Diclofenac (Monograph)
Brand names: Cambia, Flector, Licart, Pennsaid, Voltaren, Zipsor
Drug class: Other Nonsteroidal Anti-inflammatory Agents
Chemical name: 2-[(2,6-dichlorophenyl)amino] benzeneacetic acid, monopotassium salt
Molecular formula: C14H11C12NO2•KC14H11C12NO2.NaC20H24Cl2N2O3
CAS number: 15307-81-0
Warning
- Cardiovascular Risk
-
Increased risk of serious (sometimes fatal) cardiovascular thrombotic events (e.g., MI, stroke).1 302 303 317 318 500 502 508 Risk may occur early in treatment and may increase with duration of use.500 502 505 506 508 (See Cardiovascular Thrombotic Effects under Cautions.)
-
Contraindicated in the setting of CABG surgery.508
- GI Risk
-
Increased risk of serious (sometimes fatal) GI events (e.g., bleeding, ulceration, perforation of the stomach or intestine).1 302 303 317 318 Serious GI events can occur at any time and may not be preceded by warning signs and symptoms.1 302 303 317 318 Geriatric individuals and patients with history of peptic ulcer disease and/or GI bleeding are at greater risk for serious GI events.1 302 303 317 318 (See GI Effects under Cautions.)
Introduction
Prototypical NSAIA;1 2 3 4 5 6 7 8 9 189 302 303 317 318 phenylacetic acid derivative;1 2 3 4 5 6 7 8 9 189 262 structurally related to meclofenamate sodium and mefenamic acid.203
Uses for Diclofenac
Inflammatory Diseases
Orally for symptomatic treatment of osteoarthritis,1 81 82 83 84 85 86 89 90 107 108 109 110 111 112 113 114 121 125 126 133 274 302 303 rheumatoid arthritis,1 74 75 76 77 78 79 80 87 88 107 115 116 117 118 119 121 125 126 129 254 302 303 and ankylosing spondylitis.1 91 120 121 125 127 274
Orally in fixed combination with misoprostol for the symptomatic treatment of osteoarthritis and rheumatoid arthritis in patients at high risk for developing NSAIA-induced gastric or duodenal ulcers and in patients at high risk for developing complications from these ulcers.284
Topically (as 1% gel or 1.5 or 2% solution) for the symptomatic treatment of osteoarthritis-related joint pain.318 321 325 326 327 Gel used for joints amenable to topical therapy (e.g., hands, wrists, elbows, knees, ankles, feet); has not been evaluated on joints of the spine, hip, or shoulder.318 325 Topical solution used for symptoms (e.g., pain) affecting knees.326 327 American College of Rheumatology (ACR) states that topical NSAIAs may be an appropriate initial choice for pharmacologic therapy of osteoarthritis for some patients with limited disease; oral NSAIAs more appropriate for those with hip or polyarticular involvement.330
Orally for management of juvenile rheumatoid arthritis† [off-label].3 128 210
Orally for symptomatic relief of acute gouty arthritis† [off-label].121 130 131 132
Orally or topically for symptomatic treatment of infusion-related superficial thrombophlebitis† [off-label].310 311
Pain
Orally for relief of mild to moderate acute pain, postoperative (e.g., orthopedic, gynecologic, oral) pain, and orthopedic pain (e.g., musculoskeletal sprains, traumatic joint distortions).276 277 278 279 303 331
Transdermally for relief of acute pain due to minor strains, sprains, and contusions.317 319 324
Migraine
Orally (as solution) for acute treatment of attacks of migraine with or without aura; should not be used for prophylaxis of migraine.328 329
Safety and efficacy not established for treatment of cluster headache (an older, predominantly male population).328
Dysmenorrhea
Orally for symptomatic management of primary dysmenorrhea.303
Related/similar drugs
gabapentin, acetaminophen, prednisone, ibuprofen, aspirin, meloxicam, cyclobenzaprine
Diclofenac Dosage and Administration
General
-
Consider potential benefits and risks of diclofenac therapy as well as alternative therapies before initiating therapy with the drug.1 302 303 317
Administration
Oral Administration
Diclofenac sodium delayed-release (enteric-coated) and extended-release tablets are not recommended for relief of acute pain3 248 or primary dysmenorrhea1 because of slow onset of action.53 54 56 57 60 61
Oral Solution
Empty the contents of one packet containing 50 mg of buffered diclofenac potassium powder for oral solution into a cup containing 30–60 mL of water, mix well, and administer immediately.328 Do not use liquids other than water.328
Administration with food may decrease peak plasma concentrations and reduce efficacy compared with administration on an empty stomach.328
Topical Administration
Diclofenac Sodium 1% Gel
Apply gel 4 times daily to the affected joint.318 325 Use the dosing card from the manufacturer to measure the appropriate dose.318 325 Apply the gel within the oblong area of the dosing card up to the appropriate line (2.25- or 4.5-inch line, corresponding to 2 or 4 g of gel, respectively); then use the dosing card to apply the gel.318 325 Gently massage the gel into the skin; ensure gel is applied to the entire affected joint (e.g., foot [including sole, top of foot, and toes], knee, ankle, hand [including palm, back of hand, and fingers], elbow, wrist).318
Allow application site to dry for 10 minutes before covering treated area with clothing; wait ≥60 minutes before bathing or showering.318 Wash hands after application unless the treated joint is in the hand.318
Do not apply to open wounds or areas of skin with cuts, infections, or rashes; avoid contact with eyes and mucous membranes.318 325
Do not expose treated joint to external heat or to natural or artificial sunlight; do not use occlusive dressings.318 325
Avoid application of sunscreens, cosmetics, lotions, moisturizers, insect repellents, or other topical agents to the same site; concomitant use with other topical agents not studied.318 325
Diclofenac Sodium 1.5 or 2% Topical Solution
Topical 1.5% solution: Administer as drops dispensed directly onto affected knee(s); alternatively, administer into palm of hand and apply to affected knee(s).326 To avoid spillage, apply drops in 4 increments of 10 drops each per joint; following each incremental application, spread solution evenly around the front, back, and sides of the knee.326
Topical 2% solution: Administer via pump dispenser (2 pump actuations per affected joint) into palm of hand; then evenly apply the entire volume of solution around the front, back, and sides of the knee.327 Pump must be primed before first use by fully depressing the pump mechanism 4 times while holding the bottle in an upright position.327
Wait until treated area is dry before covering with clothing; wait ≥30 minutes before bathing or showering.326 327
Wash hands after application.326 327
Avoid skin-to-skin contact between other individuals and the treated area until the area is completely dry.326 327
Do not apply to open wounds, infected or inflamed areas of skin, or areas affected with exfoliative dermatitis; avoid contact with eyes and mucous membranes.326 327
Do not expose treated knee to external heat, and avoid exposing treated knee to natural or artificial sunlight; also avoid use of occlusive dressings.326 327
Allow treated knee to dry completely before applying other topical preparations (e.g., sunscreen, insect repellant, lotions, moisturizers, cosmetics, other topical medications) to the same area.326 327
Diclofenac Epolamine Transdermal System
Apply transdermal system to the most painful area once daily (Licart) or twice daily (Flector).317 324 Apply to intact skin; do not apply to damaged skin (e.g., wounds, burns, infected areas of skin, areas affected with eczema or exudative dermatitis).317 324
Wash hands after handling the system.317 324
Avoid contact with eyes and mucous membranes.317 324
Do not wear the transdermal system while bathing or showering.317 324
If a system should begin to peel off during the period of use, the edges of the system may be taped to the skin.317 324 If problems with adhesion persist, a nonocclusive mesh netting sleeve (e.g., Curad Hold Tite, Surgilast Tubular Elastic Dressing) may be used when appropriate (e.g., over ankles, knees, or elbows) to secure the system.317 324
Dosage
Available as diclofenac potassium, diclofenac sodium, or diclofenac epolamine; dosage expressed in terms of the salt.1 302 303 317 318
To minimize the potential risk of adverse cardiovascular and/or GI events, use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals.1 302 303 317 Adjust dosage based on individual requirements and response; attempt to titrate to the lowest effective dosage.1 302 303 317
Based on safety reviews conducted to evaluate cardiovascular risk of diclofenac, some authorities (e.g., Health Canada) now recommend that systemic diclofenac dosage not exceed 100 mg daily (except on first day of treatment for dysmenorrhea when total dose of 200 mg may be administered).520 (See Cardiovascular Thrombotic Effects under Cautions.)
Different strengths and formulations of oral diclofenac are not interchangeable.331 Commercially available diclofenac sodium enteric-coated tablets, diclofenac sodium extended-release tablets, and diclofenac potassium immediate-release tablets are not necessarily bioequivalent on a mg-per-mg basis.1 302 303 Diclofenac potassium liquid-filled capsules and conventional tablets are not equivalent.332
Each actuation of the pump dispenser of diclofenac sodium 2% topical solution delivers 20 mg of diclofenac sodium in 1 g of solution.327 The 1.5% topical solution contains diclofenac sodium 16.05 mg/mL.326 The 1% gel contains 10 mg of diclofenac sodium per 1 g of gel.318
Adults
Inflammatory Diseases
Oral
Some authorities (e.g., Health Canada) recommend that systemic diclofenac dosage for inflammatory diseases not exceed 100 mg daily.520 (See Cardiovascular Thrombotic Effects under Cautions.)
