Loratadine (Monograph)
Brand names: Alavert, Claritin
Drug class: Second Generation Antihistamines
Introduction
Second generation antihistamine;1 2 3 4 5 6 7 8 9 10 36 37 45 46 derivative of azatadine.7 10 31 37 44
Uses for Loratadine
Allergic Rhinitis
Self-medication for symptomatic relief (alone or in fixed combination with pseudoephedrine sulfate) of seasonal allergic rhinitis (e.g., hay fever);1 3 4 5 7 8 18 19 44 67 70 71 72 73 74 75 76 77 use fixed combination preparations only when both antihistamine and nasal decongestant activity are desired.18 19
As effective as astemizole (no longer commercially available in the US),4 7 39 azatadine,10 39 chlorpheniramine,7 39 clemastine,4 7 37 39 or terfenadine (no longer commercially available in the US).4 5 7 21 37 39
Has been used for the symptomatic treatment of perennial allergic rhinitis† [off-label].39
Chronic Idiopathic Urticaria
Self-medication for symptomatic relief of pruritus, erythema, and urticaria associated with chronic idiopathic urticaria (e.g., hives);1 15 16 17 21 78 not for prevention of chronic idiopathic urticaria or allergic skin reactions.78
Related/similar drugs
prednisone, hydroxyzine, fluticasone nasal, montelukast, cetirizine, triamcinolone, promethazine
Loratadine Dosage and Administration
Administration
Oral Administration
Administer conventional tablets, orally disintegrating tablets, and fixed-combination tablets orally1 2 3 4 5 6 7 8 18 19 67 70 71 72 73 74 76 77 without regard to meals.1 18 20
Orally disintegrating tablets: Place tablet on the tongue, allow it to disintegrate (within a few seconds), then swallow with or without water.1 68 71
Fixed-combination loratadine/pseudoephedrine tablets: Swallow whole; do not break, crush, chew, or dissolve.18 19 70 73 75 76 Administer Claritin-D 24 Hour tablets with a full glass of water.19 70
Dosage
Fixed-combination tablets formulated for 12-hour dosing contain 5 mg of loratadine and 60 mg of pseudoephedrine sulfate in an immediate-release outer shell and 60 mg of pseudoephedrine sulfate in an extended-release matrix core that slowly releases the drug.18
Fixed-combination tablets formulated for 24-hour dosing contain 10 mg of loratadine in an immediate-release outer shell and 240 mg of pseudoephedrine sulfate in an extended-release matrix core that slowly releases the drug.19 20
Pediatric Patients
Allergic Rhinitis
Oral
Self-medication in children 2 to <6 years of age:65 66 5 mg once daily (as oral solution).1 72
Self-medication in children ≥6 years of age:65 66 10 mg once daily (as conventional or orally disintegrating tablets or oral solution).1 5 7 10 67 68 69 74 77
Self-medication in children ≥12 years of age:65 66 5 mg every 12 hours (in fixed combination with 120 mg pseudoephedrine sulfate as the 12-hour formulation [e.g., Alavert Allergy & Sinus, Claritin-D 12 Hour])18 73 75 76 or 10 mg once daily (in fixed combination with 240 mg pseudoephedrine sulfate as the 24-hour formulation [Claritin-D 24 Hour]).19 70
Chronic Idiopathic Urticaria
Oral
Children 2–5 years of age: Not recommended for self-medication;78 a dosage of 5 mg once daily (as oral solution) has been recommended when clinicians prescribe the drug in children 2–5 years of age.1
Self-medication in children ≥6 years of age: 10 mg once daily.1 78
Adults
Allergic Rhinitis
Oral
Self-medication:65 66 10 mg once daily (as conventional or orally disintegrating tablets or oral solution).1 5 7 10 67 68 69 74 77
Self-medication: 5 mg every 12 hours (in fixed combination with 120 mg pseudoephedrine sulfate as the 12-hour formulation)18 73 75 76 or 10 mg once daily (in fixed combination with 240 mg pseudoephedrine sulfate as the 24-hour formulation).19 70
Chronic Idiopathic Urticaria
Oral
Self-medication: 10 mg once daily.1 78
Prescribing Limits
Pediatric Patients
Allergic Rhinitis
Oral
Self-medication65 66 in children 2 to <6 years of age: Maximum 5 mg once daily (as oral solution).72
Self-medication65 66 in children ≥6 years of age: Maximum 10 mg once daily (as conventional or orally disintegrating tablets or oral solution).67 68 71 77
Self-medication in children ≥12 years of age: Maximum 10 mg daily (in fixed combination with pseudoephedrine sulfate as the 12-hour or 24-hour formulations).70 73 76
Adults
Allergic Rhinitis
Oral
Self-medication65 66 : Maximum 10 mg once daily (as conventional or orally disintegrating tablets or oral solution).67 68 71 77
Self-medication: Maximum 10 mg daily (in fixed combination with pseudoephedrine sulfate as the 12-hour or 24-hour formulations).70 73 76
Special Populations
