MMR Vaccine for Children
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is the MMR vaccine?
The MMR vaccine is an injection given to help prevent measles, mumps, and rubella.
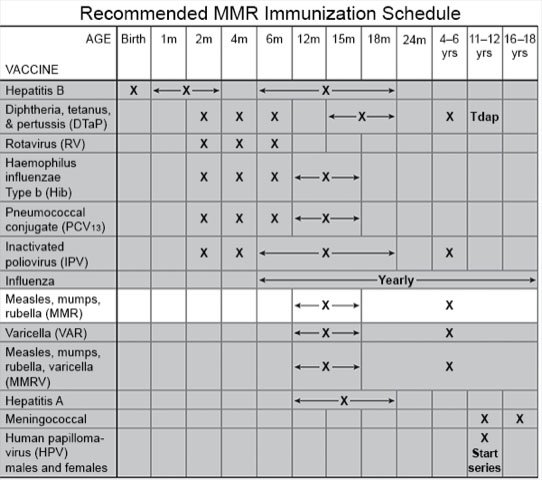
When should my child get the MMR vaccine?
The vaccine is usually given in 2 doses, but 3 doses are sometimes given. Your child's healthcare provider will tell you if your child needs a third dose, and when to get it.
- Children 12 months to 6 years usually receive 2 doses. The first dose should be given at 12 to 15 months. The second dose is usually given at 4 to 6 years. The second dose may be given before age 4 if it has been at least 4 weeks since the first.
- Infants 6 to 11 months who will be traveling internationally should get 1 dose before departure. They should then receive 2 more doses. The second dose should be given at 12 to 15 months. The third dose should be given at least 4 weeks later.
- Children 12 months or older who will be traveling internationally may need 2 doses before departure. The second dose should be given at least 4 weeks after the first.
- Children 7 to 18 years who have not had the vaccine should receive 2 doses. The second dose should be given at least 4 weeks after the first.
 |
What are reasons my child may not be able to get the MMR vaccine?
- Your child had an allergic reaction to the vaccine. Tell your child's healthcare provider about any life-threatening allergies your child has. Your child's provider can tell you if the vaccine is safe for your child.
- Your child has a severely weakened immune system or a family history of immune system disorders. The provider may recommend this vaccine if benefits outweigh the risks for your child.
What are reasons my child should wait to get the MMR vaccine?
- Your child is sick or has a fever.
- Your child received other vaccines within the past 4 weeks.
- Your child is taking a medicine that weakens the immune system, such as steroids.
- Your child has a condition that causes him or her to bleed easily, such as thrombocytopenia.
- Your child received a blood transfusion in the past 3 to 11 months.
- Your child is or may be pregnant.
- Your child has tuberculosis (TB).
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
- measles virus vaccine/mumps virus vaccine/rubella virus vaccine/varicella virus vaccine
- ProQuad
- Rotarix
- RotaTeq
- rotavirus vaccine
What are the risks of the MMR vaccine?
The area where the vaccine was given may be red, tender, or swollen. Your child may get a fever, mild rash, or swollen glands in his or her cheeks or neck. Your child's joints may be painful and swollen. Your child may have an allergic reaction to the vaccine. The MMR vaccine may cause a low platelet count, which may lead to internal bleeding. This can be life-threatening.
Call your local emergency number (911 in the US) if:
- Your child's mouth and throat are swollen.
- Your child is wheezing or has trouble breathing.
- Your child has chest pain or his or her heart is beating faster than usual.
- Your child feels like he or she is going to faint.
When should I seek immediate care?
- Your child's face is red or swollen.
- Your child has hives that spread over his or her body.
When should I call my child's doctor?
- Your child feels weak or dizzy.
- Your child has a fever or chills.
- Your child has swollen lymph glands in his or her cheeks or neck.
- Your child's joints are painful and swollen.
- Your child has increased pain, redness, or swelling around the area where the shot was given.
- You have questions or concerns about your child's condition or the MMR vaccine.
Care Agreement
You have the right to help plan your child's care. Learn about your child's health condition and how it may be treated. Discuss treatment options with your child's healthcare providers to decide what care you want for your child. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about MMR Vaccine for Children
Treatment options
Care guides
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
