/kg.
Children 0–2 years of age with severe symptoms: Usual initial IM dose is 0.1 mg/kg.
Children 2–10 years of age with mild to moderate symptoms: Usual initial IM dose is 1 mg.
Children 2–10 years of age with severe symptoms: Usual initial IM dose is 2 mg.
Children older than 10 years of age with mild to moderate symptoms: Usual initial IM dose is 2 mg.
Children older than 10 years of age with severe symptoms: Usual initial IM dose is 4 mg.
Repeat doses every 2–10 minutes as needed until muscarinic toxicity resolves (e.g., secretions have diminished and breathing is comfortable or airway resistance has returned to near normal).
IM Self-administrationFor self-administration using a prefilled auto-injector (e.g., AtroPen), dose is based on body weight and symptom severity.
Mild symptoms include miosis, blurred vision, tearing, runny nose, hypersalivation, drooling, wheezing, muscle fasciculations, nausea/vomiting.
Severe symptoms include behavioral changes, severe breathing difficulty, severe respiratory secretions, severe muscle twitching, involuntary defecation or urination, seizures, unconsciousness.
Children <7 kg: Inject 0.25 mg IM initially for mild symptoms. If severe symptoms develop, inject 2 additional 0.25-mg IM doses in rapid succession 10 minutes after the initial dose.
Children <7 kg who present with severe symptoms or are unconscious: Inject three 0.25-mg IM doses in rapid succession.
Children <7 kg: Additional doses (i.e., >3) should only be administered under the supervision of trained medical personnel.
Children 7–18 kg: Inject 0.5 mg IM initially for mild symptoms. If severe symptoms develop, inject 2 additional 0.5-mg IM doses in rapid succession 10 minutes after the initial dose.
Children 7–18 kg who present with severe symptoms or are unconscious: Inject three 0.5-mg IM doses in rapid succession.
Children 7–18 kg: Additional doses (i.e., >3) should only be administered under the supervision of trained medical personnel.
Children 18–41 kg: Inject 1 mg IM initially for mild symptoms. If severe symptoms develop, inject 2 additional 1-mg IM doses in rapid succession 10 minutes after the initial dose.
Children 18–41 kg who present with severe symptoms or are unconscious: Inject three 1-mg IM doses in rapid succession.
Children 18–41 kg: Additional doses (i.e., >3) may be given every 5–10 minutes but only under the supervision of trained medical personnel.
Children >41 kg: Inject 2 mg IM initially for mild symptoms. If severe symptoms develop, inject 2 additional 2-mg IM doses in rapid succession 10 minutes after the initial dose.
Children >41 kg who present with severe symptoms or are unconscious: Inject three 2-mg IM doses in rapid succession.
Children >41 kg: Additional doses (i.e., >3) may be given every 5–10 minutes but only under the supervision of trained medical personnel.
IVChildren 0–2 years of age with mild, moderate, or severe symptoms: May receive 0.02 mg/kg IV, if treated in an emergency department.
Mushroom Poisoning
Muscarine-containing Clitocybes and Inocybes
IVIf needed for severe symptoms, 0.02 mg/kg IV (minimum of 0.1 mg), repeated and titrated as needed according to response.
Adults
Surgery
Preoperatively for Antisialagogue or Antivagal Effects
IV, IM, or Sub-Q0.5–1 mg administered 30–60 minutes prior to surgery. May repeat in 1–2 hours.
Muscarinic Blockade during Anticholinesterase Reversal of Neuromuscular Blocking Agents
IV0.6–1.2 mg for each 0.5–2.5 mg of neostigmine methylsulfate or 10–20 mg of pyridostigmine bromide given.
Administer concurrently with (but in a separate syringe) or a few minutes before the anticholinesterase agent.
If bradycardia is present, administer before the anticholinesterase agent to increase pulse to 80 bpm.