Osteoarthritis
OralMay change dosage to 50 or 75 mg twice daily in patients who do not tolerate usual dosage; however, these dosages may be less effective in preventing NSAIA-induced ulcers.284
|
Preparation |
Dosage |
|---|---|
|
Diclofenac potassium conventional tablets |
100–150 mg daily, given as 50 mg 2 or 3 times daily303 |
|
Diclofenac sodium delayed-release tablets |
100–150 mg daily, given as 50 mg 2 or 3 times daily or 75 mg twice daily1 |
|
Diclofenac sodium extended-release tablets |
100 mg once daily302 |
|
Diclofenac sodium (in fixed combination with misoprostol) |
50 mg 3 times daily284 |
For lower extremity (i.e., knees, ankles, feet) joint pain, massage 4 g of diclofenac sodium 1% gel into the affected joint 4 times daily.318 325
For upper extremity (i.e., elbows, wrists, hands) joint pain, massage 2 g of diclofenac sodium 1% gel into the affected joint 4 times daily.318 325
If multiple joints are treated, total daily dose applied to all joints should be ≤32 g of gel daily.318
When used for self-medication for temporary relief of arthritis pain, treat no more than 2 body areas at the same time, and apply no more than 16 g of gel daily to any single lower extremity joint and no more than 8 g of gel daily to any single upper extremity joint.325 May use for up to 21 days unless otherwise directed by a clinician; discontinue if no pain relief within 7 days.325
Topical (solution)Diclofenac sodium 1.5% topical solution: 40 drops (approximately 1.2 mL) applied to each affected knee 4 times daily.326
Diclofenac sodium 2% topical solution: 40 mg (2 pump actuations) applied to each affected knee twice daily.327
Rheumatoid Arthritis
OralMay change dosage to 50 or 75 mg twice daily in patients who do not tolerate usual dosage; however, these dosages may be less effective in preventing NSAIA-induced ulcers.284
|
Preparation |
Dosage |
|---|---|
|
Diclofenac potassium conventional tablets |
150–200 mg daily, given as 50 mg 3 or 4 times daily303 |
|
Diclofenac sodium delayed-release tablets |
150–200 mg daily, given as 50 mg 3 or 4 times daily or 75 mg twice daily1 |
|
Diclofenac sodium extended-release tablets |
100 mg once daily; may increase to 100 mg twice daily 302 |
|
Diclofenac sodium (in fixed combination with misoprostol) |
50 mg 3 or 4 times daily284 |
Ankylosing Spondylitis
Oral100–125 mg daily (as diclofenac sodium delayed-release tablets); administer as 25 mg 4 times daily, with 5th dose at bedtime as needed.1 91 125
Pain
Oral
50 mg 3 times daily (as diclofenac potassium conventional tablets).303 Some patients may benefit from initial dose of 100 mg (followed by 50-mg doses).303
25 mg 4 times daily (as diclofenac potassium liquid-filled capsules) for mild to moderate acute pain.331
Some authorities (e.g., Health Canada) recommend that dosage not exceed 100 mg daily.520 (See Cardiovascular Thrombotic Effects under Cautions.)
Topical (transdermal system)
Apply 1 transdermal system (diclofenac epolamine 1.3%) once daily (Licart) or twice daily (Flector).317 324
Migraine
Oral
Single 50-mg dose (contents of one packet containing diclofenac potassium for oral solution mixed with water).328 Safety and efficacy of administering a second dose not established.328
Dysmenorrhea
Oral
50 mg 3 times daily (as diclofenac potassium conventional tablets).303 Some patients may benefit from initial dose of 100 mg (followed by 50-mg doses).303
Some authorities (e.g., Health Canada) state that a total dose of 200 mg may be administered on the first day of treatment for dysmenorrhea but subsequent dosage should not exceed 100 mg daily.520 (See Cardiovascular Thrombotic Effects under Cautions.)
Prescribing Limits
Adults
Based on safety reviews conducted to evaluate cardiovascular risk of diclofenac, some authorities (e.g., Health Canada) now recommend that systemic diclofenac dosage not exceed 100 mg daily (except on first day of treatment for dysmenorrhea when total dose of 200 mg may be administered).520 (See Cardiovascular Thrombotic Effects under Cautions.)
Inflammatory Diseases
Osteoarthritis
Topical (gel)Maximum total daily dose applied to all affected joints: 32 g of diclofenac sodium 1% gel.318 Maximum 16 g of gel applied daily to any single lower extremity joint and 8 g applied daily to any single upper extremity joint.318
For self-medication, treat no more than 2 body areas at the same time; maximum 16 g of gel applied daily to any single lower extremity joint and 8 g of gel applied daily to any single upper extremity joint.325 Maximum 21 days of treatment unless otherwise directed by a clinician.325
Migraine
Oral
Single 50-mg dose (as diclofenac potassium for oral solution mixed with water).328 Safety and efficacy of administering a second dose not established.328
Special Populations
Renal Impairment
Dosage adjustment not required.1 3 72 247 248 302 303 (See Renal Impairment under Cautions.)
Hepatic Impairment
Reduction of oral dosage may be necessary.1 302 303 331
Manufacturer of diclofenac potassium liquid-filled capsules recommends initiating treatment at the lowest dosage; if efficacy is not achieved at that dosage, discontinue diclofenac and consider alternative therapy.331
Cautions for Diclofenac
Contraindications
-
Known hypersensitivity (e.g., anaphylaxis, serious dermatologic reactions) to diclofenac or any ingredient in the formulation.1 302 303 317 318
-
History of asthma, urticaria, or other sensitivity reaction precipitated by aspirin or other NSAIAs.1 141 144 145 146 147 168 225 302 303 317 318
-
In the setting of CABG surgery.508
-
Diclofenac sodium in fixed combination with misoprostol: Contraindicated in pregnant women.284
-
Diclofenac epolamine transdermal system: Use on nonintact or damaged skin, regardless of etiology (e.g., exudative dermatitis, eczema, infected lesions, burns, wounds), is contraindicated.317 324
Warnings/Precautions
Warnings
Consider potential benefits and risks of diclofenac therapy as well as alternative therapies before initiating therapy with the drug.1 302 303 317 Use lowest effective dosage and shortest duration of therapy consistent with the patient’s treatment goals.1 302 303 317 318
Cardiovascular Thrombotic Effects
NSAIAs (selective COX-2 inhibitors, prototypical NSAIAs) increase the risk of serious adverse cardiovascular thrombotic events (e.g., MI, stroke) in patients with or without cardiovascular disease or risk factors for cardiovascular disease.500 502 508
Findings of FDA review of observational studies, meta-analysis of randomized controlled trials, and other published information500 501 502 indicate that NSAIAs may increase the risk of such events by 10–50% or more, depending on the drugs and dosages studied.500
Relative increase in risk appears to be similar in patients with or without known underlying cardiovascular disease or risk factors for cardiovascular disease, but the absolute incidence of serious NSAIA-associated cardiovascular thrombotic events is higher in those with cardiovascular disease or risk factors for cardiovascular disease because of their elevated baseline risk.500 502 506 508
Increased risk may occur early (within the first weeks) following initiation of therapy and may increase with higher dosages and longer durations of use.500 502 505 506 508
In controlled studies, increased risk of MI and stroke observed in patients receiving a selective COX-2 inhibitor for analgesia in first 10–14 days following CABG surgery.508
In patients receiving NSAIAs following MI, increased risk of reinfarction and death observed beginning in the first week of treatment.505 508
Increased 1-year mortality rate observed in patients receiving NSAIAs following MI;500 508 511 absolute mortality rate declined somewhat after the first post-MI year, but the increased relative risk of death persisted over at least the next 4 years.508 511
Some systematic reviews of controlled observational studies and meta-analyses of randomized studies suggest naproxen may be associated with lower risk of cardiovascular thrombotic events compared with other NSAIAs.312 313 314 316 500 501 502 503 506 FDA states that limitations of these studies and indirect comparisons preclude definitive conclusions regarding relative risks of NSAIAs.500
Findings from some meta-analyses and systematic reviews also suggest that cardiovascular risk of diclofenac, particularly at higher dosages (e.g., ≥150 mg daily), is similar to that observed with selective COX-2 inhibitors.312 313 501 503 506 520 521 Some authorities (e.g., Health Canada) recommend that systemic diclofenac dosage not exceed 100 mg daily (except for first day of treatment for dysmenorrhea).520 (See Dosage under Dosage and Administration.)
Use NSAIAs with caution and careful monitoring (e.g., monitor for development of cardiovascular events throughout therapy, even in those without prior cardiovascular symptoms) and at the lowest effective dosage for the shortest duration necessary.1 302 303 317 318 500 508
Some clinicians suggest that it may be prudent to avoid NSAIA use, whenever possible, in patients with cardiovascular disease.505 511 512 516 Avoid use in patients with recent MI unless benefits of therapy are expected to outweigh risk of recurrent cardiovascular thrombotic events; if used, monitor for cardiac ischemia.508 Contraindicated in the setting of CABG surgery.508
No consistent evidence that concomitant use of low-dose aspirin mitigates the increased risk of serious adverse cardiovascular events associated with NSAIAs.1 302 303 317 318 502 508 (See Specific Drugs under Interactions.)
GI Effects
Serious, sometimes fatal, GI toxicity (e.g., bleeding, ulceration, perforation of esophagus, stomach, or small or large intestine) can occur with or without warning symptoms.1 167 181 187 256 259 260 267 268 282 292 300 302 303 317 318
Risk for GI bleeding increased more than tenfold in patients with a history of peptic ulcer disease and/or GI bleeding who are receiving NSAIAs compared with patients without these risk factors.260 292 302 317 318
Other risk factors for GI bleeding include concomitant use of oral corticosteroids, anticoagulants, aspirin, or SSRIs; longer duration of NSAIA therapy (however, short-term therapy is not without risk); smoking; alcohol use; older age; poor general health status; and advanced liver disease and/or coagulopathy.260 292 300 302
Most spontaneous reports of fatal adverse GI effects involve geriatric or debilitated patients.1 167 181 259 302 303 317 318
Frequency of NSAIA-associated upper GI ulcers, gross bleeding, or perforation is approximately 1% in patients receiving NSAIAs for 3–6 months and 2–4% at one year.1 302 303 317 318
Use at lowest effective dosage for the shortest duration necessary.1 302 303 317 318
Avoid use of more than one NSAIA at a time.1 302 303 317 318 (See Specific Drugs under Interactions.)