Hepatic Impairment
Self-medication: Consult a clinician.67 70 71 72 78
Children 2–5 years of age with hepatic failure: 5 mg every other day (as oral solution).1
Adults and children ≥6 years of age with hepatic failure: 10 mg every other day (as conventional or orally disintegrating tablets or oral solution).1 18
Fixed-combination loratadine/pseudoephedrine sulfate preparations generally should not be used in patients with hepatic impairment.18 19
Renal Impairment
Self-medication: Consult a clinician.67 70 71 72 78
Children 2–5 years of age with renal insufficiency (glomerular filtration rate <30 mL/minute): 5 mg every other day (as oral solution).1
Adults and children ≥6 years of age with renal insufficiency (glomerular filtration rate <30 mL/minute): 10 mg every other day (as conventional or orally disintegrating tablets or oral solution).1 18
Fixed-combination loratadine/pseudoephedrine sulfate preparations in adults and children ≥12 years of age with renal insufficiency (glomerular filtration rate <30 mL/minute): 5 mg of loratadine once daily (when the 12-hour formulation is used) or 10 mg of loratadine every other day (when the 24-hour formulation is used).18 19
Cautions for Loratadine
Contraindications
Warnings/Precautions
Warnings
Phenylketonuria
Alavert orally disintegrating tablets contain aspartame (NutraSweet), which is metabolized in the GI tract to provide 8.4 mg of phenylalanine per tablet.68
Sensitivity Reactions
Possible rash.1 Urticaria, pruritus, purpura, photosensitivity reaction, erythema multiforme, and anaphylaxis reported rarely.1 18 19
General Precautions
Use of Fixed Combinations
When using fixed-combination preparation containing pseudoephedrine sulfate, consider the cautions, precautions, and contraindications associated with pseudoephedrine.18 19
GI Obstruction and Esophageal Perforation
Mechanical upper GI obstruction and esophageal perforation reported rarely with a previously marketed formulation of Claritin-D 24 Hour tablets;19 30 individuals with a history of difficulty in swallowing tablets, a known upper GI narrowing, or abnormal esophageal peristalsis should not use the Claritin-D 24 Hour preparation since it is not known whether the currently commercially available formulation has potential for this effect.19 30
Specific Populations
Pregnancy
Lactation
Loratadine and its active metabolite desloratadine distribute readily into milk; pseudoephedrine (a component of fixed combination preparations) also distributes into milk.1 18 19 Caution advised; discontinue nursing or the drug.1 18 19
Pediatric Use
Safety and efficacy of loratadine alone or in fixed combination with pseudoephedrine sulfate not established in children <2 or <12 years of age, respectively.1 18 19
Risk of overdosage and toxicity (including death) in children <2 years of age receiving OTC preparations containing antihistamines, cough suppressants, expectorants, and nasal decongestants alone or in combination for relief of symptoms of upper respiratory tract infection.83 84 Limited evidence of efficacy for these preparations in this age group; appropriate dosages not established.83 Therefore, FDA recommended not to use such preparations in children <2 years of age;b safety and efficacy in older children under evaluation.d f FDA recommends that parents and caregivers adhere to dosage instructions and warnings on the product labeling that accompanies the preparation and consult a clinician about any concerns.c d e Clinicians should ask caregivers about use of OTC cough/cold preparations to avoid overdosage.a
Geriatric Use
Conventional or orally disintegrating tablets or oral solution: Risk of somnolence.1 Because geriatric patients frequently have decreased renal function, evaluate renal function prior to initiation and subsequently thereafter in this age group; adjust dosage if renal impairment exists or develops.1
Fixed-combination loratadine/pseudoephedrine sulfate preparations: Safety and efficacy not studied in patients ≥60 years of age.18 19 Geriatric patients are more likely to have adverse effects from sympathomimetic amines than younger patients.18 19
Hepatic Impairment
Conventional or orally disintegrating tablets or oral solution: Dosage adjustment recommended.1 (See Hepatic Impairment under Dosage and Administration.)
Fixed-combination loratadine/pseudoephedrine sulfate preparations: Use not recommended.18 19
Renal Impairment
Conventional or orally disintegrating tablets or oral solution: Dosage adjustment recommended.1 (See Renal Impairment under Dosage and Administration.)
