Spinal Cord Injury
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
What do I need to know about a spinal cord injury (SCI)?
Your spinal cord is protected by vertebrae that make up the spinal column. An SCI can happen if your spinal column presses down on or pinches your spinal cord. This causes swelling or bruising of your spinal cord. Damage to your spinal column, disease, or infection can cause an injury to your spinal cord. An SCI is referred to by a letter and a number. The letter represents the spinal column level where the injury occurred. The number represents which vertebrae is involved.
What do I need to know about the spinal column levels?
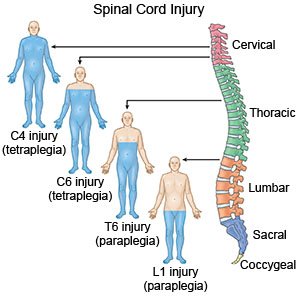
The spinal column usually has about 30 vertebrae. The column is divided into levels:
- The cervical (C) region includes the 8 vertebrae (C1 to C8) that form the neck.
- The thoracic (T) region includes the 12 vertebrae (T1 to T12) that form the upper to middle back.
- The lumbar (L) region includes the 5 vertebrae (L1 to L5) that form the lower back.
- The sacral (S) region includes the 5 vertebrae (S1 to S5) between the lumbar region and the tailbone.
 |
What are the types of SCI?
An SCI may occur at any level. You have an incomplete injury if you have some feeling or movement below the level of injury. You have a complete injury if you have no movement or feeling below the level of injury.
- Tetraplegia usually happens at a level from C1 to T1. You may not have any feeling or movement of your arms and legs. You also may not be able to move your head and neck. This may also be called quadriplegia.
- Paraplegia usually happens at a level from T2 to S5. You may have a loss of feeling or movement in your chest, stomach, hips, legs and feet.
How is an SCI diagnosed?
Your healthcare provider will do tests to see if you have any movement or feeling in your arms and legs. You may also need tests such as MRI, CT, or x-ray, to show any damage to your spinal cord. You may be given contrast material to help show the damage to your spinal cord better. Tell your healthcare providers if have ever had an allergic reaction to contrast material.
What is the immediate treatment for an SCI?
You may have to be put in a firm brace or have traction to your spine. The brace and traction are used to prevent movement of your spinal column. Movement of your spinal column may cause more damage to your spinal cord. You may also need medicines to keep you from moving. You may need a ventilator to help you breathe if your injury affects your lungs or diaphragm. You may need surgery to remove the part of your spinal column that is damaging or blocking your spinal cord.
What health problems are common with an SCI?
These complications can become life-threatening:
- Pressure injuries (bedsores)
- Deep vein thrombosis
- Hyperreflexia caused by an irritant to nerves below the level of injury
- Lung conditions such as pneumonia, pulmonary blood clots, or a collapsed lung
Why is rehabilitation after an SCI important?
You will begin rehabilitation after your hospitalization. The goal of rehabilitation is to help you function with an SCI. The rehabilitation team includes the following:
- A doctor who specializes in physical medicine and rehabilitation
- Physical therapists who teach you exercises to build strength and use of adaptive devices, such as a wheelchair
- Occupational therapists who teach you how to do activities of daily living, such as grooming and toileting routines
- Rehabilitation psychologists who help you cope emotionally with your SCI
- Rehabilitation nurses, dietitians, social workers, and other specialists who monitor your condition
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Spinal Cord Injury
Treatment options
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
