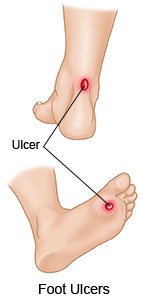
Foot Ulcers in a Person with Diabetes
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
A foot ulcer can be redness over a bony area or an open sore. The ulcer can develop anywhere on your foot or toes. Ulcers usually develop on the bottom of the foot. You may not know you have an ulcer until you notice drainage on your sock. Drainage is fluid that may be yellow, brown, or red. The fluid may also contain pus or blood.
 |
WHILE YOU ARE HERE:
Informed consent
is a legal document that explains the tests, treatments, or procedures that you may need. Informed consent means you understand what will be done and can make decisions about what you want. You give your permission when you sign the consent form. You can have someone sign this form for you if you are not able to sign it. You have the right to understand your medical care in words you know. Before you sign the consent form, understand the risks and benefits of what will be done. Make sure all your questions are answered.
An IV
is a small tube placed in your vein that is used to give you medicine or liquids.
Antibiotics
help treat a bacterial infection.
Tests:
- Blood tests may show an infection.
- An ankle brachial index test may show how well blood flows to your feet.
- A monofilament test may show nerve damage in your feet. A healthcare provider presses a small wire against the bottoms of your feet.
- A tissue, drainage, or bone sample may be taken from the ulcer to check for infection. These samples help providers find the best treatment for your foot ulcer.
- An x-ray, ultrasound, CT, or MRI may show the infection and how deep it is. You may be given contrast liquid to help the ulcer show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
Treatment:
- Debridement (removal) of dead tissue may be done in and around your foot ulcer. This procedure may be done in your hospital room.
- A bandage will be placed over the ulcer to help keep the area moist and free from infection. The bandage may contain medicines to help the ulcer heal and prevent growth of unhealthy tissue.
- Taking the pressure off the area can help it heal. Healthcare providers may use cushions or braces, or custom foot wear may be ordered. You may be asked to stay in bed or use a wheelchair or crutches. These devices help decrease the amount of weight and pressure placed on your foot.
- Surgery may be needed if you have an infection and decreased blood flow to your foot.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
RISKS:
The ulcer may not heal, or it may become infected. The infection may spread to your organs or blood. An infected foot ulcer can be life-threatening. Tissue death that is not treated can make your foot or leg start to turn black. You may need an amputation if this happens.
CARE AGREEMENT:
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Foot Ulcers in a Person with Diabetes
Treatment options
Care guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
