Myxedema Coma
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
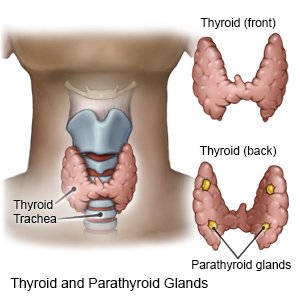
Myxedema coma is a severe form of hypothyroidism (low thyroid function). Myxedema coma occurs when thyroid hormone levels are not treated or controlled. Thyroid hormones help control body temperature, heart rate, growth, and weight. Myxedema coma can be triggered by not taking medicine to treat hypothyroidism. It may also be triggered by an infection, medicine, or a sudden stressful event, such as trauma or surgery.
 |
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
Diet and nutrition:
A dietitian may help you or family members find the best way to help you eat or get nutrition. If you cannot eat normally, you may need to receive nutrition through an IV or tube into your stomach.
Medicines:
- Thyroid hormone is given through an IV to increase thyroid hormone levels.
- Anticonvulsants are given to control seizures.
- Steroids may be given to treat adrenal problems.
- Heart medicine may be given to bring blood pressure back to normal.
- Antibiotics may be given to treat or prevent a bacterial infection.
Monitoring:
- Telemetry is continuous monitoring of your heart rhythm. Sticky pads placed on your skin connect to an EKG machine that records your heart rhythm.
- Neurologic signs are done to check reflexes and alertness.
Tests:
- Blood and urine tests are done to check for hormone levels, infection, and blood sugar levels. They are also used to get information about your overall health.
- A chest x-ray is done to look for signs of infection or fluid around the heart and lungs.
Treatment:
- Oxygen is given if your blood oxygen level is lower than it should be. You may get oxygen through a mask placed over your nose and mouth or through small tubes placed in your nostrils. Ask your healthcare provider before you take off the mask or oxygen tubing.
- A ventilator is a machine that breathes for you if you cannot breathe well on your own. You may have an endotracheal (ET) tube in your mouth, nose, or through an incision in the neck. The ET tube or trach is hooked to the ventilator.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
RISKS:
Myxedema coma may lead to long-term problems with your heart, lungs, or brain. Myxedema coma may become life-threatening.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Myxedema Coma
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