Avoid use of NSAIAs in patients at higher risk for GI toxicity unless expected benefits outweigh increased risk of bleeding; consider alternate therapies in high-risk patients and those with active GI bleeding.302
For patients at high risk for complications from NSAIA-induced GI ulceration (e.g., bleeding, perforation), consider concomitant use of misoprostol;249 254 284 292 293 alternatively, consider concomitant use of a proton-pump inhibitor (e.g., omeprazole)249 254 292 or use of an NSAIA that is a selective inhibitor of COX-2 (e.g., celecoxib).249
Monitor for GI ulceration and bleeding; even closer monitoring for GI bleeding recommended in those receiving concomitant low-dose aspirin for cardiac prophylaxis.1 167 181 256 302 303 317 318
If serious adverse GI event suspected, promptly initiate evaluation and discontinue diclofenac until serious adverse GI event ruled out.1 302 303 317 318
Other Warnings and Precautions
Hepatic Effects
Severe hepatic reactions (sometimes fatal or requiring liver transplantation), including jaundice, fulminant hepatitis, liver necrosis, and hepatic failure, reported rarely with diclofenac.1 302 303 317 318 323
Serum ALT or AST elevations reported.1 79 155 302 303 317 318 323 In one large, open-label, controlled study, ALT/AST elevations were observed more frequently with diclofenac than with other NSAIAs.302 Aminotransferase elevations also observed more frequently in patients with osteoarthritis than in those with rheumatoid arthritis.302 During clinical trials, test abnormalities were observed during the first 2 months of diclofenac therapy in 82% of patients who developed marked aminotransferase elevations.302
Retrospective population-based, case-control study of drug-induced liver injury suggested current diclofenac use is associated with increased risk of liver injury (adjusted odds ratio of 4.1) compared with nonuse of the drug; findings also suggested increased risk in women compared with men and with use of higher doses (≥150 mg) and longer durations of therapy (>90 days).302 335
Monitor for symptoms and/or signs suggesting liver dysfunction.1 302 303 317 318 323 Measure serum aminotransferase concentrations at baseline and 4–8 weeks after initiating therapy; monitor periodically during long-term therapy.302 317 318 323
Use at lowest effective dosage for the shortest duration necessary; use with caution in patients receiving other potentially hepatotoxic drugs (e.g., acetaminophen, certain antibiotics, anticonvulsant agents).302
Discontinue immediately if abnormal liver function test results persist or worsen, if clinical signs and symptoms consistent with liver disease develop, or if systemic manifestations (e.g., eosinophilia, rash) occur.1 164 255 302 303 317 318 323
Hypertension
Hypertension and worsening of preexisting hypertension reported; either event may contribute to the increased incidence of cardiovascular events.1 302 303 317 318 Monitor BP during initiation of diclofenac and throughout therapy.1 302 303 317 318
Impaired response to ACE inhibitors, angiotensin II receptor antagonists, β-blockers, and certain diuretics may occur.1 302 303 317 318 508 (See Specific Drugs under Interactions.)
Heart Failure and Edema
Fluid retention and edema reported.1 302 303 317 318 508
NSAIAs (selective COX-2 inhibitors, prototypical NSAIAs) may increase morbidity and mortality in patients with heart failure.500 501 504 507 508
NSAIAs may diminish cardiovascular effects of diuretics, ACE inhibitors, or angiotensin II receptor antagonists used to treat heart failure or edema.508 (See Specific Drugs under Interactions.)
Manufacturer recommends avoiding use in patients with severe heart failure unless benefits of therapy are expected to outweigh risk of worsening heart failure; if used, monitor for worsening heart failure.508
Some experts recommend avoiding use, whenever possible, in patients with reduced left ventricular ejection fraction and current or prior symptoms of heart failure.507
Renal Effects
Direct renal injury, including renal papillary necrosis, reported in patients receiving long-term NSAIA therapy.1 302 303 317 318
Potential for overt renal decompensation.1 171 302 303 317 318 Increased risk of renal toxicity in patients with renal or hepatic impairment or heart failure, in geriatric patients, in patients with volume depletion, and in those receiving a diuretic, ACE inhibitor, or angiotensin II receptor antagonist.1 160 174 185 191 284 302 303 306 315 317 318 (See Renal Impairment under Cautions.)
Correct fluid depletion prior to initiating diclofenac; monitor renal function during therapy in patients with renal or hepatic impairment, heart failure, dehydration, or hypovolemia.302
Hyperkalemia
Hyperkalemia reported with NSAIAs, even in some patients without renal impairment; in such patients, effects attributed to a hyporenin-hypoaldosterone state.302
Hypersensitivity Reactions
Anaphylactic reactions reported.1 302 303 317 318 Immediate medical intervention and discontinuance for anaphylaxis.1 302 303 317 318
Avoid in patients with aspirin triad (aspirin sensitivity, asthma, nasal polyps); in patients with asthma but without known aspirin sensitivity. monitor for changes in manifestations of asthma.302 303 317 318
Potentially fatal or life-threatening syndrome of multi-organ hypersensitivity (i.e., drug reaction with eosinophilia and systemic symptoms [DRESS]) reported in patients receiving NSAIAs.303 Clinical presentation is variable, but typically includes eosinophilia, fever, rash, lymphadenopathy, and/or facial swelling, possibly associated with other organ system involvement (e.g., hepatitis, nephritis, hematologic abnormalities, myocarditis, myositis).303 Symptoms may resemble those of acute viral infection.303 Early manifestations of hypersensitivity (e.g., fever, lymphadenopathy) may be present in the absence of rash.303 If signs or symptoms of DRESS develop, discontinue diclofenac and immediately evaluate the patient.303
Dermatologic Reactions
Serious skin reactions (e.g., exfoliative dermatitis, Stevens-Johnson syndrome, toxic epidermal necrolysis) reported; can occur without warning.1 302 303 317 318 Discontinue at first appearance of rash or any other sign of hypersensitivity (e.g., blisters, fever, pruritus).1 302 303 317 318
Hematologic Effects
Anemia reported rarely.1 302 303 317 318 May be due to occult or gross blood loss, fluid retention, or an incompletely described effect on erythropoiesis.302 Determine hemoglobin concentration or hematocrit if signs or symptoms of anemia or blood loss occur.1 248 302 303 317 318
NSAIAs may increase the risk of bleeding.302 Patients with certain coexisting conditions (e.g., coagulation disorders) or receiving concomitant therapy with anticoagulants, antiplatelet agents, or serotonin-reuptake inhibitors may be at increased risk; monitor such patients for bleeding.302 (See Specific Drugs under Interactions.)
May inhibit platelet aggregation and prolong bleeding time.3 40 41 42 43 165 166
Precautions Specific to Diclofenac Sodium Topical Gel or Solution
Avoid exposure of treated areas to natural or artificial sunlight.318 326 327 Topical application of diclofenac gel formulations has resulted in early onset of ultraviolet (UV) light-related skin tumors in animal studies.318 321 The potential effects of topical diclofenac gel or solution on skin response to UV damage in humans are not known.318 326 327
Application to nonintact skin may alter absorption and tolerability; apply only to intact skin.318 326 327
Avoid contact with the eyes and mucous membranes.318 326 327 If contact with the eyes occurs, thoroughly rinse the eyes with water or saline.318 326 327 If ocular irritation persists for >1 hour, consult a clinician.318 326 327
Precautions Specific to Diclofenac Epolamine Transdermal System
Avoid contact with eyes and mucous membranes.317 324 If contact with the eyes occurs, thoroughly rinse the eyes with water or saline.317 324 If ocular irritation persists for >1 hour, consult a clinician.317 324
Do not apply to nonintact or damaged skin.317 324
Patient should bathe or shower after removing one transdermal system and before applying a new system; the transdermal system should not be worn during bathing or showering.317 324
Store and discard transdermal systems in a manner that avoids accidental exposure or ingestion by children or pets.317 324
Medication Overuse Headache
Excessive use of drugs indicated for the management of acute migraine attacks (e.g., use of NSAIAs, 5-HT1 receptor agonists, ergotamine, or opiates on a regular basis for ≥10 days per month) may result in migraine-like daily headaches or a marked increase in the frequency of migraine attacks.328 Detoxification, including withdrawal of the overused drugs and treatment of withdrawal symptoms (which often include transient worsening of headaches), may be necessary.328
Use of Fixed Combinations
Observe the usual cautions, precautions, and contraindications associated with misoprostol therapy when diclofenac is used in fixed combination with misoprostol.284
Concomitant NSAIA Therapy
Do not use multiple diclofenac-containing preparations concomitantly.1 302 303 Concomitant use of topical formulations of diclofenac and oral NSAIAs may increase risk of adverse effects.317 318 (See Specific Drugs under Interactions.)
Other Precautions
Not a substitute for corticosteroid therapy; not effective in the management of adrenal insufficiency.1 248 302 303 317 318
May mask certain signs of infection.1 302 303 317 318
Obtain CBC and chemistry profile periodically during long-term use.1 302 303 317 318
Specific Populations
Pregnancy
Use of NSAIAs during pregnancy at about ≥30 weeks’ gestation can cause premature closure of the fetal ductus arteriosus; use at about ≥20 weeks’ gestation associated with fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment.303 1200
Effects of NSAIAs on the human fetus during third trimester of pregnancy include prenatal constriction of the ductus arteriosus, tricuspid incompetence, and pulmonary hypertension; nonclosure of the ductus arteriosus during the postnatal period (which may be resistant to medical management); and myocardial degenerative changes, platelet dysfunction with resultant bleeding, intracranial bleeding, renal dysfunction or renal failure, renal injury or dysgenesis potentially resulting in prolonged or permanent renal failure, oligohydramnios, GI bleeding or perforation, and increased risk of necrotizing enterocolitis.1202
Avoid use of NSAIAs in pregnant women at about ≥30 weeks’ gestation; if use required between about 20 and 30 weeks’ gestation, use lowest effective dosage and shortest possible duration of treatment, and consider monitoring amniotic fluid volume via ultrasound examination if treatment duration >48 hours; if oligohydramnios occurs, discontinue drug and follow up according to clinical practice.303 1200 (See Advice to Patients.)