Fixed-combination loratadine/pseudoephedrine preparations: Dosage adjustment recommended.18 19 (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Children 2–5 years of age receiving oral solution: Diarrhea, epistaxis, pharyngitis, flu-like symptoms, fatigue, stomatitis, tooth disorder, earache, viral infection, rash.1
Children 6–12 years of age receiving oral solution: Nervousness, wheezing, fatigue, hyperkinesia, abdominal pain, conjunctivitis, dysphonia, upper respiratory tract infection.1
Adults and children ≥12 years of age receiving conventional or orally disintegrating tablets: Headache, somnolence, fatigue, dry mouth.1
Fixed combination loratadine/pseudoephedrine sulfate preparations: Insomnia, dry mouth, headache, somnolence, nervousness, dizziness, fatigue.18 19
Drug Interactions
Metabolized principally by CYP3A4 and to lesser extent by CYP2D6.1 39
No formal drug interaction studies conducted with fixed combination loratadine/pseudoephedrine preparations.18 19 When using these preparations, consider drug interactions associated with pseudoephedrine.18 19
Drugs Affecting Hepatic Microsomal Enzymes
Inhibitors of CYP3A4 or CYP2D6: Potential pharmacokinetic interaction (increased plasma concentrations of loratadine and desloratadine).1 18 19 39 64 (See Specific Drugs under Interactions.)
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Cimetidine |
Increased loratadine and desloratadine concentrations; no clinically important changes in ECG or laboratory evaluations, vital signs, or adverse effects reported1 18 19 39 64 |
|
|
Ketoconazole |
Increased loratadine and desloratadine concentrations; no clinically important changes in ECG or laboratory evaluations, vital signs, or adverse effects reported1 18 19 39 64 |
|
|
Macrolide antibiotics (e.g., clarithromycin, erythromycin) |
Increased loratadine and desloratadine concentrations; no clinically important changes in ECG or laboratory evaluations, vital signs, or adverse effects reported1 18 19 39 64 |
Loratadine Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed from the GI tract following oral administration;1 10 18 19 37 38 39 42 49 in animal studies, 85% of an oral dose was absorbed.7 41 43 Peak plasma concentrations are attained in about 1.5–3.7 hours.10
Onset
Antihistaminic effect is apparent within 1–4 hours.1 10 18 19 36 39
Duration
Antihistaminic effect persists for 12–24 hours.1 2 10 18 19 38 46 61
Food
Food increases the extent of loratadine absorption and delays time to peak plasma concentration by about 1 hour.1 18 19
Special Populations
In patients with hepatic impairment, increased peak plasma loratadine concentrations and AUC secondary to impaired drug metabolism can occur.1 7 10 18 19 39
In patients with chronic renal impairment (Clcr ≤30 mL/minute), peak plasma concentrations and AUC of loratadine and desloratadine are increased compared with those in adults with normal renal function.1 4 18 19 38
In geriatric patients, peak plasma concentrations and AUC of loratadine and desloratadine are increased compared to those in younger adults.1 18 19
Distribution
Extent
Distribution has not been determined.10 Neither the drug nor its metabolites appear to cross the blood-brain barrier.1 18 19 Loratadine and its metabolites are distributed into breast milk in concentrations that are equivalent to plasma concentrations.1 7 10 18 19 40
Plasma Protein Binding
97–99% (loratadine); 73–77% (desloratadine).7 10 18 19 39 40
Elimination
Metabolism
Extensive first-pass metabolism by CYP enzymes in the liver to the active desloratadine metabolite.1 18 19 39 41 44 49 50 Metabolized principally by CYP3A4 and to lesser extent by CYP2D6.1 39
Elimination Route
Excreted equally in urine and feces as metabolic products.1 18 19
Half-life
The mean distribution half-life of loratadine is about 1–2 hours;7 10 37 41 42 the mean elimination half-life is 8–15 hours.1 7 10 18 19 37 41 42 44 49 The mean distribution half-life of desloratadine is about 2–4 hours;7 10 41 42 the mean elimination half-life is 17–28 hours.1 7 10 18 19 41 42 44 49
Special Populations
In patients with hepatic impairment, elimination half-life of loratadine and desloratadine is increased with increasing severity of hepatic disease.1 7 10 18 19 39
In patients with renal impairment (Clcr ≤30 mL/minute), mean elimination half-lives of loratadine and desloratadine appear to be similar to those in patients with normal renal function.1 4 10 18 19 39 43
In a limited number of geriatric patients (66–78 years of age), half-lives of loratadine and desloratadine were increased compared to those in younger adults.1 18 19
Stability
Storage
Oral
Tablets
2–30°C.1 Protect from excessive moisture.67 77 78
Orally Disintegrating Tablets
2–25°C.68 71 Use tablet immediately after opening individual blister; use within 6 months of opening foil pouch.71
Solution
2–25°C.72
Fixed-Combination Tablets
Actions
-
Exhibits specific, selective peripheral H1-receptor antagonistic activity.1 2 3 4 5 6 7 8 9 10 36 37 45 46
-
No appreciable anticholinergic7 10 49 or α-adrenergic blocking7 10 37 51 activity in vitro.
