Tracheotomy
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
A tracheotomy is surgery to help you breathe through an opening in your trachea.
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) for any of the following:
- Your trach tube falls out and you cannot get it back in. This is an emergency. Call for an ambulance to take you to the nearest hospital. Do not drive yourself.
- You are coughing up blood.
- You are very short of breath, and coughing and suctioning does not help.
- You have sudden chest pain.
- You start bleeding from your incision.
Call your doctor or surgeon if:
- You have an increased amount of mucus, or it is very thick.
- You have chills, a cough, or feel weak and achy.
- You have pain in your neck that does not go away or gets worse.
- You have trouble swallowing.
- Your incision is swollen, red, or has pus coming from it.
- You have questions or concerns about your condition or care.
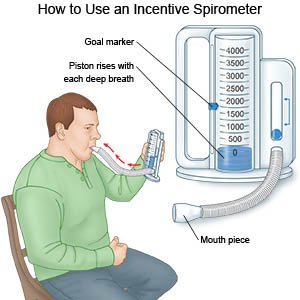
Deep breathing and coughing
may help prevent a lung infection. Take deep breaths and cough 10 times each hour. Take a deep breath and hold it for as long as you can. Let the air out and cough strongly. Deep breaths help open your airway. You may be given an incentive spirometer to help you take deep breaths. Put the plastic piece in your mouth and take a slow, deep breath. Then let the air out and cough. Repeat these steps 10 times every hour.
 |
Suction
may be needed to remove any mucus you have trouble getting out of the trach tube. This is done by putting a plastic suction tube down into your trach tube to get the mucus out.
Nutrition:
Follow your healthcare provider's instructions on what you can eat after you leave the hospital. To decrease the risk of food going into your trachea, keep your head raised while you eat. Ask your healthcare provider if you need to be on a special diet.
Mouth care:
Follow your healthcare provider's instructions on how to keep your mouth clean and moist.
Oxygen:
You may need extra oxygen to help you breathe easier. It may be given through your nose or through a plastic mask over your trach tube. Never smoke or let anyone else smoke around your oxygen. This can be very dangerous.
Speaking:
Healthcare providers will help you learn how to let others know what you need. You will learn how to adjust your trach tube so you can speak. You may need to release air from the plastic cuff around the trach tube in your neck. When you breathe out, air will pass through your vocal cords and allow you to speak in a whisper. You may also be given a one-way valve to help you speak.
Wound and tube care:
The hole in your neck and your trach tube must stay clean and dry to prevent infection. Your trach tube will have inner and outer tubes called cannulas. The inner cannula may need to be changed daily. Your healthcare provider will teach you how to care for your trach tube. If someone is helping you at home, make sure that person watches and learns.
Follow up with your doctor or surgeon as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