ACLS and Bradyarrhythmias
Bradycardia
IVFor symptomatic bradycardia, AHA recommends initial dose of 0.5 mg; may repeat every 3–5 minutes up to 3 mg. Doses <0.5 mg may cause paradoxical slowing of heart rate.
Asystole or PEA
IV or IO†In previous ACLS guidelines, 1 mg every 3–5 minutes up to 3 doses recommended.
EndotrachealOptimum dose not established; typical doses 2–2.5 times usual IV doses.
One manufacturer recommends a dose of 1–2 mg (diluted in no more than 10 mL with sterile water or 0.9% sodium chloride injection).
Pesticide Poisoning
Various doses and dosing intervals have been recommended; dosage requirements are based on severity of poisoning and individual patient response.
Organophosphate Anticholinesterase Pesticides
Preferably should be administered IV, especially the initial dose.
A cholinesterase reactivator (pralidoxime chloride) is administered concomitantly.
Some degree of atropinism should be maintained for at least 48 hours; prolonged therapy (e.g., for several weeks) may be necessary in severe cases.
IV or IMUsual initial dose 1–2 mg IV (preferable) or IM; some clinicians recommend that additional 2-mg doses may be administered every 5–60 minutes until muscarinic symptoms disappear. For severe cases, 2–6 mg may be given initially, repeating doses every 5–60 minutes.
Alternatively, infuse IV at an initial rate of 0.5–1 mg/hour, adjusting rate according to response.
Mildly symptomatic poisoning may respond to 1–2 mg for reversal of muscarinic toxicity whereas moderate poisoning commonly requires total doses up to 40 mg.
For severe poisoning, 5-mg doses may be repeated every 2–3 minutes for stabilization.
Cumulative doses up to 1 g in 24 hours or 11 g over a course of treatment have been used.
IM Self-administrationFor self-administration using a prefilled auto-injector (e.g., AtroPen), dose is based on body weight and symptom severity.
Mild symptoms include miosis, blurred vision, tearing, runny nose, hypersalivation, drooling, wheezing, muscle fasciculations, nausea/vomiting.
Severe symptoms include behavioral changes, severe breathing difficulty, severe respiratory secretions, severe muscle twitching, involuntary defecation or urination, seizures, unconsciousness.
Adults >41 kg: Inject 2 mg IM initially for mild symptoms. If severe symptoms develop, inject 2 additional 2-mg IM doses in rapid succession 10 minutes after the initial dose.
Adults >41 kg who present with severe symptoms or are unconscious: Inject three 2-mg IM doses in rapid succession.
Additional doses (i.e., >3) should only be administered under the supervision of trained medical personnel.
Adults <41 kg: Pediatric doses can be used. (See Pediatric Patients: Pesticide Poisoning, under Dosage.)
Carbamate Anticholinesterase Pesticides
Carbamate poisoning is treated with the same doses of atropine sulfate as for organophosphate poisoning and IM self-administration can be employed when necessary. (See Organophosphate Anticholinesterase Pesticides under Dosage.)
Concomitant cholinesterase reactivator (pralidoxime chloride) therapy may not be necessary and atropine therapy generally is less prolonged (e.g., only 1 or 2 days) and symptoms usually do not recur once asymptomatic.
Chemical Warfare Agent Poisoning
Various doses and dosing intervals have been recommended; dosage requirements are based on severity of poisoning and individual patient response.
Organophosphate Anticholinesterase Nerve Agents
Administered IM in out-of-hospital setting or emergency department.
A cholinesterase reactivator (pralidoxime chloride) is administered concomitantly.
Give diazepam for seizure control.
Total atropine sulfate doses usually are much less than those required for organophosphate anticholinesterase pesticide poisoning.
IMMild to moderate symptoms: Usual initial IM dose is 2–4 mg.
Severe symptoms: 5–6 mg.
Frail geriatric patients with mild to moderate symptoms: 1 mg.
Frail geriatric patients with severe symptoms: 2–4 mg.