Fetal renal dysfunction resulting in oligohydramnios and, in some cases, neonatal renal impairment observed, on average, following days to weeks of maternal NSAIA use; infrequently, oligohydramnios observed as early as 48 hours after initiation of NSAIAs.303 1200 Oligohydramnios is often, but not always, reversible (generally within 3–6 days) following NSAIA discontinuance.303 1200 Complications of prolonged oligohydramnios may include limb contracture and delayed lung maturation.303 1200 In limited number of cases, neonatal renal dysfunction (sometimes irreversible) occurred without oligohydramnios.303 1200 Some neonates have required invasive procedures (e.g., exchange transfusion, dialysis).303 1200 Deaths associated with neonatal renal failure also reported.1200 Limitations of available data (lack of control group; limited information regarding dosage, duration, and timing of drug exposure; concomitant use of other drugs) preclude a reliable estimate of the risk of adverse fetal and neonatal outcomes with maternal NSAIA use.303 Available data on neonatal outcomes generally involved preterm infants; extent to which risks can be generalized to full-term infants is uncertain.303
Animal data indicate important roles for prostaglandins in kidney development and endometrial vascular permeability, blastocyst implantation, and decidualization.303 In animal studies, inhibitors of prostaglandin synthesis increased pre- and post-implantation losses; also impaired kidney development at clinically relevant doses.303
Diclofenac crosses the placenta.303 No evidence of teratogenicity in animal studies; however, fetal toxicity (e.g., reduced weight, growth, and survival) observed.307
Effects of diclofenac on labor and delivery not known.303 In animal studies, NSAIAs, including diclofenac, increased incidence of dystocia, delayed parturition, and increased stillbirths.303
Fixed combination of diclofenac and misoprostol: Contraindicated in pregnant women.284 Misoprostol exhibits abortifacient activity and can cause serious fetal harm.284
Lactation
May be distributed into milk; 3 303 consider the developmental and health benefits of breast-feeding along with the mother's clinical need for diclofenac and any potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.303
Fertility
NSAIAs may be associated with reversible infertility in some women.303 Reversible delays in ovulation observed in limited studies in women receiving NSAIAs; animal studies indicate that inhibitors of prostaglandin synthesis can disrupt prostaglandin-mediated follicular rupture required for ovulation.303
Consider withdrawal of NSAIAs in women experiencing difficulty conceiving or undergoing evaluation of infertility.303
Pediatric Use
Safety and efficacy not established in children.1 302 303 317 318 324 326 327 328 331
Good results with oral diclofenac obtained in a limited number of children 3–16 years of age for the management of juvenile rheumatoid arthritis† [off-label].3 128 210
Geriatric Use
Increased risk for serious adverse cardiovascular, GI, and renal effects.302 317 Fatal adverse GI effects reported more frequently in geriatric patients than younger adults.1 302 303 317 318 If anticipated benefits outweigh potential risks, initiate at lower end of dosing range and monitor for adverse effects.302 317
Diclofenac sodium 1% gel: No substantial difference in safety and efficacy in individuals ≥65 years of age compared with younger individuals; possibility of greater sensitivity to the drug in some geriatric individuals.318
Diclofenac sodium 1.5% topical solution: No age-related differences in the incidence of adverse effects observed.326 327
Diclofenac epolamine transdermal system: Insufficient experience in individuals ≥65 years of age to determine whether geriatric patients respond differently than younger individuals.317 324
Diclofenac potassium oral solution: Insufficient experience in individuals ≥65 years of age to determine whether geriatric patients respond differently than younger individuals.328
Use diclofenac with caution because of age-related decreases in renal function.302 318 May be useful to monitor renal function.302 318
Hepatic Impairment
Almost completely metabolized in the liver; reduction of oral dosage may be necessary.302 303 331
Renal Impairment
Metabolites eliminated principally via the kidney.1 302 303
May hasten progression of renal dysfunction in patients with preexisting renal disease.302 Monitor patients with preexisting renal disease for worsening renal function.302
Avoid use in patients with advanced renal disease unless benefits are expected to outweigh risk of worsening renal function; close monitoring of renal function advised if used.1 248 302 303 304 317 318
Common Adverse Effects
Oral diclofenac: Abdominal pain or cramps,1 75 86 93 107 113 136 302 303 constipation,1 75 113 132 134 136 302 303 diarrhea,1 84 86 87 93 95 125 134 302 303 flatulence,1 302 303 GI bleeding,1 302 303 GI perforation, 1 302 303 peptic ulcer,1 302 303 vomiting, 1 302 303 dyspepsia,1 302 303 nausea,1 76 78 84 85 93 95 96 97 98 99 109 111 113 126 129 134 165 302 303 dizziness,1 102 107 113 125 129 165 302 303 headache,1 89 90 91 93 95 107 110 113 118 125 127 129 132 165 302 303 liver function test abnormalities,1 116 125 165 189 209 223 255 302 303 renal function abnormalities,1 302 303 anemia,1 302 303 prolonged bleeding time,1 302 303 pruritus,1 302 303 rash,1 302 303 tinnitus,1 302 303 edema.1 109 125 132 159 165 302 303
Diclofenac sodium gel: Application site reactions (e.g., dermatitis).318
Diclofenac sodium topical solution: Application site reactions (e.g., dryness; exfoliation; erythema; pruritus; contact dermatitis with erythema, induration, or vesicles).326 327
Diclofenac epolamine transdermal system: Application site reactions (e.g., pruritus, dermatitis, irritation, erythema), nausea, altered taste.317 324
Drug Interactions
Metabolized by CYP isoenzymes, mainly CYP2C9.302 CYP3A4, uridine diphosphate-glucuronosyltransferase (UGT) 2B7, and CPY2C8 may contribute to metabolism.302
Drugs Affecting Hepatic Microsomal Enzymes
CYP2C9 inhibitors: Possible increased systemic exposure to diclofenac and risk of adverse effects. 302 Dosage adjustment may be required.302 Examples include but are not limited to voriconazole.302
CYP2C9 inducers: Possible reduced efficacy of diclofenac.302 Dosage adjustment may be required.302 Examples include, but are not limited to, rifampin.302
Protein-bound Drugs
Only minimally displaces other highly protein-bound drugs from binding sites; however, may be displaced from binding sites by other highly protein-bound drugs.51 52 59 61
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Reduced BP response to ACE inhibitor1 248 302 303 317 318 Possible deterioration of renal function, including acute renal failure, in geriatric patients and patients with volume depletion or renal impairment302 315 |
Monitor BP1 248 302 303 317 318 Ensure adequate hydration; assess renal function when initiating concomitant therapy and periodically thereafter302 Monitor geriatric patients and patients with volume depletion or renal impairment for worsening renal function302 |
|
Angiotensin II receptor antagonists |
Reduced BP response to angiotensin II receptor antagonist302 315 Possible deterioration of renal function, including acute renal failure, in geriatric patients and patients with volume depletion or renal impairment302 315 |
Monitor BP302 Ensure adequate hydration; assess renal function when initiating concomitant therapy and periodically thereafter302 Monitor geriatric patients and patients with volume depletion or renal impairment for worsening renal function302 |
|
Antacids (magnesium- or aluminum-containing) |
||
|
Anticoagulants (warfarin) |
Caution advised; carefully observe for signs of bleeding1 302 303 |
|
|
β-Adrenergic blocking agents |
Reduced BP response to β-blocker302 |
Monitor BP302 |
|
Cyclosporine |
Possible increase in nephrotoxic effects of cyclosporine1 302 303 318 |
Monitor for worsening renal function302 |
|
Digoxin |
Increased serum concentrations and prolonged half-life of digoxin302 |
Monitor serum digoxin concentrations302 |
|
Diuretics (furosemide, thiazides, potassium-sparing) |
Reduced natriuretic effects1 22 179 302 303 317 318 Potassium-sparing diuretics: Possible increased serum potassium concentrations284 Triamterene: Reversible renal impairment reported174 |
Monitor for worsening renal function and for adequacy of diuretic and antihypertensive effects1 302 303 317 318 |
|
Lithium |
Increased plasma lithium concentrations1 176 188 265 302 303 317 318 |
|
|
Methotrexate |
Possible increased risk of methotrexate toxicity (e.g., neutropenia, thrombocytopenia, renal dysfunction);302 severe, sometimes fatal toxicity associated with increased plasma methotrexate concentrations175 307 |
Monitor for methotrexate toxicity302 |
|
NSAIAs |
Concomitant NSAIAs and aspirin (analgesic dosages): Therapeutic effect not greater than that of NSAIAs alone302 Concomitant NSAIAs and aspirin: Increased risk for bleeding and serious adverse GI effects302 Concomitant use of oral and topical NSAIAs may result in higher incidence of hemorrhage and abnormal Scr, urea, and hemoglobin concentrations317 318 324 326 327 Protein binding of NSAIAs reduced by aspirin, but clearance of unbound NSAIA not altered; clinical importance unknown302 Aspirin: Decreased peak plasma concentration and AUC of diclofenac;22 61 184 202 302 303 limited data indicate that diclofenac does not inhibit antiplatelet effect of aspirin262 No consistent evidence that low-dose aspirin mitigates the increased risk of serious cardiovascular events associated with NSAIAs305 317 318 502 508 |
Concomitant use of diclofenac with analgesic dosages of aspirin generally not recommended302 Do not use topical diclofenac formulations with oral NSAIAs unless expected benefits outweigh risks; if used, periodic laboratory evaluations recommended317 318 324 326 327 Advise patients not to take low-dose aspirin without consulting clinician; closely monitor patients receiving concomitant antiplatelet agents (e.g., aspirin) for bleeding302 |
|
Pemetrexed |
Possible increased risk of pemetrexed-associated myelosuppression, renal toxicity, and GI toxicity302 |
Short half-life NSAIAs (e. g., diclofenac, indomethacin): Avoid administration beginning 2 days before and continuing through 2 days after pemetrexed administration302 Longer half-life NSAIAs (e.g., meloxicam, nabumetone): In the absence of data, avoid administration beginning at least 5 days before and continuing through 2 days after pemetrexed administration302 Patients with Clcr 45–79 mL/minute: Monitor for myelosuppression, renal toxicity, and GI toxicity302 |
|
Quinolones (ciprofloxacin) |
||
|
Serotonin-reuptake inhibitors (e.g., SSRIs, SNRIs) |
Possible increased risk of bleeding due to importance of serotonin release by platelets in hemostasis302 |
Monitor for bleeding302 |
|
Voriconazole |
Peak concentration and AUC of diclofenac increased by 114 and 78%, respectively302 |
Dosage adjustment may be required302 |
Diclofenac Pharmacokinetics
Absorption
Bioavailability
Well absorbed following oral administration.1 3 51 52 53 57 68 189 302 303 Undergoes first-pass metabolism; only 50–60% of a dose reaches systemic circulation as unchanged drug.1 52 53 73 284 302 303
