Ileostomy Creation
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
What do I need to know about ileostomy creation?
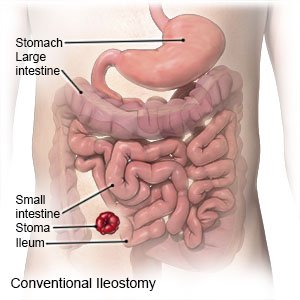
An ileostomy is an opening made on the surface of your abdomen. The lower part of your small intestine is the ileum. It is brought through the opening in your abdomen. A stoma (opening) is made from your ileum to allow you to have bowel movements. Your ileostomy may be temporary or permanent. An ileostomy is done to treat intestinal conditions such as Crohn disease, ulcerative colitis, and colorectal cancer.
How do I prepare for ileostomy creation?
- Your surgeon will make a plan a few weeks before surgery for where to place your stoma. You will also meet with an ostomy specialist to tell you what to expect after surgery.
- You will need to clean out your bowels to prepare your intestines for surgery. Your surgeon will tell you when to switch to clear liquids only. You may also need to use laxatives or an enema the night before surgery. You may be told not to eat or drink for 12 hours before your surgery.
- Tell your surgeon about all your current medicines. Your surgeon may have you stop certain medicines weeks before your surgery. Examples include blood thinners and NSAIDs, such as ibuprofen. These medicines can cause you to bleed more than expected during surgery. Your surgeon will tell you which medicines to take or not take on the day of surgery.
- Tell your surgeon about any allergies you have, including to medicines or anesthesia.
What will happen when I meet with an ostomy specialist?
Bring a family member or friend with you to learn how to help you. Write down any questions you may have so you will remember to ask them during your meetings.
- The ostomy specialist will talk with you about lifestyle changes that happen with an ileostomy.
- The specialist will explain how to prevent problems such as bowel movement leakage. You will learn stoma care to prevent a rash or infection around the stoma.
- The specialist will talk about the supplies you will need for your ileostomy. The specialist will show you how to change the ostomy bag.
- The specialist may also talk about your nutrition, bathing, and other activities after surgery.
- You may meet other people who have an ileostomy.
What will happen during surgery?
General anesthesia will be given to keep you asleep and pain-free during your surgery. Your surgeon may do any of the following, depending on if your ileostomy will be temporary or permanent:
- For a conventional ileostomy, an incision will be made in your abdomen. Your surgeon will separate your colon (lower part of your intestine) from your ileum and stitch your colon closed. Your surgeon will bring the end of your ileum through the hole in your abdomen. Then it will be folded back and stitched to the skin of your abdomen to create the stoma.
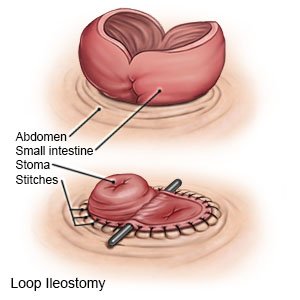
- A loop ileostomy will be created if it will be temporary. Your surgeon will bring a small section of your ileum through the hole in your abdomen. An incision will be made through one side of the ileum. Then your surgeon will fold it back and stitch it to the skin on your abdomen to create the stoma. A small rod may be placed near your stoma to secure it to your abdomen. The rod will be removed when your stoma heals.
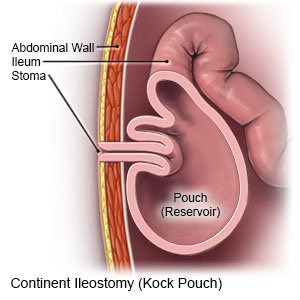
- For a continent ileostomy, your surgeon will create a reservoir from a part of your ileum. It will be inside your body and will attach to the stoma on your abdomen. It will collect bowel contents and can be emptied with a tube as needed.
What will happen after ileostomy creation?
You will stay in the hospital for up to 10 days. You will have to walk several times per day while in the hospital. You will be taught how to take care of your ileostomy.
What are the risks of an ileostomy?
- Surgery may cause bleeding or damage to nearby organs. A fistula (abnormal tissue connection) may form between your intestines and another organ. Your intestines may stop working for a period of time after surgery. You may get a life-threatening blood clot in your leg or arm.
- Your stoma or part of your intestines may become narrow or blocked. The stitches securing your ileostomy may come loose. Your stoma may slip back into your body, or come out too far on your abdomen. The rod holding your stoma in place may create a hole in your skin. You may get an infection in your intestines, reservoir pouch, urinary tract, or the skin around your stoma. The skin and intestine that forms your stoma may die. You could get a hernia (intestine that pushes through a weakened abdominal muscle wall). An ileostomy may increase your risk for dehydration.
- Your ileum may be damaged. Bowel contents may leak into your abdomen and cause a life-threatening infection.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
