Chronic Lymphocytic Leukemia
Medically reviewed by Drugs.com. Last updated on Sep 1, 2024.
What is chronic lymphocytic leukemia?
Chronic lymphocytic leukemia (CLL) is cancer in your blood and bone marrow. Lymphocytes are a type of white blood cell (WBC) that prevent and fight infections. Your bone marrow makes damaged lymphocytes and your body has trouble fighting infections. It may prevent your bone marrow from making other blood cells and cause bleeding or infections.
What causes CLL?
The cause is unknown. Your risk is increased if someone in your family has had CLL or you are older than 55 years.
What are the signs and symptoms of CLL?
You may have no symptoms during the early stages of CLL. Over time, you may start to have some of the following:
- Easy bleeding or bruising
- Frequent illnesses, such as colds, coughs, or the flu
- Low energy or feeling very tired
- Fever
- Weight loss without trying
- Night sweats
- Swollen lymph nodes in your neck, armpits, or groin
- Abdominal swelling, pain, or discomfort
How is CLL diagnosed?
Your healthcare provider will ask about your symptoms and examine you. Your provider will feel your abdomen to see if your liver or spleen is larger than normal. An enlarged liver or spleen is a sign that your body has too many WBCs. Your provider will check your neck, armpits, and groin for large lymph nodes. You may need the following:
- Blood tests are used to check if your lymphocytes are damaged. Your healthcare provider will also count the number of each type of blood cell (RBCs, WBCs, platelets).
- An ultrasound may be used to check the size of your spleen, liver, or lymph nodes.
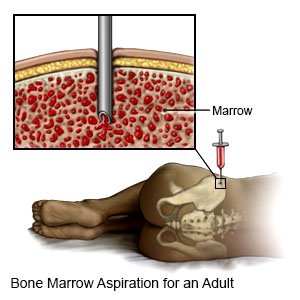
- A bone marrow biopsy is a procedure to take a small amount of bone marrow from your hip. This test helps healthcare providers find out if your bone marrow is making enough healthy blood cells.
How is CLL treated?
Your healthcare provider will use your blood tests and physical exam to determine if your CLL is early, middle, or late stage. You might not need treatment if you are in an early stage and do not have symptoms. If you do not need treatment, your healthcare provider will ask you to come back for follow-up visits. These visits will include a physical exam and blood tests. Your provider will check to see if you are still in the same stage. Your provider will also decide if you should begin treatment. You may need any of the following:
- Chemotherapy is used to kill tumor cells or shrink lymph nodes that have cancer in them.
- Biologic therapy for cancer is medicine that helps your body fight growing cancer cells. It may also make cancer cells weaker and easier to kill. You may need this medicine more than once. You may feel like you have the flu during this therapy.
- Radiation therapy shrinks tumors and kills cancer cells with x-rays or gamma rays. It may be given alone or with chemotherapy to treat cancer.
- A transplant is a procedure to put bone marrow or stem cells into your blood through an IV. The stem cells go to your bone marrow and begin to make new blood cells.
- Medicines may be given to help treat or prevent infection. Steroids may also be given to help you make healthy red blood cells.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
How may I respond to treatment?
You may have stable disease, which means your cancer does not change stages with or without treatment. You may respond one way to treatment and then have a different response later. You may have any of the following:
- Complete remission after treatment means your blood tests become normal again. The size of your spleen, liver, or lymph nodes will be normal. You will not have symptoms.
- Partial remission means you may still have signs and symptoms of CLL. Your body will have fewer damaged lymphocytes than before treatment. Your body may produce enough red blood cells. Your liver, spleen, and lymph nodes may become smaller.
- Minimal residual disease means that you have very few cancer cells left in your body.
- Progressive disease means your CLL is getting worse. Your body may not be making enough red blood cells or platelets. Your lymph nodes, spleen, and liver may get larger.
- Relapse may occur after a complete or partial response to treatment. This means that you have signs and symptoms of progressive disease. Your blood tests may become abnormal again. Your lymph nodes, spleen, and liver may get larger.
- Refractory disease means that you do not get better with treatment. You may need other treatments, such as a stem cell transplant.
What can I do to manage my CLL?
- Prevent infection. Wash your hands often, avoid people who are sick, and clean humidifiers daily. Ask your healthcare provider for more information on preventing infection.
- Prevent bleeding and bruising. Be careful with sharp or pointed objects, such as knives and toothpicks. Do not play contact sports, such as football. Use a soft toothbrush. Do not floss your teeth while your platelet count is low. Blow your nose gently. Your nose may bleed if you pick it. Do not take NSAIDs or aspirin. NSAIDs and aspirin thin your blood and increase your risk for bleeding.
- Do not smoke cigarettes or drink alcohol. Alcohol can thin your blood and make it easier to bleed. Smoking increases your risk for new or returning cancer. Smoking can also delay healing after treatment. Do not use e-cigarettes or smokeless tobacco in place of cigarettes or to help you quit. They still contain nicotine. Ask your healthcare provider for information if you currently smoke or drink and need help quitting.
- Drink liquids as directed. You may need to drink extra liquids to prevent dehydration, especially if you are vomiting or have diarrhea from cancer treatments. Ask how much liquid you need each day and which liquids are best for you.
- Exercise as directed. CLL or its treatment may make you feel tired. Exercise can help you have more energy.
- Eat healthy foods. Healthy foods may help you feel better and have more energy. If you have trouble swallowing, you may be given foods that are soft or in liquid form. Ask about any extra nutrition you may need, such as nutrition shakes or vitamins. Tell your healthcare provider if you have problems eating, or if you are nauseated.
Call your local emergency number (911 in the US) if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
When should I seek immediate care?
- You have bleeding that does not stop.
- Your heartbeat is faster than normal for you.
- You have severe pain in your abdomen.
When should I call my oncologist?
- You have a fever.
- You think you have a cough, a cold, or the flu.
- You have new bruises or bruises that are getting bigger.
- Your lymph nodes become painful or larger.
- You are losing weight without trying.
- You have night sweats.
- You feel depressed.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2024 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Chronic Lymphocytic Leukemia
Treatment options
Symptoms and treatments
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