-
In clinical studies, incidence of CNS effects (e.g., sedation, impaired psychomotor performance) associated with loratadine is similar to that with placebo or terfenadine (no longer commercially in the US) and less than that with first generation antihistamines (e.g., azatadine, chlorpheniramine, clemastine).1 7 10 18 19 37
Advice to Patients
-
For self-medication, importance of taking only as needed and not exceeding recommended dosage; taking more than recommended dosage may cause drowsiness.67 68 70 71 72 73 76 77
-
For self-medication with loratadine in fixed combination with pseudoephedrine, importance of discontinuing therapy and contacting a clinician if symptoms do not improve within 7 days or are accompanied by fever, or if nervousness, dizziness, or sleeplessness occurs.70 73 76
-
For self-medication for management of chronic idiopathic urticaria (e.g., hives), importance of understanding that loratadine does not prevent hives.78 Importance of consulting a clinician before initiating therapy if hives are unusual in color, look bruised or blistered, or do not itch.78 Importance of discontinuing therapy and contacting a clinician if symptoms do not improve within 3 days or if hives have persisted for >6 weeks.78
-
Importance of understanding that chronic idiopathic urticaria may present with other severe allergic reactions, including anaphylactic shock (e.g., trouble swallowing, swelling of the tongue, trouble speaking, wheezing or trouble breathing, dizziness or loss of consciousness, swelling in or around the mouth, drooling).78 These manifestations may occur when hives first appear or up to several hours later and can be life-threatening if not treated immediately.78 Importance of immediately seeking emergency help if anaphylactic shock occurs.78 If an epinephrine auto-injector has been prescribed, importance of carrying this device at all times; never use loratadine as a substitute for the epinephrine auto-injector.78
-
Importance of discontinuing the drug immediately and informing a clinician if an allergic or hypersensitivity reaction occurs.67 68 69 70 71 72 73 77
-
Importance of informing patients with phenylketonuria that some orally disintegrating tablet preparations (e.g. Alavert) contain aspartame.68
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.1
-
Importance of patients with renal or hepatic impairment, heart disease, hypertension, thyroid disease, diabetes mellitus, or difficulty in urination resulting from prostate enlargement not undertaking self-medication without first consulting a clinician.1 70 73 75 (See Cautions.)
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
5 mg/5 mL |
Children's Claritin Fruit Flavored Syrup 24 Hour |
Schering-Plough |
|
Children’s Claritin Allergy, Grape Flavor |
Schering-Plough |
|||
|
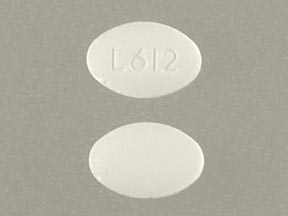
Tablets |
10 mg* |
Alavert Non-Drowsy Allergy Relief 24 Hour |
Wyeth |
|
|
Claritin Hives Relief |
Schering-Plough |
|||
|
Claritin 24 Hour |
Schering-Plough |
|||
|
Tablets, orally disintegrating |
10 mg |
Alavert Non-Drowsy Allergy Relief 24 Hour |
Wyeth |
|
|
Claritin Reditabs 24 Hour |
Schering-Plough |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, extended-release core (containing pseudoephedrine 60 mg) |
5 mg with Pseudoephedrine Sulfate 120 mg |
Alavert Allergy & Sinus D-12 Hour |
Wyeth |
|
Claritin-D 12 Hour |
Schering-Plough |
|||
|
Tablets, extended-release core (pseudoephedrine sulfate only), film-coated |
10 mg with Pseudoephedrine Sulfate 240 mg |
Claritin-D 24 Hour |
Schering-Plough |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions October 13, 2015. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Schering Corp. Claritin tablets, syrup and rapidly disintegrating tablets prescribing information. Kenilworth, NJ; 2000 Sep.
2. Kassem N, Roman I, Gural R et al. Effects of loratadine (SCH 29851) in suppression of histamine-induced skin wheals. Ann Allergy. 1988; 60:505-7. http://www.ncbi.nlm.nih.gov/pubmed/2968060?dopt=AbstractPlus
3. Oei HD. Double-blind comparison of loratadine (SCH 29851), astemizole, and placebo in hay fever with special regard to onset of action. Ann Allergy. 1988; 61:436-9. http://www.ncbi.nlm.nih.gov/pubmed/2904776?dopt=AbstractPlus
4. Quercia RA, Broisman L. Focus on loratadine: a new second-generation nonsedating H1-receptor antagonist. Hosp Formul. 1993; 28:137-53.
