Rigid Bronchoscopy
Medically reviewed by Drugs.com. Last updated on May 6, 2024.
What is a rigid bronchoscopy?
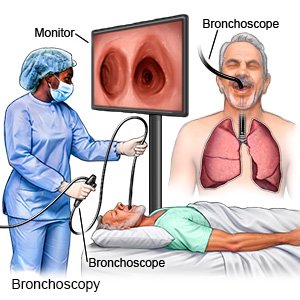
A rigid bronchoscopy is a procedure to look inside your respiratory system (nose, throat, and lungs). Healthcare providers use a bronchoscope. This is a firm tube with a light and camera on the end. Pictures of your respiratory system appear on a monitor during the procedure.
Why may I need a rigid bronchoscopy?
- A rigid bronchoscopy may help diagnose lung diseases, inflammation, cancer, or infections. You may need this procedure because you have blood in your spit, trouble breathing, or a severe cough. A biopsy may be done during a rigid bronchoscopy. This is when a small tissue sample is removed and sent to a lab for tests. You may also need lavage during this procedure. This is when a small amount of saline is used to wash parts of your airway and lungs. The cells that are rinsed off are collected and sent to a lab for tests.
- A rigid bronchoscopy may also be used to remove a foreign object or tumor that is blocking your airway. Your healthcare provider may insert tools, such as a laser, probe, needle, or suction device, through the scope. These are used to heat or freeze tissues or suction out mucus plugs or blood clots. They may also be used to stop bleeding or to place a stent (tube) or balloon to widen your airway.
How do I prepare for a rigid bronchoscopy?
- Do not eat or drink anything for 6 to 12 hours before your procedure.
- Do not take aspirin, ibuprofen, or other blood thinning medicines before your procedure. Ask your healthcare provider when you should stop taking these medicines.
- Have someone with you to drive you home.
What happens during a rigid bronchoscopy?
- Your healthcare provider will give you medicine to numb your throat, help you relax, or stop coughing or gagging. He or she will place a mouthguard to help protect your teeth.
- Your healthcare provider will gently pass the scope through your nose or mouth and into your airway. He or she will examine each part that the scope passes. Your provider may take pictures of the inside of your airway. He or she may also take samples or remove tissues that may be causing your symptoms.
 |
What are the risks of a rigid bronchoscopy?
Your heartbeat may slow down and your blood pressure may decrease. This can cause you to sweat and faint. The scope may make a hole or tear in your airway. You may get an infection after the procedure. The space between your lungs and chest may fill with air or blood. These problems can be life-threatening.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