Peak plasma concentration usually attained within about 15 minutes (diclofenac potassium oral solution), 0.47 hours (diclofenac potassium liquid-filled capsules), 1 hour (diclofenac potassium conventional tablets), 2 hours (diclofenac sodium delayed-release tablets), or 5.25 hours (diclofenac sodium extended-release tablets).1 3 51 52 302 303 307 328 331
Absorbed into systemic circulation following topical administration as gel, solution, or transdermal system; plasma concentrations generally very low compared with oral administration.3 227 317 318 324 326
Following application of a single diclofenac epolamine transdermal system (Flector) to intact skin on the upper arm, peak plasma concentrations occur in 10–20 hours; moderate exercise does not alter absorption.317
Following application of diclofenac epolamine transdermal system (Licart) to anterior thigh, peak concentrations occur in 4–20 hours; moderate exercise, application of an occlusion dressing over the system, or moderate heat increases peak plasma concentrations and systemic exposure by approximately 20%.324
Following topical application of diclofenac sodium 1.5% solution to knees, peak plasma concentrations occur in about 4 hours.326 Not established whether occlusive dressings, application of heat, or exercise affects absorption of diclofenac sodium 2% solution.327
Following topical application of diclofenac sodium 1% gel, peak plasma concentrations occur in about 10–14 hours.318 Moderate exercise does not alter systemic absorption.318 Application of a heat patch for 15 minutes before application of the 1% gel did not affect systemic absorption.318 Not established whether application of heat following gel application affects systemic absorption.318
Onset
Single 50- or 100-mg doses of diclofenac potassium provide pain relief within 30 minutes.307
Duration
Pain relief lasts up to 8 hours following administration of single 50- or 100-mg doses of diclofenac potassium.307
Food
Conventional, delayed-release, or extended-release tablets: Food delays time to reach peak plasma concentration but does not affect extent of absorption.1 302 303
Diclofenac potassium oral solution: Administration after a high-fat meal reduces peak plasma concentrations by approximately 70% but does not substantially affect extent of absorption.328
Diclofenac potassium liquid-filled capsules: Food decreases rate of absorption (47% decrease in peak concentration, twofold increase in time to peak concentration) but does not substantially affect extent of absorption.331
Distribution
Extent
Widely distributed in animals.3 51 52
Following oral administration, concentrations in synovial fluid may exceed those in plasma.1 3 62 63 64 65 66 67 68 69 302 303
Plasma Protein Binding
>99%.1 3 51 52 58 59 66 302 303 317
Elimination
Metabolism
Metabolized in the liver via hydroxylation and conjugation.1 3 51 52 68 70 302 303 Some metabolites may exhibit anti-inflammatory activity.1 3 22 302 303
Formation of 4′-hydroxydiclofenac (principal metabolite) is mediated mainly by CYP2C9; formation of 5-hydroxydiclofenac and 3′-hydroxydiclofenac (minor metabolites) is mediated by CYP3A4.302 UGT2B7 and CYP2C8 may mediate acyl glucuronidation and oxidation reactions, respectively.302
Elimination Route
Excreted in urine (65%) and in feces via biliary elimination (35%) as metabolites.1 3 51 55 56 70 71 302 303
Half-life
Oral preparations: 1–2 hours.2 53 57 60 302 303 328 331
Diclofenac epolamine transdermal system: Approximately 12 hours.317 324
Special Populations
In geriatric patients, pharmacokinetic profile similar to that in younger adults.307
In patients with renal impairment, plasma clearance not substantially altered,1 3 208 302 303 although clearance of metabolites may be decreased.3 72
Stability
Storage
Oral
Capsules, Liquid-filled
Tight container at 20–25°C (may be exposed to 15–30°C).331 Protect from moisture.331
Powder for Oral Solution
25°C (may be exposed to 15–30°C).328
Tablets
Tight containers at room temperature; consult manufacturer's labeling for specific storage recommendation.1 302 303 Protect from moisture.302 303
Topical
Gel
25°C (may be exposed to 15–30°C).318 325 Do not freeze.318 325
Solution
Diclofenac sodium 1.5% topical solution: Upright position at 20–25°C.326
Diclofenac sodium 2% topical solution: 25°C (may be exposed to 15–30°C).327
Transdermal System
20–25°C (may be exposed to 15–30°C).317 324 Licart systems are stable for up to 6 months after envelope is opened if stored at room temperature in the resealed envelope.324
Actions
-
Inhibits cyclooxygenase-1 (COX-1) and COX-2.285 286 287 288 289 290
-
Pharmacologic actions similar to those of other prototypical NSAIAs;1 3 20 21 22 23 24 25 26 189 302 303 317 318 exhibits anti-inflammatory, analgesic, and antipyretic activity.1 3 21 22 23 189 302 303 317 318
Advice to Patients
-
Importance of reading the medication guide for NSAIAs that is provided each time the drug is dispensed.1 302 303 317 318
-
Risk of serious cardiovascular events (e.g., MI, stroke).1 302 303 317 318 500 508 Importance of seeking immediate medical attention if signs and symptoms of a cardiovascular event (e.g., chest pain, dyspnea, weakness, slurred speech) occur.1 302 303 317 318 500 508
-
Risk of GI bleeding and ulceration.1 167 181 302 303 317 318 Importance of notifying clinician if signs and symptoms of GI ulceration or bleeding develop.1 302 303 317 318 Inform patients receiving concomitant low-dose aspirin of the increased risk of GI bleeding.303
-
Risk of hepatotoxicity.1 302 303 317 318 Importance of discontinuing therapy and contacting clinician immediately if signs and symptoms of hepatotoxicity (e.g., nausea, anorexia, fatigue, lethargy, pruritus, jaundice, upper right quadrant tenderness, flu-like symptoms) occur.1 302 303 317 318
-
Risk of serious skin reactions,1 302 303 317 318 DRESS,303 and anaphylactic and other sensitivity reactions.1 302 303 317 318 Advise patients to stop taking diclofenac immediately if they develop any type of rash or fever and to promptly contact their clinician.303 Importance of seeking immediate medical attention if an anaphylactic reaction occurs.1 302 303 317 318
-
Risk of heart failure or edema; importance of reporting dyspnea, unexplained weight gain, or edema.508
-
Importance of warning patients to keep diclofenac transdermal system out of the reach of children and pets and to safely dispose of used units.317 324
-
Importance of adhering to instructions for administration of topical diclofenac formulations (gel, solution, transdermal system).317 318 324 326 327
-
Importance of avoiding or limiting exposure of skin treated with diclofenac gel or solution to natural or artificial sunlight.318 326 327
-
If topical formulations of diclofenac come into contact with the eye(s), importance of rinsing the affected eye(s) with water or saline and of consulting a clinician if irritation persists for >1 hour.317 318 324 326 327
-
Advise patients receiving diclofenac topical solution that other individuals should avoid contact with the application site(s) until the site is completely dry.326 327
-
Advise patients receiving diclofenac topical solution to promptly contact their clinician if any type of rash develops at the application site.326
-
When diclofenac topical gel is used for self-medication for temporary relief of arthritis pain, importance of reviewing the product labeling and of not exceeding the recommended dosage or duration of therapy.325 Advise patients that efficacy is not established for symptomatic relief of strains, sprains, bruises, or sports injuries.325
-
Advise patients with migraine headaches that overuse of drugs intended for acute treatment of migraine attacks (e.g., use on ≥10 days per month) may exacerbate headaches; encourage patients to record the frequency of migraine headaches and medication use.328
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 302 303 317 318
-
Importance of avoiding NSAIA use beginning at 20 weeks’ gestation unless otherwise advised by a clinician; importance of avoiding NSAIAs beginning at 30 weeks’ gestation because of risk of premature closure of the fetal ductus arteriosus; monitoring for oligohydramnios may be necessary if NSAIA therapy required for >48 hours’ duration between about 20 and 30 weeks’ gestation.303 1200
-
Advise women who are trying to conceive that NSAIAs may be associated with a reversible delay in ovulation.303
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs.1 302 303 317 318 Advise patients that concomitant use of other NSAIAs with diclofenac provides little or no increase in efficacy but increases risk of GI toxicity, and is not recommended.303 Advise patients not to use concomitant low-dose aspirin without consulting their clinician.303 Alert patients to the presence of NSAIAs in many OTC preparations.303
-
Importance of informing patients of other important precautionary information.1 302 303 317 318 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Topical |
Transdermal System |
1.3%* |
Diclofenac Epolamine Transdermal System |
|
|
Flector |
Pfizer |
|||
|
Licart |
IBSA |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules, liquid-filled |
25 mg |
Zipsor |
Depomed |
|
For oral solution |
50 mg* |
Cambia |
Assertio |
|
|
Diclofenac Potassium for Oral Solution |
||||
|
Tablets |
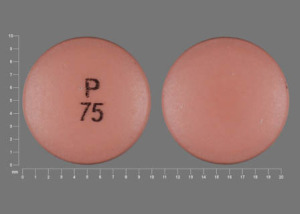
50 mg* |
Diclofenac Potassium Tablets |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, delayed-release (enteric-coated) |
25 mg* |
Diclofenac Sodium Delayed-release Tablets |
|
|
50 mg* |
Diclofenac Sodium Delayed-release Tablets |
|||
|
75 mg* |
Diclofenac Sodium Delayed-release Tablets |
|||
|
Tablets, extended-release |
100 mg* |
Diclofenac Sodium Extended-release Tablets |
||
|
Topical |
Gel |
1%* |
Diclofenac Sodium Gel |
|
|
Voltaren |
Endo |
|||
|
Voltaren Arthritis Pain |
GlaxoSmithKline |
|||
|
Solution |
1.5%* |
Diclofenac Sodium Topical Solution |
||
|
2% |
Pennsaid |
Horizon |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, delayed-release (enteric-coated core), film-coated |
50 mg diclofenac sodium enteric-coated core, with 200 mcg of misoprostol outer layer* |
Arthrotec |
Pfizer |
|
Diclofenac Sodium and Misoprostol Delayed-release Tablets |
||||
|
75 mg diclofenac sodium enteric-coated core, with 200 mcg of misoprostol outer layer* |
Arthrotec |
Pfizer |
||
|
Diclofenac Sodium and Misoprostol Delayed-release Tablets |
AHFS DI Essentials™. © Copyright 2024, Selected Revisions November 9, 2020. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Novartis. Voltaren (diclofenac sodium enteric-coated tablets) prescribing information. East Hanover, NJ; 2006 Jan.
2. Reynolds JEF, ed. Martindale: the extra pharmacopeia. 28th ed. London: The Pharmaceutical Press; 1989:250.
3. Todd PA, Sorkin EM. Diclofenac sodium: a reappraisal of its pharmacodynamic and pharmacokinetic properties, therapeutic efficacy. Drugs. 1988; 35:244-85. http://www.ncbi.nlm.nih.gov/pubmed/3286213?dopt=AbstractPlus
4. Brogden RN, Heel RC, Pakes GE et al. Diclofenac sodium: a review of its pharmacological properties and therapeutic use in rheumatic diseases and pain of varying origin. Drugs. 1980; 20:24-48. http://www.ncbi.nlm.nih.gov/pubmed/6772422?dopt=AbstractPlus
5. Windholz M, ed. The Merck index. 10th ed. Rahway, NJ: Merck & Co, Inc; 1983:447-8.
6. Hart FD, Huskisson EC, Answell BM. Non-steroidal anti-inflammatory analgesics. In: Hart FD, ed. Drug treatment of the rheumatic diseases. 2nd ed. Balgowlah, NSW Australia: ADIS Press; 1982:7-60.