5. Del Carpio JD, Kabbash L, Turenne Y et al. Efficacy and safety of loratadine (10 mg once daily), terfenadine (60 mg twice daily), and placebo in the treatment of seasonal allergic rhinitis. J Allergy Clin Immunol. 1989; 84:741-6. http://www.ncbi.nlm.nih.gov/pubmed/2572617?dopt=AbstractPlus
6. Simons FER. The antiallergic effects of antihistamines (H1-receptor antagonists). J Allergy Clin Immunol. 1992; 90:705-15. http://www.ncbi.nlm.nih.gov/pubmed/1383310?dopt=AbstractPlus
7. Barenholtz AH, McLeod DC. Loratadine: a nonsedating antihistamine with once-daily dosing. DICP. 1989; 23:445-50. http://www.ncbi.nlm.nih.gov/pubmed/2525847?dopt=AbstractPlus
8. Simons FE. Loratadine, a non-sedating H1-receptor antagonist (antihistamine). Ann Allergy. 1989; 63:266-8. http://www.ncbi.nlm.nih.gov/pubmed/2572187?dopt=AbstractPlus
9. Barnett A, Iorio LC, Kreutner W et al. Evaluation of the CNS properties of SCH 29851, a potential non-sedating antihistamine. Agents Actions. 1984; 14:590-7. http://www.ncbi.nlm.nih.gov/pubmed/6236679?dopt=AbstractPlus
10. Clissold SP, Sorkin EM, Goa KL. Loratadine: a preliminary review of its pharmacodynamic properties and therapeutic efficacy. Drugs. 1989; 37:42-57. http://www.ncbi.nlm.nih.gov/pubmed/2523301?dopt=AbstractPlus
11. Borge PA. Problems in allergic rhinitis. Arzneimittelforschung. 1982; 32:1199-201. http://www.ncbi.nlm.nih.gov/pubmed/6891258?dopt=AbstractPlus
12. Anon. Treatment of seasonal and perennial rhinitis. BMJ. 1981; 283:808-10. http://www.ncbi.nlm.nih.gov/pubmed/6117350?dopt=AbstractPlus http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1507045&blobtype=pdf
13. Food and Drug Administration. Over-the-counter drugs: establishment of a monograph for OTC cold, cough, allergy, bronchodilator and antiasthmatic products. [21 CFR 341] Fed Regist. 1976; 41:38312-424. (IDIS 66640)
14. Douglas WW. Histamine and 5-hydroxytryptamine (serotonin) and their antagonists. In: Gilman AG, Goodman LS, Rall TW et al, eds. Goodman and Gilman’s the pharmacologic basis of therapeutics. 7th ed. New York: Macmillan Publishing Company; 1985:605-38.
15. Ormerod AD. Urticaria: recognition, causes and treatment. Drugs. 1994; 48:717-30. http://www.ncbi.nlm.nih.gov/pubmed/7530629?dopt=AbstractPlus
16. Monroe EW. Relative efficacy and safety of loratadine, hydroxyzine, and placebo in chronic idiopathic urticaria and atopic dermatitis. Clin Ther. 1992; 14:17-21. http://www.ncbi.nlm.nih.gov/pubmed/1349509?dopt=AbstractPlus
17. Belaich B, Bruttmann D, DeGreef H et al. Comparative effects of loratadine and terfenadine in the treatment of chronic idiopathic urticaria. Ann Allergy. 1990; 64:191-4. http://www.ncbi.nlm.nih.gov/pubmed/1967919?dopt=AbstractPlus
18. Schering Corp. Claritin-D 12 Hour (loratadine and pseudoephedrine sulfate) extended-release tablets prescribing information. Kenilworth, NJ; 1998 May.
19. Schering Corp. Claritin-D 24 Hour (loratadine and pseudoephedrine sulfate) extended-release tablets prescribing information. Kenilworth, NJ; 1998 Apr.
20. Schering Corp, Kenilworth, NJ: Personal communication.
21. Lutsky BN, Klose P, Melon J et al. A comparative study of the efficacy and safety of loratadine syrup and terfenadine suspension in the treatment of 3- to 6-year-old children with seasonal allergic rhinitis. Clin Ther. 1993; 15:855-65. http://www.ncbi.nlm.nih.gov/pubmed/8269452?dopt=AbstractPlus
22. Meltzer EO, Weiler JM, Widlitz MD. Comparative outdoor study of the efficacy, onset and duration of action, and safety of cetirizine, loratadine, and placebo for seasonal allergic rhinitis. J Allergy Clin Immunol. 1996; 97:617-26. http://www.ncbi.nlm.nih.gov/pubmed/8621847?dopt=AbstractPlus
23. Simons FER. Hl-Receptor antagonists: comparative tolerability and safety. Drug Saf. 1994; 10:350-80. http://www.ncbi.nlm.nih.gov/pubmed/7913608?dopt=AbstractPlus
24. Gosselin RE, Smith RP, Hodge HC. Clinical toxicology of commercial products. 5th ed. Baltimore: Williams & Wilkins; 1984:I10,III-36-40.
25. Cirillo VJ, Tempero KF. The pharmacology and therapeutic use of H1 and H2 antihistamines. In: Miller RR, Greenblatt DJ, eds. Drug therapy reviews. Vol 2. New York: Elsevier/North Holland Inc; 1979:24-47.
