Benign Paroxysmal Positional Vertigo
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is benign paroxysmal positional vertigo (BPPV)?
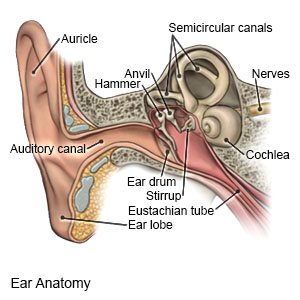
BPPV is an inner ear condition that causes you to suddenly feel dizzy. Benign means it is not serious or life-threatening. BPPV is caused by a problem with the nerves and structure of your inner ear. BPPV happens when small pieces of calcium break loose and lump together in one of your inner ear canals.
 |
What are the signs and symptoms of BPPV?
You may feel that you or the room is moving or spinning. Turning your head, rolling over in bed, getting up or lying down may lead to sudden vertigo. You may also have any of the following symptoms:
- Nystagmus (quick shaky eye movement that you cannot control)
- Nausea
- Poor balance and feeling unsteady when you walk
What increases my risk for BPPV?
- Older age
- An injury or trauma to your head or neck
- Frequent ear infections
- Long-term bed rest
- A medical condition such as diabetes, high blood pressure, migraine headaches, or Ménière disease
How is BPPV diagnosed?
Your healthcare provider will ask about your symptoms and examine you. Your healthcare provider can usually determine if you have BPPV by doing a few simple tests. He or she may have you move your head or body in certain ways. Tell him or her if you feel dizzy or nauseated during these movements.
How is BPPV managed?
- Your healthcare provider will teach you how to move your head and body to prevent symptoms. For example, he or she may teach you certain ways to move your head or body. These movements usually help relieve your symptoms and keep the dizziness from returning. The exercises help move the calcium pieces to a different part of your ear. Do the movements only as directed.
- Vestibular and balance rehabilitation therapy (VBRT) is used to teach you exercises to improve your balance and strength. VBRT may help decrease your dizziness and prevent injuries if you are at risk for falls.
- Medicines may be recommended or prescribed to treat dizziness or nausea.
How can I help prevent my symptoms?
- Try to avoid sudden head movements. Stand up and lie down slowly.
- Raise and support your head when you lie down. Place pillows under your upper back and head or rest in a recliner.
- Change your position often when you are lying down. Try not to lie with your head on the same side for long periods of time. Roll over slowly.
- Wear protective gear when you ride a bike or play sports. A helmet helps protect your head from injury.
When should I seek immediate care?
- You fall during a BPPV episode and are injured.
- You have a severe headache that does not go away.
- You have new changes in your vision or feel weak or confused.
- You have problems hearing, or you have ringing or buzzing in your ears.
When should I contact my healthcare provider?
- Your BPPV symptoms do not go away or they return.
- You have problems with your balance, or you are falling often.
- You have new or increased nausea or vomiting with vertigo.
- You feel anxious or depressed and do not want to leave your home.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