7. Fowler PD. Voltarol: diclofenac sodium. Clin Rheum Dis. 1979; 5:427-64.
8. Calabro JJ, Ehrlich GE. Introduction. Am J Med. 1986; 80(Suppl 4B):1-3.
9. Sallmann AR. The history of diclofenac. Am J Med. 1986; 80(Suppl 4B):29-33. http://www.ncbi.nlm.nih.gov/pubmed/3085489?dopt=AbstractPlus
10. Fini A, De Maria P, Guarnieri A et al. Acidity constants of sparingly water-soluble drugs from potentiometric determinations in aqueous dimethyl sulfoxide. J Pharm Sci. 1987; 76:48-52. http://www.ncbi.nlm.nih.gov/pubmed/3585723?dopt=AbstractPlus
11. Abramson S, Edelson H, Kaplan H et al. Inhibition of neutrophil activation by nonsteroidal anti-inflammatory drugs. Am J Med. 1984; 10:3-6.
12. Moncada S, Flower RJ, Vane JR. Prostaglandins, prostacyclin, thromboxane A2, and leukotrienes. In: Gilman AG, Goodman LS, Rall TW et al, eds. Goodman and Gilman’s the pharmacological basis of therapeutics. 7th ed. New York; Macmillan Publishing Company; 1985; 660- 73.
13. Deraedt R, Jouquey S, Benzoni J et al. Inhibition of prostaglandin biosynthesis by non-narcotic analgesic drugs. Arch Int Pharmacodyn Ther. 1976; 224:30-42. http://www.ncbi.nlm.nih.gov/pubmed/13749?dopt=AbstractPlus
14. Atkinson DC, Collier HOJ. Salicylates: molecular mechanism of therapeutic action. Adv Pharmacol Chemother. 1980; 233-88.
15. Robinson DR. Prostaglandins and the mechanism of action of anti-inflammatory drugs. Am J Med. 1983; 10:26-31.
16. O’Brien WM. Pharmacology of nonsteroidal anti- inflammatory drugs. Am J Med. 1983; 10:32-9.
17. Koch-Weser J. Nonsteroidal antiinflammatory drugs (first of two parts). N Engl J Med. 1980; 302:1179-85. http://www.ncbi.nlm.nih.gov/pubmed/6988717?dopt=AbstractPlus
18. Ferreira SH, Lorenzetti BB, Correa FMA. Central and peripheral analgesic action of aspirin-like drugs. Eur J Pharmacol. 1978; 53:39-48. http://www.ncbi.nlm.nih.gov/pubmed/310771?dopt=AbstractPlus
19. Hart FD. Rheumatic disorders. In: Avery GS, ed. Drug treatment: principles and practice of clinical pharmacology and therapeutics. 2rd ed. New York: ADIS Press; 1987:910-57.
20. Ku EC, Lee W, Kothari HV et al. The effects of diclofenac sodium on arachidonic acid metabolism. Semin Arthritis Rheum. 1985; 15(Suppl 1):36-41. http://www.ncbi.nlm.nih.gov/pubmed/3936178?dopt=AbstractPlus
21. Scholer DW, Ku EC, Boettcher I et al. Pharmacology of diclofenac sodium. Am J Med. 1986; 80(Suppl 4B):34-8. http://www.ncbi.nlm.nih.gov/pubmed/3085490?dopt=AbstractPlus
22. Menassé R, Hedwall PR, Kraetz J et al. Pharmacological properties of diclofenac sodium and its metabolites. Scand J Rheumatol. 1978; 22(Suppl):5-16.
23. Ku EC, Lee W, Kothari HV et al. Effect of diclofenac sodium on the arachidonic acid cascade. Am J Med. 1986; 80(Suppl 4B):18-23. http://www.ncbi.nlm.nih.gov/pubmed/3085488?dopt=AbstractPlus
24. Peters P, Cooper C, Maiorana K et al. The effect of topically applied agents on ultraviolet erythema in guinea pigs. Agents Actions. 1977; 7:545- 53. http://www.ncbi.nlm.nih.gov/pubmed/414528?dopt=AbstractPlus
25. De Menezes MRD, Catanzaro-Guimaraes SA. Determination of anti-inflammatory and antimitotic activities of non-steroid anti-inflammatory drugs ibuprofen, diclofenac sodium and fentiazac. Cell Mol Biol. 1985; 31:455-61. http://www.ncbi.nlm.nih.gov/pubmed/4075369?dopt=AbstractPlus
26. Ku EC, Wasvary JM, Cash WD. Diclofenac sodium (GP 45840, Voltaren), a potent inhibitor of prostaglandin synthetase. Biochem Pharmacol. 1975; 24:641-3. http://www.ncbi.nlm.nih.gov/pubmed/804905?dopt=AbstractPlus
27. Perianin A, Gougerot-Pocidalo MA, Giroud JP et al. Diclofenac sodium, a negative chemokinetic factor for neutrophil locomotion. Biochem Pharmacol. 1985; 34:3433-8. http://www.ncbi.nlm.nih.gov/pubmed/3902025?dopt=AbstractPlus
28. Friman C, Johnston C, Chew C et al. Effect of diclofenac sodium, tolfenamic acid and indomethacin on the production of superoxide induced by N-formyl- methionyl-leucyl-phenylalanine in normal human polymorphonuclear leukocytes. Scand J Rheumatol. 1986; 15:41-6. http://www.ncbi.nlm.nih.gov/pubmed/3008321?dopt=AbstractPlus
29. Martini A, Bondiolotti GP, Sacerdote P et al. Diclofenac increases beta-endorphin plasma concentrations. J Int Med Res. 1984; 12:92-5. http://www.ncbi.nlm.nih.gov/pubmed/6202572?dopt=AbstractPlus
30. Sacerdote P, Monza G, Mantegazza P et al. Diclofenac and pirprofen modify pituitary and hypothalamic beta-endorphin concentrations. Pharmacol Res Commun. 1985; 17:679-84. http://www.ncbi.nlm.nih.gov/pubmed/2931730?dopt=AbstractPlus
31. Tiitinen S, Nissila M, Ruutsalo HM et al. Effect of nonsteroidal anti-inflammatory drugs on the renal excretion of uric acid. Clin Rheumatol. 1983; 2:233-6. http://www.ncbi.nlm.nih.gov/pubmed/6678696?dopt=AbstractPlus
32. Vandenburg MJ, Currie WJC, Mann SG et al. Differential effects of two non steroidal anti- inflammatory drugs on the plasma urea of elderly patients with osteoarthritis: a multicentre study. Br J Clin Pract. 1984; 38:403-6. http://www.ncbi.nlm.nih.gov/pubmed/6397222?dopt=AbstractPlus
33. Laurent J, Belghiti D, Bruneau C et al. Diclofenac, a nonsteroidal anti-inflammatory drug, decreases proteinuria in some glomerular diseases: a controlled study. Am J Nephrol. 1987; 7:198-202. http://www.ncbi.nlm.nih.gov/pubmed/3307414?dopt=AbstractPlus
34. Oliw E, Lundén I, Anggard E. In vivo inhibition of prostaglandin synthesis in rabbit kidney by non-steroidal anti-inflammatory drugs. Acta Pharmacol Toxicol (Copenh). 1978; 42:179-84. http://www.ncbi.nlm.nih.gov/pubmed/580346?dopt=AbstractPlus
35. Rainsford KD, Willis C. Relationship of gastric mucosal damage induced in pigs by antiinflammatory drugs to their effects on prostaglandin production. Dig Dis Sci. 1982; 27:624-35. http://www.ncbi.nlm.nih.gov/pubmed/6953009?dopt=AbstractPlus
36. Kobayashi K, Arakawa T, Satoh H et al. Effect of indomethacin, tiaprofenic acid and dicrofenac [sic] on rat gastric mucosal damage and content of prostacyclin and prostaglandin E2. Prostaglandins. 1985; 30:609-18. http://www.ncbi.nlm.nih.gov/pubmed/3909233?dopt=AbstractPlus
37. Rainsford KD. The comparative gastric ulcerogenic activities of non-steroid anti-inflammatory drugs. Agents Actions. 1977; 7:573-7. http://www.ncbi.nlm.nih.gov/pubmed/602882?dopt=AbstractPlus
38. Lehtola J, Sipponen P. A gastroscopic and histological double-blind study of the effects of diclofenac sodium and naproxen on the human gastric mucosa. Scand J Rheumatol. 1977; 6:97-102. http://www.ncbi.nlm.nih.gov/pubmed/331465?dopt=AbstractPlus
39. Yasunaga K. [Effect of N-(2,6-dichlorophenyl)- o-aminophenylacetic acid (GP 45 840) on blood platelets, coagulation and fibrinolysis.] (Japanese; with English abstract.) Naika Hokan. 1972; 19:301-6.
40. Fowler PD. Diclofenac sodium (Voltarol): drug interactions and special studies. Rheumatol Rehabil. 1979; 18(Suppl 2):60-8.
