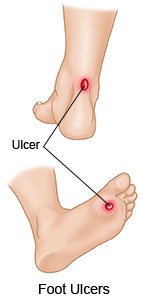
Foot Ulcers in a Person with Diabetes
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is a foot ulcer?
A foot ulcer can be redness over a bony area or an open sore. The ulcer can develop anywhere on your foot or toes. Ulcers usually develop on the bottom of the foot. You may not know you have an ulcer until you notice drainage on your sock. Drainage is fluid that may be yellow, brown, or red. The fluid may also contain pus or blood.
 |
What increases my risk for a foot ulcer?
- Blood sugar levels that are not controlled
- Nerve damage and numbness in your feet
- Poor blood flow
- A foot deformity, such as a bunion or hammertoe
- Calluses or corns on your feet or toes
- A decrease in vision that keeps you from seeing your feet clearly
- Overweight or obesity
- Cigarette smoking or alcohol use
How is a foot ulcer diagnosed and treated?
Your healthcare provider will ask about your symptoms and examine your foot and the ulcer. Your provider may check your shoes. The goal of treatment is to start healing your foot ulcer as soon as possible. The risk for infection decreases with faster healing. Do the following to help the ulcer heal:
- Prevent or treat an infection. A bandage will be put on the ulcer. Your healthcare provider will give you instructions on changing your bandage. You may need to clean the ulcer and change the bandage daily. The bandage may contain medicines to help the ulcer heal. You may be asked to put medicine on your foot ulcer before you put on the bandage. The medicine may also prevent growth of tissue that is not healthy. If you have an infection, your provider will give you antibiotics to treat it.
- Have any dead tissue debrided (removed). The removal of dead skin and tissue around your foot ulcer can help with healing.
- Manage your blood sugar levels and other health problems. Your blood sugar, blood pressure, and cholesterol levels need to be controlled to help your foot ulcer heal. Your provider can help you make a plan to manage your health problems.
- Take the pressure off the foot ulcer. You may need special shoes with insoles, cushions, or braces. You may be asked to use a wheelchair or crutches until your foot ulcer heals. These items will help keep pressure and irritation off the area of your foot ulcer. Your foot ulcer can heal faster without pressure and irritation.
- Have blood flow to your foot increased. Your provider may use hyperbaric oxygen therapy or negative pressure wound therapy to increase blood flow. Ask for more information about these therapies.
- Go to specialists as directed. Your provider may recommend you see a podiatrist, or an orthopedic or vascular surgeon. These healthcare providers may recommend any of the following wound care treatments if other treatments do not work:
- Biophysical therapy applies heat, laser, light, or electrical stimulation to your foot ulcer. This may help reduce inflammation and pain, increase blood flow, and promote wound healing.
- Autologous blood products are treatments made from your own blood to create a clot or gel. The clot or gel contains proteins to help the wound heal.
- Acellular matrix tissues are natural materials such as animal skin. These tissues are used to give a support structure for new cells to grow.
- Cellular treatments are made from living cells from a donor. The cells release substances to reduce inflammation and help new tissue grow.
- Stem cell treatment uses your own stem cells, or stem cells from a donor. Stem cells can change into different types of cells that the body can use to heal. They also provide nutrients and oxygen to the wound.
What can I do to prevent foot ulcers?
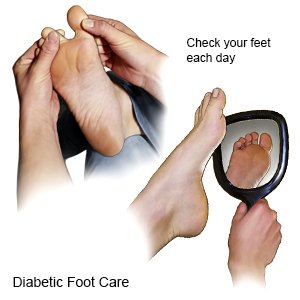
Good foot care may help prevent ulcers, or keep them from getting worse. Ask someone to help you if you are not able to check or care for your feet. The following can help you prevent foot ulcers:
- Keep your blood sugar levels under control. Continue the plan for your diabetes that you and your healthcare provider have discussed. Healthy food choices and taking your medicines as directed may help control blood sugars. Contact your provider if your blood sugar levels are higher than directed.
- Wash your feet each day with soap and warm water. Do not use hot water, because this can injure your foot. Dry your feet gently with a towel after you wash them. Dry between and under your toes.
- Apply lotion or a moisturizer on your dry feet. Ask your care team provider what lotions are best to use. Do not put lotion or moisturizer between your toes. Moisture between your toes could lead to skin breakdown.
- Check your feet each day. Look at your whole foot, including the bottom, and between and under your toes. Check for wounds, corns, and calluses. Use a mirror to see the bottom of your feet. The skin on your feet may be shiny, tight, or darker than normal. Your feet may also be cold and pale. Feel your feet by running your hands along the tops, bottoms, sides, and between your toes. Redness, swelling, and warmth are signs of blood flow problems that can lead to a foot ulcer. Do not try to remove corns or calluses yourself. Do not ignore small problems, such as dry skin or small wounds. These can become life-threatening over time without proper care.
- Cut your toenails correctly. File or cut your toenails straight across. Use a soft brush to clean around your toenails. If your toenails are very thick, you may need to have a care team provider or specialist cut them.
- Protect your feet. Do not walk barefoot or wear your shoes without socks. Check your shoes for rocks or other objects that can hurt your feet. Wear cotton socks to help keep your feet dry. Wear socks without toe seams, or wear them with the seams inside out. Change your socks each day. Do not wear socks that are dirty or damp.
- Wear shoes that fit well. Wear shoes that do not rub against any area of your feet. Your shoes should be ½ to ¾ inch (1 to 2 centimeters) longer than your feet. Your shoes should also have extra space around the widest part of your feet. Walking or athletic shoes with laces or straps that adjust are best. Ask your care team provider for help to choose shoes that fit you best. Ask your provider if you need to wear an insert, orthotic, or bandage on your feet.

- Go to your follow-up visits. Your care team provider will do a foot exam at least 1 time each year. You may need a foot exam more often if you have nerve damage, foot deformities, or ulcers. Your provider will check for nerve damage and how well you can feel your feet. Your provider will check your shoes to see if they fit well.
- Do not smoke. Smoking can damage your blood vessels and put you at increased risk for foot ulcers. Ask your care team provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your care team provider before you use these products.
- Know the risks if you choose to drink alcohol. Alcohol can cause your blood sugar levels to be low if you use insulin. Alcohol can cause high blood sugar levels and weight gain if you drink too much. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. A healthy weight can help you control your diabetes. Ask your provider to help you create a weight loss plan if needed. Even a 10 to 15 pound weight loss can help you better manage your blood sugar level.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Call your local emergency number (911 in the US) if:
- You have a fever with chills.
- You begin vomiting.
- You feel faint or become confused.
When should I seek immediate care?
- You see new drainage on your sock.
- Your foot becomes red, warm, and swollen.
- Your foot ulcer has a bad smell or is draining pus.
- You feel pain in a foot that used to have little or no feeling.
- You see black or dead tissue in or around the ulcer.
When should I call my doctor?
- The ulcer becomes bigger, deeper, or does not heal.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Foot Ulcers in a Person with Diabetes
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
