Pertussis in Children
Medically reviewed by Drugs.com. Last updated on Jun 30, 2025.
Pertussis, or whooping cough, is an infection of the nose, throat, and lungs. Your child's air passages narrow and get plugged with thick mucus. This may cause him or her to have coughing spells. Anyone can have pertussis, but it is most serious in babies and young children. A baby may get pertussis before he or she is old enough to get the shots to prevent the infection. Pertussis is caused by bacteria. It is easily spread in the air when someone with pertussis coughs or sneezes.
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) if:
- Your child has more severe coughing spells.
- Your child is short of breath or works hard to breathe.
- The skin between his or her ribs or above his or her breastbone pulls in with each breath.
- Your child's nostrils are flaring with each breath.
Call your child's pediatrician if:
- Your child's lips or fingernails are blue or white.
- Your child has been vomiting and cannot keep anything down.
- Your child has the following signs of dehydration:
- Crying without tears
- Dry mouth or tongue
- Fussiness, sleepiness, or dizziness
- Sunken soft spot on the top of his or her head (if your baby is younger than 1 year)
- Urinating less than usual
- Wrinkled skin
- Your child has a fever.
- Your child is not drinking liquids.
- Your child's cough is getting worse.
- Your child is tugging his or her ears or has ear pain.
- Your child is not sleeping or resting because of the cough.
- You have questions or concerns about your child's condition or care.
Medicines:
Your child may need any of the following:
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If your child takes blood thinner medicine, always ask if NSAIDs are safe for him or her. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to give your child and how often to give it. Follow directions. Read the labels of all other medicines your child uses to see if they also contain acetaminophen, or ask your child's doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Antibiotics help treat or prevent a bacterial infection.
- Do not give aspirin to children younger than 18 years. Your child could develop Reye syndrome if he or she has the flu or a fever and takes aspirin. Reye syndrome can cause life-threatening brain and liver damage. Check your child's medicine labels for aspirin or salicylates.
- Give your child's medicine as directed. Contact your child's healthcare provider if you think the medicine is not working as expected. Tell the provider if your child is allergic to any medicine. Keep a current list of the medicines, vitamins, and herbs your child takes. Include the amounts, and when, how, and why they are taken. Bring the list or the medicines in their containers to follow-up visits. Carry your child's medicine list with you in case of an emergency.
Manage your child's symptoms:
Your child's cough may last 10 weeks or longer. It may be worse at night. Coughing helps keep mucus from clogging his or her lungs. Any of the following may help your child:
- Wash hands often. Help your child wash his or her hands after he or she coughs, sneezes, or uses the bathroom. Also wash your hands after changing diapers and before preparing or eating food.

- Help your child during a coughing spell. If your child has a coughing spell, put him or her on his or her side in the crib or bed. This is a safe position because it will keep your child from choking if he or she vomits. You may also hold your child in a sitting position during a coughing spell. Help your coughing child sit up and lean forward if he or she is older. This makes it easier to cough and bring up mucus from the lungs.
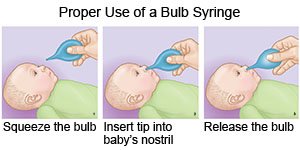
- Help keep your baby's airways clear. Use a bulb syringe to gently clean your baby's nose. Wash the bulb syringe after each use. Clean your baby's nose before breast or bottle feeding so he or she can breathe easier while feeding. You may need to feed your baby smaller amounts more often if he or she gets tired during feedings. Clean your baby's nose before you put him or her down to sleep.
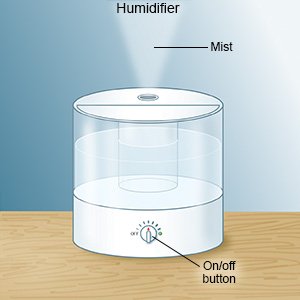
- Use a cool mist humidifier to increase air moisture in your home. This may make it easier for your child to breathe and help decrease his or her cough.
- Give your child liquids as directed. Ask how much liquid to give him or her each day and what liquids are best for him or her. You may need to give him or her small amounts of liquid every hour when he or she is awake. This will help prevent dehydration. Good liquids to drink are water or fruit juices. Limit caffeine.
- Give your child small, healthy meals often. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Healthy foods may give him or her energy and help him or her feel better.
- Help your child rest as much as possible until he or she begins to feel better.
- Do not smoke around your child or let anyone smoke around him or her. His or her breathing and coughing may get worse if he or she is near smoke.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Prevent the spread of pertussis:
- Help protect others from pertussis. Do not let your child go to school or daycare until his or her healthcare provider says it is okay.
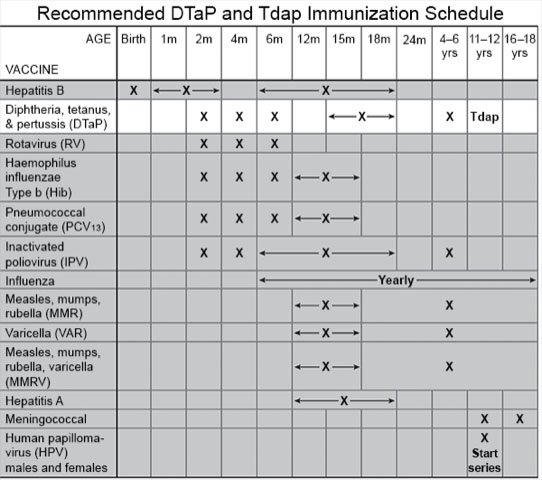
- Talk to your child's healthcare provider about vaccines. A pertussis infection will not make your child immune from another infection. The DTaP and Tdap vaccines help protect against pertussis. The vaccines are given to children in several doses. Your child's provider can help you create a schedule so you know when to bring your child in. If your adolescent is pregnant, she should get a dose of Tdap during weeks 27 to 36. Tdap will help your adolescent build antibodies against pertussis bacteria. She will also pass the antibodies to her unborn baby. This helps protect her baby from infection until his or her immune system is developed.
Follow up with your child's pediatrician as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Pertussis
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