41. Rorarius M, Miralles J, Baer GA et al. Diclofenac versus indomethacin given as intravenous infusions: their effect on haemodynamics and bleeding time, and side-effects in healthy subjects. Ann Clin Res. 1985; 17:306-9. http://www.ncbi.nlm.nih.gov/pubmed/3913378?dopt=AbstractPlus
42. Djaldetti M, Fishman P, Creter D et al. Ultrastructural and functional studies on human platelets incubated with diclofenac sodium (Voltaren). Acta Haematol. 1982; 68:285-94. http://www.ncbi.nlm.nih.gov/pubmed/6817571?dopt=AbstractPlus
43. Jobin F, Gagnon FT. Inhibition of human platelet aggregation by a dibenzazepine compound (GP 44296) and by N-(2,6-dichlorophenyl)-o- aminophenylacetic acid (GP 45840). Can J Physiol Pharmacol. 1971; 49:479-81. http://www.ncbi.nlm.nih.gov/pubmed/5120275?dopt=AbstractPlus
44. Oates JA, FitzGerald GA, Branch RA et al. Clinical implications of prostaglandin and thromboxane A2 formation (first of two parts). N Engl J Med. 1988; 319:689-98. http://www.ncbi.nlm.nih.gov/pubmed/3045550?dopt=AbstractPlus
45. Al-Waili NS. Diclofenac sodium and intractable epilepsy. Acta Neurol Scand. 1986; 73:507. http://www.ncbi.nlm.nih.gov/pubmed/3727929?dopt=AbstractPlus
46. Araie M, Sawa M, Takase M. Topical flurbiprofen and diclofenac suppress blood-aqueous barrier breakdown in cataract surgery: a fluorophotometric study. Jpn J Ophthalmol. 1983; 27:535-42. http://www.ncbi.nlm.nih.gov/pubmed/6656015?dopt=AbstractPlus
47. Bonfiglioli D, Sommariva D, Zanaboni L et al. Influence of two non-steroidal anti-inflammatory drugs on lipolysis and on plasma post-heparin lipoprotein lipase activity in normal man. Eur J Clin Pharmacol. 1981; 20:263-7. http://www.ncbi.nlm.nih.gov/pubmed/6796423?dopt=AbstractPlus
48. Bhattacherjee P. Prostaglandins and inflammatory reactions in the eye. Methods Find Exp Clin Pharmacol. 1980; 2:17-31. http://www.ncbi.nlm.nih.gov/pubmed/6803089?dopt=AbstractPlus
49. Podos SM, Becker B. Comparison of ocular prostaglandin synthesis inhibitors. Invest Ophthalmol. 1976; 15:841-4. http://www.ncbi.nlm.nih.gov/pubmed/977253?dopt=AbstractPlus
50. Osnes M, Larsen S, Eidsaunet W et al. Effect of diclofenac and naproxen on gastroduodenal mucosa. Clin Pharmacol Ther. 1979; 26:399-405. http://www.ncbi.nlm.nih.gov/pubmed/380868?dopt=AbstractPlus
51. Riess W, Stierlin H, Degen P et al. Pharmacokinetics and metabolism of the anti- inflammatory agent Voltaren. Scand J Rheumatol. 1978; (Suppl 22):17-29. http://www.ncbi.nlm.nih.gov/pubmed/353972?dopt=AbstractPlus
52. John VA. The pharmacokinetics and metabolism of diclofenac sodium (Voltarol) in animals and man. Rheumatol Rehabil. 1979; 18:(Suppl 2):22-35.
53. Willis JV, Kendall MJ, Flinn RM et al. The pharmacokinetics of diclofenac sodium following intravenous and oral administration. Eur J Clin Pharmacol. 1979; 16:405-10. http://www.ncbi.nlm.nih.gov/pubmed/527637?dopt=AbstractPlus
54. Willis JV, Kendall MJ, Jack DB. The influence of food on the absorption of diclofenac after single and multiple oral doses. Eur J Clin Pharmacol. 1981; 19:33-7. http://www.ncbi.nlm.nih.gov/pubmed/7461021?dopt=AbstractPlus
55. Willis JV, Jack DB, Kendall MJ et al. The influence of food on the absorption of diclofenac as determined by the urinary excretion of the unchanged drug and its major metabolites during chronic administration. Eur J Clin Pharmacol. 1981; 19:39-44. http://www.ncbi.nlm.nih.gov/pubmed/7461022?dopt=AbstractPlus
56. Willis JV, Kendall MJ. Pharmacokinetic studies on diclofenac sodium in young and old volunteers. Scand J Rheumatol. 1978; 22(Suppl):36-41.
57. Kendall MJ, Thornhill DP, Willis JV. Factors affecting the pharmacokinetics of diclofenac sodium (Voltarol). Rheumatol Rehabil. 1979; 18(Suppl 2):38-45. http://www.ncbi.nlm.nih.gov/pubmed/424666?dopt=AbstractPlus
58. Chamouard JM, Barre J, Urien S et al. Diclofenac binding to albumin and lipoproteins in human serum. Biochem Pharmacol. 1985; 34:1695-1700. http://www.ncbi.nlm.nih.gov/pubmed/4004886?dopt=AbstractPlus
59. Wagner J, Sulc M. Bindung von diclofenac-Na (Voltaren) an serumproteine verschiedener Spezies und Interaktionen mit anderen Pharmaka. (German; with English abstract.) Akt Rheumatol. 1979; 4:153-62.
60. Crook PR, Willis JV, Kendall MJ et al. The pharmacokinetics of diclofenac sodium in patients with active rheumatoid disease. Eur J Clin Pharmacol. 1982; 21:331-4. http://www.ncbi.nlm.nih.gov/pubmed/7056279?dopt=AbstractPlus
61. Willis JV, Kendall MJ, Jack DB. A study of the effect of aspirin on the pharmacokinetics of oral and intravenous diclofenac sodium. Eur J Clin Pharmacol. 1980; 18:415-8. http://www.ncbi.nlm.nih.gov/pubmed/7439264?dopt=AbstractPlus
62. Gaucher A, Netter P, Faure G et al. Passage du diclofénac sodium dans le liquide synovial. Thérapie. 1983; 38:431-4.
63. Sioufi A, Schoeller JP, Schwarzberg C et al. Présence du diclofénac dans le plasma et le liquide synovial au cours de diverses affections rhumatismales. Gaz Med Fr. 1984; 91:88-9.
64. Benson MD, Aldo-Benson M, Brandt KD. Synovial fluid concentrations of diclofenac in patients with rheumatoid arthritis or osteoarthritis. Semin Arthritis Rheum. 1985; 15(Suppl 1):65-7. http://www.ncbi.nlm.nih.gov/pubmed/4081792?dopt=AbstractPlus
65. Liauw H, Waiter S, Lee L et al. Effects of diclofenac on synovial eicosanoid product formation in arthritis patients. J Clin Pharmacol. 1985; 25:455- 74.
66. Chan KKH, Vyas KH, Brandt KD. In vitro protein binding of diclofenac sodium in plasma and synovial fluid. J Pharm Sci. 1987; 76:105-8. http://www.ncbi.nlm.nih.gov/pubmed/3572745?dopt=AbstractPlus
67. Fowler PD, Dawes PT, John VA et al. Plasma and synovial fluid concentrations of diclofenac sodium and its hydroxylated metabolites during once-daily administration of a 100 mg slow-release formulation. Eur J Clin Pharmacol. 1986; 31:469-72. http://www.ncbi.nlm.nih.gov/pubmed/3469101?dopt=AbstractPlus
68. Fowler PD, Shadforth MF, Crook PR et al. Plasma and synovial fluid concentrations of diclofenac sodium and its major hydroxylated metabolites during long-term treatment of rheumatoid arthritis. Eur J Clin Pharmacol. 1983; 25:389-94. http://www.ncbi.nlm.nih.gov/pubmed/6628528?dopt=AbstractPlus
69. Seppala E, Nissila M, Isomaki H et al. Comparison of the effects of different anti-inflammatory drugs on synovial fluid prostanoid concentrations in patients with rheumatoid arthritis. Clin Rheumatol. 1985; 4:315-20. http://www.ncbi.nlm.nih.gov/pubmed/3864577?dopt=AbstractPlus
70. Stierlin H, Faigle JW, Sallmann A et al. Biotransformation of diclofenac sodium (Voltaren) in animals and in man: I. Isolation and identification of principal metabolites. Xenobiotica. 1979; 9:601-10. http://www.ncbi.nlm.nih.gov/pubmed/119352?dopt=AbstractPlus
71. Stierlin H, Faigle JW. Biotransformation of diclofenac sodium (Voltaren) in animals and in man. Xenobiotica. 1979; 9:611-21. http://www.ncbi.nlm.nih.gov/pubmed/119353?dopt=AbstractPlus
72. Stierlin H, Faigle JW, Colombi A. Pharmacokinetics of diclofenac sodium (Voltaren) and metabolites in patients with impaired renal function. Scand J Rheumatol. 1978; 22(Suppl):30-5.
73. Woodhouse KW, Wynne H. The pharmacokinetics of non-steroidal anti-inflammatory drugs in the elderly. Clin Pharmacokinet. 1987; 12:111-22. http://www.ncbi.nlm.nih.gov/pubmed/3549104?dopt=AbstractPlus
74. Bendix T, Schmidt I, Rasmussen KJE et al. Diclofenac (Voltaren) and ketoprofen (Orudis), in rheumatoid arthritis: a randomized double-blind multicentre trial. Curr Ther Res. 1983; 33:192-9.
75. Huntwork JC. Efficacy and safety of diclofenac compared with aspirin in the treatment of rheumatoid arthritis. Curr Ther Res. 1986; 40:576-86.
76. Keiding G, Sorensen K. A randomized, double- blind, within-patient trial of diclofenac sodium (Voltaren) and naproxen in the treatment of rheumatoid arthritis. Curr Ther Res. 1981; 29:183-92.
77. Hirsch U. Effect and tolerability of diclofenac and indomethacin administered per os and as suppositories: a comparative trial. Curr Ther Res. 1980; 28:359-66.
78. Meyers OL, Quantock OP, Joubert PG et al. A multicentre trial of Voltaren in the treatment of rheumatoid arthritis. S Afr Med J. 1974; 48:2013-7. http://www.ncbi.nlm.nih.gov/pubmed/4612752?dopt=AbstractPlus
79. Caldwell JR. Efficacy and safety of diclofenac sodium in rheumatoid arthritis: experience in the United States. Am J Med. 1986; 80(Suppl 4B):43-7. http://www.ncbi.nlm.nih.gov/pubmed/3518432?dopt=AbstractPlus
80. Zuckner J. International experience with diclofenac in rheumatoid arthritis. Am J Med. 1986; 80(Suppl 4B):39-42. http://www.ncbi.nlm.nih.gov/pubmed/3518431?dopt=AbstractPlus
81. Ward JR. Efficacy of diclofenac in osteoarthritis. Am J Med. 1986; 80(Suppl 4B):53-7. http://www.ncbi.nlm.nih.gov/pubmed/3518434?dopt=AbstractPlus
82. Altman R. International experiences with diclofenac in osteoarthritis. Am J Med. 1986; 80(Suppl 4B):48-52. http://www.ncbi.nlm.nih.gov/pubmed/3518433?dopt=AbstractPlus
83. Amundsen T, Bleken L, Borkje B et al. Variation in response to naproxen and diclofenac in patients with osteoarthritis. Curr Ther Res. 1983; 33:793-801.
84. Germain BF. A placebo-controlled study of diclofenac sodium for the treatment of osteoarthritis of the hip and knee. Curr Ther Res. 1985; 37:259-68.
