Rabies
Medically reviewed by Drugs.com. Last updated on Jun 30, 2025.
What is rabies?
Rabies is a disease that affects the body's central nervous system (brain, spinal cord, and nerves). Rabies is caused by a virus. You may get the virus if you come into contact with the saliva or other tissue of an infected animal. Rabies infection usually happens through a bite wound. Animals that may spread rabies include dogs, cats, coyotes, raccoons, foxes, skunks, and bats. Rabies develops when the virus enters the skin and goes to the muscles or nerves. Without early treatment, rabies damages the brain and other organs. You may have brain swelling, seizures, and paralysis. Rabies can be life-threatening.
What increases my risk for rabies?
Rabies can affect anyone, at any age. The following may increase your risk:
- You were bitten on the head, face, neck, or hands. Even a small bite from a bat can increase your risk for rabies.
- You were bitten many times during an attack, or you have deep bite wounds.
- You have a weak immune system from medicine such as steroids or a disease such as HIV/AIDS.
- You travel to places where rabies is common.
- You have a job that includes handling the virus or working with animals. These jobs include laboratory workers, veterinarians, forest rangers, and animal control and wildlife workers.
What are the early signs and symptoms of rabies?
Signs and symptoms of rabies may appear weeks, months, or even years after the infection. During the early stages of rabies, you may feel like you have the flu. You may have one or more of the following for up to 10 days:
- Weakness, fever, headache, and irritability
- Loss of appetite, nausea, and vomiting
- Pain, numbness, or burning or tingling that may slowly spread to other areas
- Severe itching at the bite site
What are the late signs and symptoms of rabies?
Over time, rabies may affect the brain. You may have any of the following:
- Confusion or insomnia
- Dizziness, seeing double, or seeing something that is not really there
- Restlessness, anxiety, and hyperactivity increased by thirst, fear, light, or noise
- Seizures or twitching
- Slurred speech, drooling, swallowing problems, and a fear of water
- Tiredness, muscle cramps, or trouble moving
- Severe weakness that may be only on one side of your body or face
 |
How is rabies diagnosed?
Your healthcare provider will ask if you have been bitten by an animal and how the animal behaved before it bit you. He or she will ask about vaccinations you have received, and your past travels. You may need any of the following tests:
- Blood tests are done to look for antibodies to the rabies virus. Antibodies are substances that the immune system makes to protect the body from outside organisms. You may need to have blood drawn more than 1 time.
- A biopsy is done to remove a small piece of skin to be tested for the cause of your symptoms. A skin sample is usually taken from the back of the neck.
- Cultures are done to test your saliva, tears, or the fluid around your brain and spinal cord.
- A lumbar puncture , or spinal tap, may be done to check the fluid around your brain and spinal cord for the rabies virus.
- A CT or MRI may be used to check for signs of swelling or infection in your brain.
How is rabies treated?
The main goal of treatment is to prevent the virus from spreading inside the body. Treatment as soon as possible may prevent more serious problems and increase recovery.
- You may need to get the rabies vaccine. The rabies vaccine helps your body make antibodies to fight the virus. You will be given 2 doses if you received at least 1 dose before. You will be given 4 doses over 2 weeks if you never received a dose. You may be given 5 doses if you never received a dose and you have a weak immune system.
- Rabies immune globulin (RIG) may be given. This medicine will attack the virus and help your immune system fight the infection. RIG is usually given on the day you receive the first vaccine dose, or soon after.
What can I do to prevent rabies?
- Ask your healthcare provider about the rabies vaccine. You may need the vaccine if your risk for rabies is increased through work or travel. You will be given 2 doses a week apart. You may need a booster dose within 3 years after the first 2 doses.
- Avoid contact with animals. Do not approach any wild animal, or any tame animal that you do not know. Cover windows and other openings in your home with screens so wild animals cannot get inside.
- Get medical care if you get bitten by an animal. Do this even if the wound is very small.
- Get your pet vaccinated against rabies. You will need to do this every 3 years or as directed by your veterinarian.
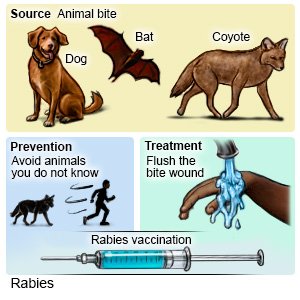 |
What should I do if an animal that can carry rabies bites me?
- Clean the bite wound. Clean the bite wound for at least 5 minutes. Use soap and water, or povidone-iodine solution mixed with water. Do this right after you are bitten to lower the risks for a wound infection and rabies. Cover the wound with a clean bandage to prevent infection.
- Seek care right away. Healthcare providers may need to treat the wound and close it with stitches. You may need to take antibiotics to help fight or treat a bacterial infection. The rabies vaccine series may be started immediately.
Call your local emergency number (911 in the US) or have someone else call if:
- You have trouble swallowing or slurred speech.
- You have double vision, or you see things that are not really there.
- You begin twitching, have muscle cramps, or have a seizure.
When should I seek immediate care?
- You think you were exposed to rabies.
- You were bitten by an animal. Clean the wound as soon after the bite as possible.
- You feel weak, tired, dizzy, confused, restless, or anxious.
When should I call my doctor?
- You have a fever.
- Your signs and symptoms do not get better after treatment.
- You have questions or concerns about rabies and rabies treatment.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Rabies
Treatment options
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