26. AMA Division of Drugs. AMA drug evaluations. 5th ed. Chicago: American Medical Association; 1983:1465-79.
27. Church JA. Allergic rhinitis: diagnosis and management. Clin Pediatr. (Philadelphia). 1980; 19:655-9.
28. Food and Drug Administration. Cold, cough, allergy, bronchodilator, and antiasthmatic drug products for over-the-counter human use; tentative final monograph for OTC antihistamine drug products. [21 FR Part 341] Fed Regist. 1985; 50:2200-18. (IDIS 195256)
29. Holgate S. Comparative trial of two non-sedative H1 antihistamines, terfenadine and astemizole, for hay fever. Thorax. 1985; 40:399. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=460082&blobtype=pdf
30. Harris AG. Dear doctor letter regarding mechanical upper GI obstruction with Claritin-D 24 Hour tablets. Kenilworth, NJ: Schering Corporation; 1997 Jul.
31. Villani FJ, Magatti CV, Vashi DB et al. N-substituted 11-(4-piperidylene)-5,6-dihydro-11H-benzo-[5,6]cyclohepta[1,2b]pyrid ines. Antihistamines with no sedating liability. Arzneimittelforschung. 1986; 36:1311-4. http://www.ncbi.nlm.nih.gov/pubmed/2947582?dopt=AbstractPlus
32. IorioLC, Cohen-Winston M, Barnett A. Interaction studies in mice of SCH 29851, a potential non-sedating antihistamine, with commonly used therapeutic agents. Agents Actions. 1986; 18:485-93. http://www.ncbi.nlm.nih.gov/pubmed/2945410?dopt=AbstractPlus
33. Sorkin EM, Heel RC. Terfenadine: a review of its pharmacodynamic properties and therapeutic efficacy. Drugs. 1985; 29:34-56. http://www.ncbi.nlm.nih.gov/pubmed/2857636?dopt=AbstractPlus
34. Moser L, Huther KJ, Koch-Weser J et al. Effects of terfenadine and diphenhydramine alone or in combination with diazepam or alcohol on psychomotor performance and subjective feelings. Eur J Clin Pharmacol. 1978; 14:417-23. (IDIS 110254)
35. Bousquet J, Chanal I, Skassa-Brociek W et al. Lack of subsensitivity to loratadine during long-term dosing during 12 weeks. J Allergy Clin Immunol. 1990; 86:248-53. http://www.ncbi.nlm.nih.gov/pubmed/1974561?dopt=AbstractPlus
36. Roman IJ, Kassem N, Gural RP et al. Suppression of histamine-induced wheal response by loratadine (SCH 29851) over 28 days in man. Ann Allergy. 1986; 57:253-6. http://www.ncbi.nlm.nih.gov/pubmed/2945499?dopt=AbstractPlus
37. Dockhorn RJ, Bergner A, Connell JT et al. Safety and efficacy of loratadine (Sch- 29851): a new non-sedating antihistamine in seasonal allergic rhinitis. Ann Allergy. 1987; 58:407-11. http://www.ncbi.nlm.nih.gov/pubmed/2954497?dopt=AbstractPlus
38. Desager J, Horsmans Y. Pharmacokinetic-pharmacodynamic relationships of H1- antihistamines. Clin Pharmacokinet. 1995; 28:419-32. http://www.ncbi.nlm.nih.gov/pubmed/7614779?dopt=AbstractPlus
39. Haria M, Fitton A, Peters DH. Loratadine. A reappraisal of its pharmacological properties and therapeutic use in allergic disorders. Drugs. 1994; 48:617-37. http://www.ncbi.nlm.nih.gov/pubmed/7528133?dopt=AbstractPlus
40. Hilbert J, Radwanski E, Affrime MB et al. Excretion of loratadine in breast milk. J Clin Pharmacol. 1988; 28:234-9. http://www.ncbi.nlm.nih.gov/pubmed/2966185?dopt=AbstractPlus
41. Hilbert J, Radwanski E, Weglein R et al. Pharmacokinetics and dose proportionality of loratadine. J Clin Pharmacol. 1987; 27:694-8. http://www.ncbi.nlm.nih.gov/pubmed/2960701?dopt=AbstractPlus
42. Radwanski E, Hilbert J, Symchowicz S et al. Loratadine: Multiple-dose pharmacokinetics. J Clin Pharmacol. 1987; 27:530-3. http://www.ncbi.nlm.nih.gov/pubmed/2958516?dopt=AbstractPlus
43. Matzke GR, Halstenson CE, Opsahl JA et al. Pharmacokinetics of loratadine in patients with renal insufficiency. J Clin Pharmacol. 1990; 30:364-71. http://www.ncbi.nlm.nih.gov/pubmed/2140371?dopt=AbstractPlus
44. Anon. Loratadine–a new antihistamine. Med Lett Drugs Ther. 1993; 35:71-2. http://www.ncbi.nlm.nih.gov/pubmed/8336639?dopt=AbstractPlus
45. Katchen B, Cramer J, Chung M et al. Disposition of14C-SCH 29851 in humans. Ann Allergy. 1985; 55:366.
46. Kassem NY, Garvin PR, Gural RP et al. Inhibition of histamine-induced wheals by SCH 29851 (SCH). Ann Allergy. 1985; 54:366.
