Thoracotomy
Medically reviewed by Drugs.com. Last updated on May 6, 2024.
A thoracotomy is surgery to repair any damage to the blood vessels and organs inside your chest. These organs include your esophagus, heart, lungs, and trachea (windpipe). A thoracotomy is also done to remove a lung tumor or an abscess (infection with pus). It may also be done to remove air or blood trapped inside your chest.
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) if:
- You feel lightheaded, short of breath, or have chest pain.
- You cough up or vomit blood.
Seek care immediately if:
- You feel dizzy, or have trouble thinking or remembering things.
- Your heart is beating fast or out of rhythm.
- Blood soaks through your bandage.
- Your incision site is swollen, red, or has pus coming from it.
- Your stitches or staples come loose or fall out.
Call your doctor or surgeon if:
- You have a fever and shaking chills.
- You cough up yellow, green, or bloody sputum.
- Your skin is itchy, swollen, or you have a new rash.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Antibiotics help prevent or fight a bacterial infection.
- Heart medicine helps strengthen or regulate your heartbeat.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask if NSAIDs are safe for you. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Patient-controlled analgesia:
- You may get pain medicine from a pump. You can receive the pain medicine through an IV or an epidural line. This is called patient-controlled analgesia (PCA) or patient-controlled epidural analgesia (PCEA). Your healthcare providers set up the PCA pump to give you small amounts of pain medicine. The PCA pump has a cord coming from it, with a push button on the end. When you feel pain, you may push the button to give yourself pain medicine. To keep you from getting too much medicine, there is a limit on how often you can get the medicine.
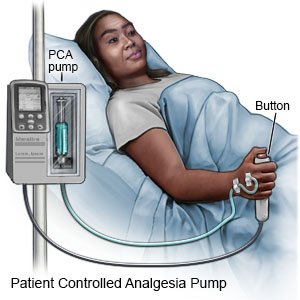
- Do not let anyone else push the button for you. Your pump may give you a constant dose of pain medicine, as well as the medicine that you give yourself. If your pain continues, even with the use of the PCA, let your healthcare provider know.
Prevent a lung infection:
- Deep breathing opens the tubes going to your lungs. Coughing helps to bring up sputum (mucus) from your lungs for you to spit out. Take a deep breath and hold the breath as long as you can. Push the air out of your lungs with a deep strong cough. Put any sputum that you have coughed up into a tissue. Take 10 deep breaths in a row every hour while you are awake. Remember to follow each deep breath with a cough. Hold a pillow tightly against your incision when you cough to help decrease the pain.
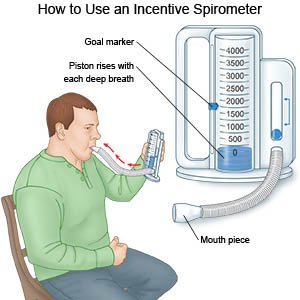
- You may need to use an incentive spirometer to help you take deeper breaths. Put the plastic piece into your mouth and take a very deep breath. Hold your breath as long as you can and then let out your breath. Ask your healthcare provider for information on how to use a spirometer.
Follow up with your doctor or surgeon as directed:
Ask when to return to have your surgery site checked. You may also need to have your chest drain, stitches, or staples removed. If you were given PCA medicine, ask when to return to have your IV or epidural line removed. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