Repeat doses every 2–10 minutes as needed until muscarinic toxicity resolves (e.g., secretions have diminished and breathing is comfortable or airway resistance has returned to near normal).
Up to 15–20 mg may be required within the first 3 hours, but most patients respond to <20 mg usually during the initial 24 hours. In a report of sarin poisoning, <20% of moderately symptomatic patients required more than 2 mg. Pralidoxime chloride is administered concomitantly with atropine.
IM Self-administrationFor self-administration using a prefilled auto-injector (e.g., AtroPen), dose is based on body weight and symptom severity.
Mild symptoms include miosis, blurred vision, tearing, runny nose, hypersalivation, drooling, wheezing, muscle fasciculations, nausea/vomiting.
Severe symptoms include behavioral changes, severe breathing difficulty, severe respiratory secretions, severe muscle twitching, involuntary defecation or urination, seizures, unconsciousness.
Adults >41 kg: Inject 2 mg IM initially for mild symptoms. If severe symptoms develop, inject 2 additional 2-mg IM doses in rapid succession 10 minutes after the initial dose.
Adults >41 kg who present with severe symptoms or are unconscious: Inject three 2-mg IM doses in rapid succession.
Additional doses (i.e., >3) may be given every 5–10 minutes but only under the supervision of trained medical personnel.
Adults <41 kg: Pediatric doses can be used. (See Pediatric Patients: Pesticide Poisoning, under Dosage.)
Mushroom Poisoning
Muscarine-containing Clitocybes and Inocybes
IVIf needed for severe symptoms, 1–2 mg IV (minimum of 0.1 mg), repeated and titrated as needed according to response.
Radiographic Uses
Hypotonic Radiograph of the GI Tract
IMUsual dose is 1 mg.
Prescribing Limits
Pediatric Patients
PALS and Bradyarrhythmias
Bradycardia
IV, IO†, or EndotrachealInfants and children: AHA recommends maximum single dose of 0.5 mg.
Adults
ACLS and Bradyarrhythmias
Asystole, PEA, and Bradycardia
IVMaximum total dose of 3 mg recommended.
Special Populations
Hepatic Impairment
No specific hepatic dosage recommendations.
Renal Impairment
No specific renal dosage recommendations.
Geriatric Patients
Similar response between geriatric and younger patients. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Cautions for Atropine
Contraindications
-
No absolute contraindications to use in life-threatening conditions (e.g., poisoning by organophosphate nerve agents and pesticides).
-
Relative contraindications include:
-
known hypersensitivity to atropine or any ingredient in the formulation
-
angle-closure glaucoma
-
obstructive uropathy (e.g., bladder neck obstruction secondary to prostatic hypertrophy)
-
obstructive GI disease (e.g., pyloroduodenal stenosis, achalasia)
-
paralytic ileus
-
intestinal atony (especially in geriatric and debilitated patients)
-
severe ulcerative colitis
-
toxic megacolon
-
tachycardia secondary to cardiac insufficiency or thyrotoxicosis
-
acute hemorrhage when cardiovascular status is unstable
-
myasthenia gravis (unless used to reduce adverse muscarinic effects of an anticholinesterase agent such as neostigmine)
-
Warnings/Precautions
Warnings
Overdosage
Avoid overdosage, especially with IV administration.
Pediatric patients are particularly susceptible to overdosage.
Pesticide and Chemical Warfare Agent Poisoning
Use in patients with a history of anaphylactic reaction to atropine and mildly symptomatic organophosphate pesticide or nerve agent poisoning only when there is adequate medical supervision.
Severe breathing difficulty requires artificial respiration because atropine alone is not dependable in reversing respiratory muscle weakness or paralysis.
Administer with extreme caution when the symptoms of nerve agent poisoning are less severe in patients with disorders of heart rhythm (e.g., atrial flutter), substantial renal insufficiency, or a recent MI.