47. Bronsky E, Boggs P, Findlay S et al. Comparative efficacy and safety of once-daily loratadine-pseudoephedrine combination versus its components alone and placebo in the management of seasonal allergic rhinitis. J Allergy Clin Immunol. 1995; 96:139-47. http://www.ncbi.nlm.nih.gov/pubmed/7636050?dopt=AbstractPlus
48. Jordana G, Dolovich J, Briscoe MP et al. Intranasal fluticasone propionate versus loratadine in the treatment of adolescent patients with seasonal allergic rhinitis. J Allergy Clin Immunol. 1996; 97:588-95. http://www.ncbi.nlm.nih.gov/pubmed/8621843?dopt=AbstractPlus
49. Hilbert J, Moritzen V, Parks A et al. The pharmacokinetics of loratadine in normal geriatric volunteers. J Int Med Res. 1988; 16:50-60. http://www.ncbi.nlm.nih.gov/pubmed/2965043?dopt=AbstractPlus
50. Hilbert JM, Matzke GR, Radwanski E et al. Loratadine pharmacokinetics in renal impairment. J Allergy Clin Immunol. 1987; 79:206.
51. BarnettA, Kreutner W. Pharmacology of non-sedating H1 antihistamines. Agents Actions. 1991; 33:181-96. http://www.ncbi.nlm.nih.gov/pubmed/1675833?dopt=AbstractPlus
52. Good AP, Rockwood R, Schad P. Loratadine and ventricular tachycardia. Am J Cardiol. 1994; 74:207. http://www.ncbi.nlm.nih.gov/pubmed/7517624?dopt=AbstractPlus
53. Woosley R, Darrow WR. Analysis of potential adverse drug reactions—A case of mistaken identity. Am J Cardiol. 1994; 74:208-9. http://www.ncbi.nlm.nih.gov/pubmed/8023797?dopt=AbstractPlus
54. Antihistamines, nonsedating /macrolide antibiotics. In: Tatro DS, Olin BR, Hebel SK eds. Drug interaction facts. St. Louis: JB Lippincott Co; 1997(Oct):110d.
55. Lindquist M, Edwards IR. Risks of non-sedating antihistamines. Lancet. 1997; 349:1322. http://www.ncbi.nlm.nih.gov/pubmed/9142080?dopt=AbstractPlus
56. O’Hanlon JF, Ramaekers JG. Antihistamine effects on actual driving performance in a standard test: a summary of Dutch experience, 1989–94. Allergy. 1995; 50:234-42. http://www.ncbi.nlm.nih.gov/pubmed/7677241?dopt=AbstractPlus
57. Ramaekers JG, Uiterwijk MM, O’Hanlon JF. Effects of loratadine and cetirazine on actual driving and psychometric test performance, and EEG during driving. Eur J Clin Pharmacol. 1992; 42:363-9. http://www.ncbi.nlm.nih.gov/pubmed/1355427?dopt=AbstractPlus
58. Gaillard AW, Gruisen A, de Jong R. The influence of antihistamines on human performance. Eur J Clin Pharmacol. 1988; 249-53. IDIS 2467817.
59. Bradley CM, Nicholson AN. Studies on the central effects of the H1-antagonist, loratadine. Eur J Clin Pharmacol. 1987; 32:419-21. http://www.ncbi.nlm.nih.gov/pubmed/2886343?dopt=AbstractPlus
60. Roth T, Roehrs T, Koshorek G et al. Sedative effects of antihistamines. J Allergy Clin Immunol. 1987; 80:94-8. http://www.ncbi.nlm.nih.gov/pubmed/2885356?dopt=AbstractPlus
61. Kassem NY, Garvin PR, Gural RP et al. Inhibition of histamine-induced wheals bt SCH 29851 (SCH). Ann Allergy. 1985; 54:366.
62. Babe KS, Serfin WE. Histamine, bradykinin, and their antagonists. In: Hardman JG, Limbird LE, Molinoff PB et al, eds. Goodman and Gilman’s the pharmacologic basis of therapeutics. 9th ed. New York: McGraw-Hill; 1996:581-600.
63. Reviewers’ comments (personal observations).
64. Carr RA, Edmonds A, Shi H et al. Steady-state pharmacokinetics and electrocardiographic pharmacodynamics of clarithromycin and loratadine after individual or concomitant administration. Antimicrobial Agents Chemother. 1998; 42:1176-1180.
