Laparoscopic Cystectomy with Ileal Conduit
Medically reviewed by Drugs.com. Last updated on Jun 30, 2025.
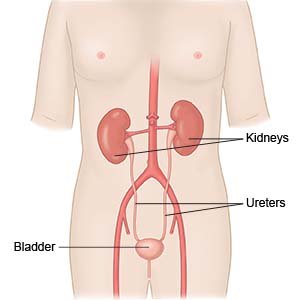
Laparoscopic cystectomy with ileal conduit is surgery to remove your bladder. Your surgeon will use a scope inserted through small incisions on your abdomen to do the surgery. He or she will use a small section of your intestines to create a urostomy (ileal conduit). This will allow urine to drain from your kidneys through an opening on your abdomen and out of your body. The opening, called a stoma, will be connected to a bag that collects urine.
 |
WHILE YOU ARE HERE:
Before your surgery:
- Informed consent is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
- Medicines may be given to prevent a bacterial infection or to prevent blood clots.
- General anesthesia will keep you asleep and free from pain during surgery. Anesthesia may be given through your IV. You may instead breathe it in through a mask or a tube placed down your throat. The tube may cause you to have a sore throat when you wake up.
During your surgery:
- General anesthesia will be given to keep you asleep and free from pain during surgery. Your surgeon will insert a scope through small incisions in your abdomen. He or she will insert tools through the scope to perform your surgery.

- Your surgeon will remove your bladder and may remove nearby tissue or organs. In men, the organs include the prostate and seminal vesicles (glands near the prostate). In women, the organs include the uterus, cervix, ovaries, and fallopian tubes. Your surgeon may also remove part of the urethra and lymph nodes near your bladder.
- Your surgeon will then remove part of your intestine. He or she will use this to connect your ureters to an opening in your abdomen (the stoma). Two small stents (tubes) will be placed inside the ureters to help urine drain while you heal. Your surgeon will close your incision with stitches or staples.
Related medications
Botox
Botox is used cosmetically to reduce facial lines and wrinkles and for medical purposes for ...
After your surgery:
You will be taken to a room to rest until you are fully awake. You will be monitored closely for any problems. Do not get out of bed until your healthcare provider says it is okay. You will then be able to go home or be taken to your hospital room.
- You will be helped to walk around after surgery. Movement will help prevent blood clots. You may also be given exercises to do in bed. Do not get out of bed on your own until your healthcare provider says you can. Talk to a healthcare provider before you get up the first time. He or she may need to help you stand up safely. When you are able to get up on your own, sit or lie down right away if you feel weak or dizzy. Then let healthcare providers know you need help.
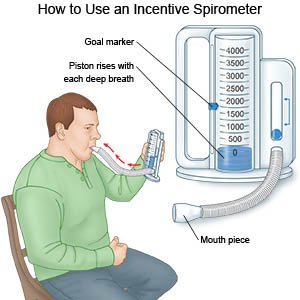
- Deep breathing and coughing will decrease your risk for a lung infection. Take a deep breath and hold it for as long as you can. Let the air out and then cough strongly. Deep breaths help open your airway. You may be given an incentive spirometer to help you take deep breaths. Put the plastic piece in your mouth and take a slow, deep breath. Then let the air out and cough. Repeat these steps 10 times every hour.
- Medicine may be given to manage pain. Medicines may also be given to treat or prevent an infection caused by bacteria, or to prevent nausea and vomiting. You may also be given medicine to decrease stomach acid or to make it easier to have a bowel movement.
RISKS:
Surgery may increase your risk for bleeding or infection. The stoma may become swollen or painful. Part of your intestine may bulge into the area around the stoma. Urine may leak where the ureters are connected to the section of intestine. You may get a kidney stone. Your ureters may become blocked and not empty urine. Your intestines may also stop working, and it may become difficult to have a bowel movement. You may develop a blood clot in your leg or arm. Any of these conditions may become life-threatening.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Laparoscopic Cystectomy with Ileal Conduit
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
