Emphysema
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
Emphysema is a long-term lung disease. Emphysema is part of a group of lung diseases called chronic obstructive pulmonary disease (COPD). Emphysema damages the alveoli (air sacs) in your lungs. This makes it hard for your lungs to send oxygen to the rest of your body.
 |
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) if:
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
Seek care immediately if:
- You have shortness of breath that is so severe you cannot talk.
- You cough up blood.
- You are confused, dizzy, or feel like you may pass out.
Call your doctor or pulmonologist if:
- You have trouble reaching your oxygen level goal.
- You have a fever.
- You have trouble doing your usual activities because it is hard to breathe.
- You need to use your inhalers or take breathing treatments more often than usual.
- You cough up more sputum than is normal for you.
- You wheeze more than is normal for you.
- Your legs or ankles are swollen.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Bronchodilators help open your airway so you can breathe better. They are most often taken through one of the following devices:
- An inhaler is a handheld device that delivers medicine that you breathe in.
- A nebulizer is a machine that turns liquid medicine into mist that you breathe in through a mouthpiece.
- Steroids decrease swelling in your lungs. They may be inhaled or taken as a pill.
- Antibiotics treat a bacterial infection.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
An emphysema exacerbation
is when your symptoms suddenly get worse. You may have a harder time breathing, your cough may get worse, and you may cough up more sputum. You may have a fever, an increased heart rate, or feel more tired. An exacerbation may be caused by a lung infection, air pollution, or other lung irritants. Sometimes the cause of an exacerbation is not known.
Prevent an exacerbation:
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung damage. Ask your provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
- Avoid irritants when possible. Wear protective gear if your workplace has dust or chemicals that bother you. Avoid secondhand smoke. Stay inside when air quality is bad. Cover your mouth and nose when you are outside in cold weather or poor air quality.
- Go to pulmonary rehabilitation (rehab), as directed. Pulmonary rehab is a program to help you manage your symptoms and improve your quality of life. It may include nutritional counseling and exercise to strengthen your lungs.
- Get recommended vaccines. Get the flu vaccine as soon as recommended each year, usually in September or October. Get all recommended COVID-19 vaccine doses and booster shots. The pneumonia vaccine may also be recommended. Ask about other vaccines you may need, and when to get them.
- Prevent the spread of germs. Avoid people who are sick. Cover your mouth when you cough. Cough into a tissue or the bend of your elbow so you do not spread germs from your hands. Wash your hands often. Use soap and water. Wash your hands after you use the bathroom, change a child's diapers, or sneeze. Wash before you prepare or eat food.

- Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. You may need to eat foods that have extra calories, fat, vitamins, or calcium. Ask your provider if you need to be on a special diet.

Treatment options
The following list of medications are related to or used in the treatment of this condition.
Manage your symptoms:
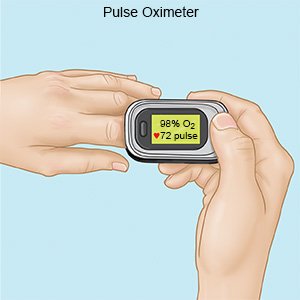
- Check your oxygen level as directed. You may need to check your blood oxygen level with a device called a pulse oximeter. The device shows your heart rate and the percentage of oxygen in your blood. You may be given an oxygen level goal for when you are at rest and another goal for activity. Your provider can tell you how often to check during the day.
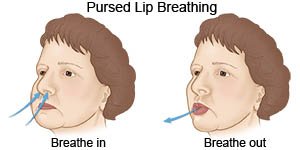
- Use pursed-lip breathing. Pursed-lip breathing can be used any time you feel short of breath. It can also be helpful before you start an activity.
- Count to 2 while you take a deep breath in through your nose.
- Slowly breathe out through your mouth with your lips slightly puckered. You should make a quiet hissing sound as you breathe out.
- Repeat this exercise 4 or 5 times a day. When you are used to doing pursed-lip breathing, you can use it any time you need more air.
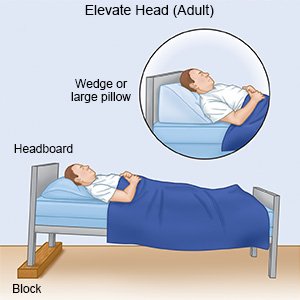
- Rest or sleep with your head elevated. This will help keep your airway open. Use foam wedges or elevate the head of your bed. Use a device that will tilt your whole body, or bend your body at the waist. The device should not bend your body at the upper back or neck.
Follow up with your doctor or pulmonologist as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Emphysema
Treatment options
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