65. Anon. FDA approves OTC Claritin. FDA Talk Paper. Rockville, MD: Food and Drug Administration; 2002 Nov 27.
66. Anon. Learn about Claritin. From the Claritin website. Accessed Feb 13, 2003. http://www.claritin.com
67. Schering-Plough Healthcare Products, Inc. Claritin tablets patient information. Memphis, TN; 2003 Feb.
68. Wyeth Consumer Healthcare. Alavert (loratadine) orally disintegrating tablets patient information. From the Alavert website. Accessed Feb 14, 2003. http://www.alavert.com
69. Anon. Loratadine tablets prescribing information. From the CVS website. Accessed Feb 14, 2003. http://www.cvs.com
70. Schering-Plough Healthcare Products, Inc. Claritin-D 24 Hour tablets patient information. Memphis, TN; 2003 Feb.
71. Schering-Plough Healthcare Products, Inc. Claritin RediTabs patient information. Memphis, TN; 2003 Feb.
72. Schering-Plough Healthcare Products, Inc. Children’s Claritin Fruit Flavored Syrup 24 Hour patient information. Memphis, TN; 2003 Feb.
73. Schering-Plough Healthcare Products, Inc. Claritin-D 12 Hour tablets patient information. Memphis, TN; 2003 Jul.
74. Wyeth Consumer Healthcare. Children’s Dimetapp ND Non-Drowsy Allergy (loratadine) orally disintegrating tablets patient information. Madison, NJ; 2003.
75. Wyeth Consumer Healthcare. Alavert (loratadine and pseudoephedrine sulfate) Allergy & Sinus D-12 Hour tablets patient information. Madison, NJ; 2003.
76. Wyeth Consumer Healthcare. Alavert Allergy & Sinus tablets patient information. From the Alavert website. Accessed Oct 21, 2003. http://www.alavert.com
77. Wyeth Consumer Healthcare. Alavert Easy to Swallow tablets patient information. From the Alavert website. Accessed Oct 21, 2003. http://www.alavert.com
78. Schering-Plough Healthcare Products, Inc. Claritin Hives Relief (loratadine) tablets patient information. Memphis, TN; accessed 2005 Aug.
79. Moretti ME, Caprara D, Coutinho CJ et al. Fetal safety of loratadine use in the first trimester of pregnancy: A multicenter study. J Allergy Clin Immunol. 2003; 111:479-83. http://www.ncbi.nlm.nih.gov/pubmed/12642825?dopt=AbstractPlus
80. Diav-Citrin O, Shechtman S, Aharonovich A et al. Pregnancy outcome after gestational exposure to loratadine or antihistamines: A prospective controlled cohort study. J Allergy Clin Immunol. 2003; 111:1239-43.
81. Centers for Disease Control and Prevention. Evaluation of an association between loratadine and hypospadias–United States, 1997–2001. MMWR Morb Mortal Wkly Rep. 2004; 53:219-21. http://www.ncbi.nlm.nih.gov/pubmed/15029117?dopt=AbstractPlus
82. Kallen B. Use of antihistamine drugs in early pregnancy and delivery outcome. J Matern Fetal Neonatal Med. 2002; 11:146-52. http://www.ncbi.nlm.nih.gov/pubmed/12380668?dopt=AbstractPlus
83. Srinivasan A, Budnitz D, Shehab N et al. Infant deaths associated with cough and cold medications—two states, 2005. MMWR Morb Mortal Wkly Rep. 2007; 56:1-4. http://www.ncbi.nlm.nih.gov/pubmed/17218934?dopt=AbstractPlus
84. Food and Drug Administration. Cough and cold medications in children less than two years of age. Rockville, MD; 2007 Jan 12. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm152111.htm
a. Srinivasan A, Budnitz D, Shehab N et al. Infant deaths associated with cough and cold medications—two states, 2005. MMWR Morb Mortal Wkly Rep. 2007; 56:1-4. http://www.ncbi.nlm.nih.gov/pubmed/17218934?dopt=AbstractPlus
b. Food and Drug Administration. FDA news: FDA releases recommendations regarding use of over-the-counter cough and cold products. Rockville, MD; 2008 Jan 17. From the FDA web site. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2008
c. Food and Drug Administration. Over the counter cough and cold medications. Rockville, MD; October 2008. From FDA website. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm094913.htm
d. Food and Drug Administration. FDA statement: FDA statement following CHPA’s announcement on nonprescription over-the-counter cough and cold medicines in children. 2008 Oct 8. From the FDA website. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2008/ucm116964.htm
e. Consumer Healthcare Products Association. Statement from CHPA on the voluntary label updates to oral OTC children’s cough and cold medicines. 2008 Oct 7. http://www.chpa-info.org/10_07_08_pedcc.aspx
f. Heavey S. Don’t use cold drugs in kids under 4: manufacturers. Reuters, 2008 Oct 8. From Reuters website. http://uk.reuters.com/articlePrint?articleId=UKTRE4965S520081008
Frequently asked questions
- What are the most common skin conditions? (with photos)
- Can you give loratadine to dogs?
- Why do you take Claritin with Neulasta?
- Can you take 10mg of loratadine twice a day?
- Can you take antihistamines when pregnant?
More about loratadine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (136)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: antihistamines
- Breastfeeding
- En español
Patient resources
Professional resources
Other brands
Claritin, Alavert, Allergy Relief Tablets, Allergy Relief 24 Hour, Dimetapp Children's ND Non-Drowsy Allergy