No more than 3 doses should be self-administered IM; additional doses require medical supervision.
Sensitivity Reactions
Parabens present in multiple-dose preparations may cause hypersensitivity reactions.
Hypersensitivity reactions may occasionally occur; usually skin rashes that may progress to exfoliation.
Major Toxicities
Cardiovascular Effects
Caution in patients with cardiac disease. Because heart rate is a major determinant of myocardial oxygen requirements, excessive rate acceleration in patients with acute myocardial ischemia or infarction may worsen ischemia or increase extent of infarction.
CNS Disturbances
Large or toxic doses or usual doses in patients with excess susceptibility may produce marked CNS disturbances (e.g., ranging from marked excitement, ataxia, hallucination, depression, and/or disorientation to active delirium to coma to death [secondary to respiratory failure]).
Marked somnolence in susceptible patients.
Mental confusion and/or excitement, especially in geriatric patients.
GI Disturbances
Extreme caution in known or suspected GI infections because of decreased GI motility and retention of causative organism and/or toxins.
Extreme caution in mild to moderate ulcerative colitis because of suppressed intestinal motility and resultant paralytic ileus and toxic megacolon.
Extreme caution in diarrhea (especially in patients with ileostomy or colostomy) because it may be an early sign of intestinal obstruction.
Caution in gastric ulcer because of delayed gastric emptying and possible antral stasis.
Caution in esophageal reflux and hiatal hernia because of decreased gastric motility and lower esophageal sphincter pressure leading to gastric retention and reflux aggravation.
GU Disturbances
Extreme caution in patients with partial obstructive uropathy because of decreased tone and amplitude of contractions of ureters and bladder and resultant urinary retention. (See Contraindications under Cautions)
Respiratory Effects
Caution with systemically administered atropine in debilitated patients with chronic pulmonary disease because a reduction in bronchial secretions may lead to inspissation and formation of bronchial plugs; however, has been used effectively as bronchodilator when administered via oral inhalation.
Thermoregulatory Effects
Exposure to high environmental temperatures may result in heat prostration due to decreased sweating. Increased risk of hyperthermia in patients who are febrile.
General Precautions
Neuropathy
Extreme caution in patients with autonomic neuropathy.
Down’s Syndrome, Spastic Paralysis, and Brain Damage
Increased sensitivity to antimuscarinic effects (e.g., mydriasis, positive chronotropic effect).
Hypertension
Caution in hypertensive patients.
Hyperthyroidism
Caution in hyperthyroid patients.
Seizure Management in Anticholinesterase Poisoning
Use barbiturates cautiously to manage seizures because the drugs are potentiated by anticholinesterases. Diazepam is preferred for seizure control.
Specific Populations
Pregnancy
Category C.
Lactation
Atropine is found in human milk in trace amounts; use caution when administered to a nursing woman.
Pediatric Use
Safety and efficacy in the setting of organophosphate pesticide poisoning established in children of all ages.
Increased susceptibility to the effects of atropine. More susceptible than adults to toxic effects; deaths at doses as low as 10 mg.
Infants, patients with Down’s syndrome (mongolism), and children with spastic paralysis or brain damage may be hypersensitive to antimuscarinic effects (e.g., mydriasis, positive chronotropic effect).
Geriatric Use
Increased susceptibility to the effects of atropine. Mental confusion and/or excitement are especially likely in geriatric patients.
Hepatic Impairment
Use with caution in hepatic disease.
Renal Impairment
Use with caution in renal disease.
Common Adverse Effects
Most adverse effects are manifestations of pharmacologic effects at muscarinic-cholinergic receptors and usually are reversible when therapy is discontinued.
Severity and frequency of adverse effects are dose related and individual intolerance varies greatly; adverse effects occasionally may be obviated by a reduction in dosage but this also may eliminate potential therapeutic effects.
