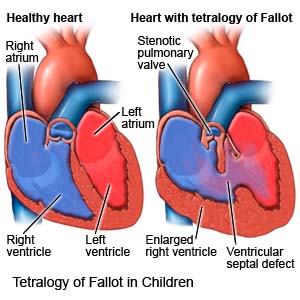
Tetralogy of Fallot in Children
Medically reviewed by Drugs.com. Last updated on Jun 2, 2025.
Tetralogy of Fallot (TOF) is a heart condition your child was born with. TOF causes the following 4 heart structure defects that lead to a weak heart and decreased blood flow:- A narrowed blood vessel that connects the heart to the lungs
- A hole in the wall that separates the heart
- Aorta (major artery) growth from both sides of the heart instead of from one side as normal
- Blood flow that backs up and causes the right side of the heart to enlarge and thicken
 |
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that your child may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your child's medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done to your child. Make sure all of your questions are answered.
Stay with your child for comfort and support
as often as possible while he or she is in the hospital. Ask another family member or someone close to the family to stay with your child when you cannot be there. Bring items from home that will comfort your child, such as a favorite blanket or toy.
Medicines:
- Antibiotics help prevent or treat a bacterial infection.
- Diuretics help your child's body get rid of extra fluid, which can help your child breathe easier. He or she may urinate more often with this medicine.
- Heart medicine helps your child's heart beat stronger or more regularly.
- An iron supplement may be given to prevent or treat anemia (low red blood cell count).
Tests:
- Blood tests may show how much oxygen is flowing through your child's blood.
- An EKG test records your child's heart rhythm and how fast his or her heart beats. It is used to check for heart enlargement and other problems with blood flow.
- A chest x-ray may show the shape of your child's heart and any enlargement from his or her condition.
- An echocardiogram is a type of ultrasound. Sound waves are used to show the structure and function of your child's heart.
- A Doppler test checks the blood flow in your child's heart. A small metal disc with gel is placed on your child's chest. Abnormal sounds may be heard when TOF is present.
- A cardiac catheterization may show the blood vessels in your child's heart and how well the heart is working. A catheter is threaded into your child's heart through a blood vessel in his or her arm, leg, or neck. Contrast dye is injected into an artery and x-rays of your child's blood flow are taken. Tell a healthcare provider if your child has ever had an allergic reaction to contrast dye.
Treatment:
- Extra oxygen may be needed if your child's blood oxygen level is lower than it should be. Oxygen will help your child breathe easier. Your child may get oxygen through small tubes placed in his or her nostrils, or through a mask.
- Surgery may be needed between ages 3 to 6 months to correct the 4 heart defects. This will improve blood flow from your child's heart and lungs to his or her body.
RISKS:
Your child's signs and symptoms may limit his or her ability to function in daily life. Without treatment, your child has an increased risk for endocarditis (swelling of the lining of the heart). Your child may also develop an abscess or blood clot. His or her signs and symptoms may get worse. His or her heart may weaken and stop working completely. This can be life-threatening.
CARE AGREEMENT:
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Tetralogy of Fallot
- Atorvastatin (Lipitor): Top 12 Drug Facts You Need to Know
- Do blood pressure drugs interact with alcohol?
- Side Effects of Weight Loss Drugs
Treatment options
Care guides
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
