Pancreatitis
Medically reviewed by Drugs.com. Last updated on May 6, 2024.
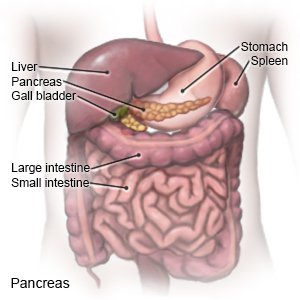
Pancreatitis is inflammation of your pancreas. The pancreas is an organ that makes insulin. It also makes enzymes (digestive juices) that help your body digest food. Pancreatitis may be an acute (short-term) problem that happens only once. It may become a chronic (long-term) problem that comes and goes over time.
 |
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
An IV
is a small tube placed in your vein that is used to give you medicine or liquids.
You may need extra oxygen
if your blood oxygen level is lower than it should be. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils. Ask your healthcare provider before you take off the mask or oxygen tubing.
A pulse oximeter
is a device that measures the amount of oxygen in your blood. A cord with a clip or sticky strip is placed on your finger, ear, or toe. The other end of the cord is hooked to a machine.
Telemetry
is continuous monitoring of your heart rhythm. Sticky pads placed on your skin connect to an EKG machine that records your heart rhythm.
Medicines:
- Antibiotics treat a bacterial infection.
- Nausea medicine helps calm your stomach and prevents vomiting.
- Pain medicine may be given. Do not wait until the pain is severe before you ask for more medicine.
Nutrition support:
If you are not able to eat food normally, you may need to be fed through a feeding tube or a catheter. You may need any of the following:
- Total parenteral nutrition (TPN) is given through your IV. TPN provides your body with nutrition such as protein, sugar, and vitamins.
- A nasogastric (NG) tube is inserted through your nose and guided down into your stomach. Food and medicine may be given through the NG tube. The tube may instead be attached to suction if your stomach needs to be empty.
- A jejunostomy tube (J-tube) is inserted through an incision in your abdomen. The end of the tube goes into your intestine. The tube is used to give you liquids, food, and medicine.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Tests:
You may be given contrast liquid to help your pancreas show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. You may need any of the following:
- Blood tests may show infection, pancreas function, or provide information about your overall health.
- An x-ray, ultrasound, MRI, or CT may show the cause of your pancreatitis and help healthcare providers plan your treatment. You may be given contrast liquid to help your pancreas show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious harm. Tell the healthcare provider if you have any metal in or on your body.
- Fine needle aspiration is a procedure used to find tissue damage or infection in your pancreas.
- Magnetic retrograde cholangiopancreatography (MRCP) uses magnetic waves to find gallstones, masses, or other problems.
- Endoscopic retrograde cholangiopancreatography (ERCP) is a procedure used to find stones, tumors, or narrowed bile ducts. ERCP may also be used to open ducts blocked by pancreatic duct stones.
Surgery
may be needed to remove your gallbladder if gallstones are causing your pancreatitis. Surgery may also be done to open blocked ducts or drain pockets of pus caused by infection.
RISKS:
Pancreatitis may lead to tissue damage and infection inside the pancreas. It can cause bleeding and fluid leakage into the abdomen. This can lead to low blood pressure, and failure of other organs. Pancreatitis can be life-threatening.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Pancreatitis
Treatment options
Care guides
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