Frequent effects include xerostomia (dry mouth), dry skin, blurred vision, cycloplegia, mydriasis, photophobia, anhidrosis, urinary hesitancy and retention, tachycardia, palpitation, xerophthalmia, and constipation, which may appear at therapeutic or subtherapeutic doses. In many patients, xerostomia is the dose-limiting effect.
Other common effects include increased ocular tension (especially in patients with angle-closure glaucoma), loss of taste, headache, nervousness, restlessness, drowsiness, weakness, dizziness, flushing, insomnia, nausea, vomiting, bloated feeling, anhidrosis (especially in hot environments), mild to moderate pain at the injection site, loss of libido, and erectile dysfunction (via block of cholinergically mediated vasodilation).
Drug Interactions
Drugs with Anticholinergic Effects
Additive adverse effects resulting from cholinergic blockade (e.g., xerostomia, blurred vision, constipation). Advise of possibility of increased anticholinergic effects and monitor carefully.
Effects on GI Absorption of Drugs
By inhibiting the motility of the GI tract and prolonging GI transit time, antimuscarinics have the potential to alter GI absorption of various drugs.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Amantadine |
Increased anticholinergic effects |
Inform patient and monitor carefully |
|
Antacids |
Decreased GI absorption of atropine |
Administer oral atropine at least 1 hour before antacids |
|
Anticholinergic drugs |
Increased anticholinergic effects |
Inform patient and monitor carefully |
|
Antihistamines (anticholinergic) |
Increased anticholinergic effects |
Inform patient and monitor carefully |
|
Antiparkinsonian (antimuscarinic) agents |
Increased anticholinergic effects |
Inform patient and monitor carefully |
|
Corticosteroids |
Increased IOP |
Caution; monitor IOP |
|
Digoxin (slow dissolving) |
Increased serum digoxin |
Use digoxin oral solution (elixir) or rapidly dissolving tablets (e.g., Lanoxin) |
|
Disopyramide |
Increased anticholinergic effects |
Inform patient and monitor carefully |
|
Ketoconazole |
Increased gastric pH decreases ketoconazole absorption |
Administer atropine at least 2 hours after ketoconazole |
|
Levodopa |
Increased GI metabolism of levodopa & decreased systemic concentrations |
Adjust levodopa dosage if atropine is started or discontinued |
|
Meperidine |
Increased anticholinergic effects |
Inform patient and monitor carefully |
|
Mexiletine |
Decreased GI absorption rate of mexiletine; no effect on bioavailability |
|
|
Muscle (anticholinergic) relaxants |
Increased anticholinergic effects |
Inform patient and monitor carefully |
|
Phenothiazines |
Increased anticholinergic effects |
Inform patient and monitor carefully |
|
Potassium chloride |
Slowed GI transit potentiates adverse GI effects of oral potassium chloride (especially wax-matrix tablets) |
Caution if used concomitantly; monitor for possible GI mucosal lesions |
|
Procainamide |
Increased anticholinergic effects |
Inform patient and monitor carefully |
|
Pralidoxime |
Increased rate of atropinization |
|
|
Tricyclic antidepressants |
Increased anticholinergic effects |
Inform patient and monitor carefully |
Atropine Pharmacokinetics
Absorption
Bioavailability
Well absorbed (90%) from the GI tract, principally from upper small intestine.
Rapidly and well absorbed after IM injection. Physical exercise, either prior to or immediately following IM injection, increases absorption due to muscle perfusion and decreases clearance.
Well absorbed following endotracheal administration. Dilution with sterile water versus 0.9% sodium chloride injection may increase endotracheal absorption.
Onset
Inhibition of salivation occurs within 30 minutes and peaks within 1–1.6 hours after IM administration.
Increase in heart rate occurs within 2–4 minutes after IV injection.
Increase in heart rate occurs within 5–40 minutes and peaks within 20–60 minutes after IM administration.
Duration
Inhibition of salivation persists for up to 4 hours.
