Pneumonia
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
Pneumonia is an infection in your lungs caused by bacteria, viruses, fungi, or parasites. You can become infected if you come in contact with someone who is sick. You can get pneumonia if you recently had surgery or needed a ventilator to help you breathe. Pneumonia can also be caused by accidentally inhaling saliva or small pieces of food. Pneumonia may cause mild symptoms, or it can be severe and life-threatening.
 |
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
An IV
is a small tube placed in your vein that is used to give you medicine or liquids.
Medicines:
- Antibiotics are given to treat a bacterial infection.
- Acetaminophen and ibuprofen decrease fever and pain.
Tests:
- Blood tests may show signs of an infection or the bacteria causing your pneumonia. Blood tests can also show how much oxygen is in your blood.
- A chest x-ray may show signs of infection in your lungs.
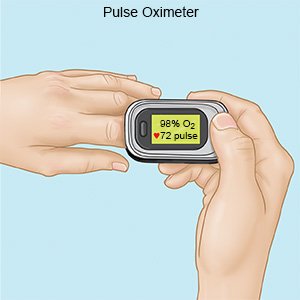
- Pulse oximetry measures the amount of oxygen in your blood.
- A mucus sample is collected and tested for the germ that is causing your illness. It can help your healthcare provider choose the best medicine to treat the infection.
Treatment:
- Airway clearance techniques are exercises to help remove mucus so you can breathe more easily. Your healthcare provider will show you how to do the exercises. These exercises may be used along with machines or devices to help decrease your symptoms.
- Respiratory support is given to help you breathe. You may receive oxygen to increase the level of oxygen in your blood. You may also need a machine to help you breathe.
- Breathing treatments may be needed to help open your airways so you can breathe easier. A machine may be used to help you breathe in medicine.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
RISKS:
Pneumonia increases your risk for breathing problems. The infection can spread to other areas of your body. Pus or extra fluid may pool in the space around your lungs. You may not be able to get enough oxygen if your lungs are inflamed or damaged. Low oxygen levels can damage other organs, such as your kidneys, heart, and brain.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Pneumonia
Treatment options
Care guides
- Aspiration Pneumonia
- Bacterial Pneumonia
- Community Acquired Pneumonia
- Hospital Acquired Pneumonia
- Pneumonia
- Pontiac Fever
- Viral Pneumonia
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