Plasma Concentrations
Following IM administration, peak plasma concentrations are reached within 30 minutes.
Distribution
Extent
Rapidly and well distributed throughout the body, including the CNS.
Traces are found in various secretions, including milk.
Crosses the placental barrier and enters fetal circulation but is not found in amniotic fluid.
Plasma Protein Binding
Low binding (about 18%) to serum albumin.
Elimination
Metabolism
Via the liver to several metabolites including tropic acid, atropine (or a chromatographically similar compound), and, possibly, esters of tropic acid and glucuronide conjugates.
Elimination Route
About 30–50% of a dose is excreted in urine unchanged.
Excreted mainly through the kidneys; however, small amounts may be excreted in the feces and expired air.
Half-life
2–3 hours.
Biphasic following IM injection; 2–3-hours initially followed by a terminal half-life of 12.5 hours or longer.
Special Populations
Elimination half-life is more than doubled in children <2 years and the elderly (>65 years of age) compared with other age groups.
No gender effect on pharmacokinetics and pharmacodynamics.
Stability
Storage
Parenteral
Injection
25°C (may be exposed to 15–30°C).
Protect from freezing and light.
Actions
-
Competitively inhibits acetylcholine or other cholinergic stimuli at autonomic effectors innervated by postganglionic cholinergic nerves and, to a lesser extent, on smooth muscles that lack cholinergic innervation. At usual doses, principally antagonizes cholinergic stimuli at muscarinic receptors and has little or no effect on cholinergic stimuli at nicotinic receptors.
-
Antimuscarinics also have been referred to as anticholinergics (cholinergic blocking agents), but this term is appropriate only when it describes the antagonism of cholinergic stimuli at any cholinergic receptor, whether muscarinic or nicotinic.
-
Also have been referred to as parasympatholytics because the antagonized functions principally are under the parasympathetic division of the nervous system.
-
Receptors at various sites are not equally sensitive to inhibition of muscarinic effects. Relative sensitivity of physiologic functions (proceeding from the most sensitive) is as follows: secretions of the salivary, bronchial, and sweat glands; pupillary dilation, ocular accommodation, and heart rate; contraction of the detrusor muscle of the bladder and smooth muscle of the GI tract; and gastric secretion and motility. Doses used to decrease gastric secretions are likely to cause dryness of the mouth (xerostomia) and interfere with visual accommodation, and possibly cause difficulty in urinating.
-
Various antisecretory effects in the GI tract, including reduction of salivation (producing xerostomia) and gastric secretions (only partial reduction in gastric acid secretion). Prolonged inhibitory effects on the motility of the esophagus, stomach, duodenum, jejunum, ileum, and colon.
-
Relaxes lower esophageal sphincter with a resultant decrease in lower esophageal sphincter pressure.
-
Decreases the tone and amplitude of contractions of the ureters and bladder. May cause urinary retention (e.g., in patients with urinary obstruction). In patients with uninhibited or reflex neurogenic bladder, the amplitude and frequency of uninhibited contractions are reduced and bladder capacity is increased.
-
Positive chronotropic effect (increased SA node automaticity), accelerating sinus rate by direct parasympathetic blockade. Stimulates the AV functional pacemaker. Facilitates AV nodal conduction in a normal AV node.
-
Can reverse reflex vagal cardiac slowing or asystole such as that induced by inhalation of irritant vapors or by vagal stimulation (e.g., carotid sinus stimulation, pressure on the eyeball).
-
May cause cutaneous vasodilation, especially at toxic doses (atropine flush).
-
Reduces secretions from the nose, mouth, pharynx, and bronchi. Relaxes smooth muscles of the bronchi and bronchioles with a resultant decrease in airway resistance. Potent bronchodilation, particularly in large bronchial airways; especially effective in reversing bronchoconstriction induced by parasympathetic stimulation.
-
Stimulates the medulla and higher cerebral centers and exhibits CNS effects similar to those produced by antimuscarinics used in the treatment of parkinsonian syndrome (e.g., trihexyphenidyl).
-
Blocks the responses of the sphincter muscle of the iris and the ciliary muscle of the lens to cholinergic stimulation, producing mydriasis and cycloplegia and a resultant decrease in ocular accommodation. Little effect on IOP except with angle-closure glaucoma where IOP may increase.
-
Reduces the volume of perspiration by inhibiting sweat-gland secretions. May suppress sweating sufficiently to increase body temperature.
Advice to Patients
-
Seek immediate medical attention after injection with an atropine injection auto-injector.
-
Advise that dry mouth may occur.
-
Advise of risk of hyperthermia and heat prostration; avoid exposure to high environmental temperatures and avoid use when febrile.
-
Advise patients receiving chronic therapy of possible blurred vision with the drug; activities that require good, clear vision should be avoided.
-
Risk of dizziness or drowsiness; avoid driving or operating machinery until effects on individual are known.
-
For IM self-administration in nerve gas and pesticide poisoning, proper techniques for storage, attention to expiration dating (replacing before expiration), use, and disposal of the prefilled auto-injector (e.g., AtroPen) and for administration of the drug.
-
For IM self-administration in nerve gas and pesticide poisoning, importance of understanding the indications for use and the symptoms of poisoning.
-
For IM self-administration in nerve gas and pesticide poisoning, importance of ensuring adequate understanding of the recognition and treatment of such poisoning and when concomitant cholinesterase reactivator (pralidoxime chloride) therapy may be necessary.
-
For IM self-administration in nerve gas and pesticide poisoning, importance of not exceeding 3 doses unless under medical supervision.
-
For IM self-administration in nerve gas and pesticide poisoning, importance of seeking immediate medical attention once the initial dose(s) is administered because respiratory and other supportive care and prolonged atropinization may be needed.
-
For IM self-administration in nerve gas and pesticide poisoning, importance of recognizing that inadvertent administration when such poisoning is not present could result in atropine toxicity and temporary incapacitation (inability to walk properly, see clearly, or think clearly for several hours or longer).
-
For self-administration in nerve gas and pesticide poisoning, importance of not contaminating other individuals (e.g., medical and emergency personnel) by clothing exposure; aggressive and safe decontamination by trained personnel is strongly suggested.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
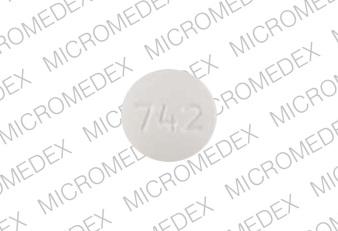
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Bulk |
Powder |
|||
|
Parenteral |
Injection |
equivalent to Atropine Sulfate 0.25 mg/0.3 mL |
AtroPen Auto-Injector (“yellow label”) |
Meridian |
|
equivalent to Atropine Sulfate 0.5 mg/0.7 mL |
AtroPenAuto-Injector (“blue label”) |
Meridian |
||
|
equivalent to Atropine Sulfate 1 mg/0.7 mL |
AtroPenAuto-Injector (“dark red label”) |
Meridian |
||
|
equivalent to Atropine Sulfate 2 mg/0.7 mL |
AtroPenAuto-Injector (“green label”) |
Meridian |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Bulk |
Powder* |
|||
|
Parenteral |
Injection |
0.05 mg/mL* |
Atropine Sulfate Injection |
|
|
0.1 mg/mL* |
Atropine Sulfate Injection |
|||
|
0.4 mg/mL* |
Atropine Sulfate Injection |
|||
|
1 mg/mL* |
Atropine Sulfate Injection |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions April 24, 2017. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
More about atropine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
- Latest FDA alerts (3)
- Side effects
- Dosage information
- During pregnancy
- Drug class: anticholinergic chronotropic agents
- Breastfeeding
- En español