85. Schubiger BI, Ciccolunghi SN, Tanner K. Once daily dose treatment with a non-steroidal anti- rheumatic drug (diclofenac) in osteoarthrosis. J Int Med Res. 1980; 8:167-74. http://www.ncbi.nlm.nih.gov/pubmed/6989687?dopt=AbstractPlus
86. Vetter G. A comparison of naproxen and diclofenac sodium in the treatment of osteoarthritis in elderly patients. Br J Clin Pract. 1985; 39:276-281. http://www.ncbi.nlm.nih.gov/pubmed/3896286?dopt=AbstractPlus
87. Eidsaunet W, Borkje B, Larsen S et al. Response to two NSAIDs: diclofenac and naproxen in rheumatoid arthritis. Curr Ther Res. 1983; 33:966-75.
88. Lizarazo PH, Cortes MP. Single-blind parallel study comparing naproxen with sulindac and with diclofenac in rheumatoid arthritis. Curr Ther Res. 1983; 34:701-7.
89. Siraux P. Diclofenac (Voltaren) for the treatment of osteo-arthrosis: a double-blind comparison with naproxen. J Int Med Res. 1977; 5:169-74. http://www.ncbi.nlm.nih.gov/pubmed/330288?dopt=AbstractPlus
90. Crook PR, Fowler PD, Hothersall TE et al. A study of the efficacy and tolerability of diclofenac and ibuprofen in osteoarthritis of the hip. Br J Clin Pract. 1981; 35:309-12. http://www.ncbi.nlm.nih.gov/pubmed/7034760?dopt=AbstractPlus
91. Calabro JJ. Efficacy of diclofenac in ankylosing spondylitis. Am J Med. 1986; 80(Suppl 4B):58-63. http://www.ncbi.nlm.nih.gov/pubmed/3518435?dopt=AbstractPlus
92. Kantor TG. Use of diclofenac in analgesia. Am J Med. 1986; 80(Suppl 4B):64-9. http://www.ncbi.nlm.nih.gov/pubmed/2939715?dopt=AbstractPlus
93. Wuolijoki E, Oikarinen VJ, Ylipaavalniemi P et al. Effective postoperative pain control by preoperative injection of diclofenac. Eur J Clin Pharmacol. 1987; 32:249-52. http://www.ncbi.nlm.nih.gov/pubmed/3595697?dopt=AbstractPlus
94. Henrikson PA, Thilander H, Wahlander LA. Absorption and effect of diclofenac-sodium after surgical removal of a lower wisdom tooth. Curr Ther Res. 1982; 31:20-6.
95. Furberg B, Lerner A, Nystrom B. Antiphlogistics in acute inflammatory conditions in the soft tissues of the musculo-skeletal system—a double blind comparison of diclofenac and indomethacin. Curr Ther Res. 1985; 38:523-27.
96. Torri G. Efficacy and tolerability of aceclofenac in the treatment of gonalgia: controlled double-blind study vs diclofenac. Curr Ther Res. 1987; 42:453-7.
97. Van Heerden JJ. Diclophenac sodium, oxyphenbutazone and placebo in sports injuries of the knee. S Afr Med J. 1977; 52:396-9. http://www.ncbi.nlm.nih.gov/pubmed/331503?dopt=AbstractPlus
98. Lundstam SOA, Leissner KH, Wahlander LA et al. Prostaglandin-synthetase inhibition with diclofenac sodium in treatment of renal colic: comparison with use of a narcotic analgesic. Lancet. 1982; 1:1096-97. http://www.ncbi.nlm.nih.gov/pubmed/6122892?dopt=AbstractPlus
99. Lundstam S, Ivarsson L, Lindblad L et al. Treatment of biliary pain by prostaglandin synthetase inhibition with diclofenac sodium. Curr Ther Res. 1985; 37:435-6.
100. Hetherington JW, Philp NH. Diclofenac sodium versus pethidine in acute renal colic. BMJ. 1986; 292:237-8. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1339208&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/3081085?dopt=AbstractPlus
101. Lundstam S, Wahlander L, Kral JG. Treatment of ureteral colic by prostaglandin synthetase inhibition with diclofenac sodium. Curr Ther Res. 1980; 28:355- 58.
102. Lundstam S, Ivarsson L, Lindblad L. Diclofenac compared with a narcotic analgesic in the treatment of biliary pain. Curr Ther Res. 1987; 42:395-99.
103. Stacher G, Steinringer H, Schneider S et al. Experimental pain induced by electrical and thermal stimulation of the skin in healthy man: sensitivity to 75 and 150 mg diclofenac sodium in comparison with 60 mg codeine and placebo. Br J Clin Pharmacol. 1986; 21:35-43. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1400805&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/3947505?dopt=AbstractPlus
104. Ingemanson CA, Sikstrom B, Bjorkman R. Comparison between diclofenac and naproxen in the treatment of primary dysmenorrhoea. Curr Ther Res. 1984; 36:1203-09.
105. Ingemanson CA, Carrington B, Sikstrom B et al. Diclofenac in the treatment of primary dysmenorrhoea. Curr Ther Res. 1981; 30:632-9.
106. Al-Waili NS. Diclofenac sodium in the treatment of primary nocturnal enuresis: double-blind crossover study. Clin Exp Pharmacol Physiol. 1986; 13:139-42. http://www.ncbi.nlm.nih.gov/pubmed/3519020?dopt=AbstractPlus
107. Abrams GJ, Solomon L, Meyers OL. A long-term study of diclophenac sodium in the treatment of rheumatoid arthritis and osteo-arthrosis. S Afr Med J. 1978; 53:442-5. http://www.ncbi.nlm.nih.gov/pubmed/354028?dopt=AbstractPlus
108. Berry H, Bloom B, Hamilton EBD. A comparative study of piroxicam (Feldene) diclofenac and placebo in osteoarthritis. Clin Trials J. 1982; 19:349-58.
109. Marcolongo R, Giordano N, Bassi GP et al. Double-blind preference and compliance multicentre study in osteoarthritis: once-a-day treatment. Clin Rheumatol. 1985; 4:267-77. http://www.ncbi.nlm.nih.gov/pubmed/3905218?dopt=AbstractPlus
110. Scharf Y, Nahir M, Schapira D et al. A comparative study of naproxen with diclofenac sodium in osteoarthrosis of the knees. Rheumatol Rehabil. 1982; 21:167-70. http://www.ncbi.nlm.nih.gov/pubmed/7048497?dopt=AbstractPlus
111. Car A, Jajic I, Krampac I et al. A double- blind multicentre comparison of diclofenac sodium and naproxen in osteoarthrosis of the hip. Scand J Rheumatol. 1978; Suppl 22:63-8.
112. Chiswell RJ, Grieve AP, MacDonald IR. An interim report on a multicentre general practice study of Voltarol: 2. Osteoarthritis. Br J Clin Pract. 1984; 34:207-10.
113. Aylward M, Maddock J, Lewis PA et al. Mefenamic acid and diclofenac sodium in osteoarthritis of the weight bearing joints: a double blind comparison. Br J Clin Pract. 1985; 39:135-9. http://www.ncbi.nlm.nih.gov/pubmed/3893502?dopt=AbstractPlus
114. Joubert PH, Kushlick AR, McNeill WG et al. South African multicentre trial with Voltaren in osteo- arthritis of the knee. S Afr Med J. 1974; 48:1973-8. http://www.ncbi.nlm.nih.gov/pubmed/4608209?dopt=AbstractPlus
115. Huskisson EC, Dieppe PA, Scott J et al. Diclofenac sodium, diflunisal and naproxen: patient preferences for anti-inflammatory drugs in rheumatoid arthritis. Rheumatol Rehabil. 1982; 21:238-42. http://www.ncbi.nlm.nih.gov/pubmed/7134745?dopt=AbstractPlus
116. Kirchheiner B, Trang L, Wollheim FA. Diclophenac sodium (Voltaren) in rheumatoid arthritis: a double-blind comparison with indomethacin and placebo. Int J Clin Pharmacol. 1976; 13:292-7.
117. Weisman MH. Double-blind randomized trial of diclofenac sodium versus placebo in patients with rheumatoid arthritis. Clin Ther. 1986; 8:427-38. http://www.ncbi.nlm.nih.gov/pubmed/3524843?dopt=AbstractPlus
118. Dürrigl T, Vitaus M, Pucar I et al. Diclofenac sodium (Voltaren): results of a multi-centre comparative trial in adult-onset rheumatoid arthritis. J Int Med Res. 1975; 3:139-44. http://www.ncbi.nlm.nih.gov/pubmed/162669?dopt=AbstractPlus
119. Tannenbaum H, Esdaile J, Topp JR et al. A double-blind, multicenter, controlled study on diclofenac (Voltaren) and naproxen in patients with rheumatoid arthritis (R.A.). Curr Ther Res. 1984; 35:357-62.
120. Nahir AM, Scharf Y. A comparative study of diclofenac and sulindac in ankylosing spondylitis. Rheumatol Rehabil. 1980; 19:193-8. http://www.ncbi.nlm.nih.gov/pubmed/6997973?dopt=AbstractPlus
121. Martinez-Elizondo P. Un estudio controlado de diclofenac sodico en reumatologia. (Spanish; with English abstract.) Invest Med Int. 1976; 3:56-60.
122. Tonachella R, Curcio CG, Grossi E. Diclofenac sodium in cancer pain: a double-blind within-patients comparison with pentazocine. Curr Ther Res. 1985; 37:1130-3.
123. Broggini M, Corbetta E, Grossi E et al. Diclofenac sodium in biliary colic: a double blind trial. BMJ. 1984; 288:1042. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1442655&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/6423186?dopt=AbstractPlus
124. Miralles R, Cami J, Gutiérrez J et al. Diclofenac versus dipyrone in acute renal colic: a double-blind controlled trial. Eur J Clin Pharmacol. 1987; 33:527-8. http://www.ncbi.nlm.nih.gov/pubmed/3322848?dopt=AbstractPlus
125. Ciccolunghi SN, Chaudri HA, Schubiger BI et al. Report on a long-term tolerability study of up to two years with diclofenac sodium (voltaren). Scand J Rheumatol. 1978; 22(Suppl):86-96.
126. Caldwell JR. Diclofenac sodium in the treatment of rheumatoid arthritis and osteoarthritis. Semin Arthritis Rheum. 1985; 15:73-9. http://www.ncbi.nlm.nih.gov/pubmed/4081794?dopt=AbstractPlus
127. Khan MA. A double blind comparison of diclofenac and indomethacin in the treatment of ankylosing spondylitis. J Rheumatol. 1987; 14:118-23. http://www.ncbi.nlm.nih.gov/pubmed/3553586?dopt=AbstractPlus
128. Haapasaari J, Wuolijoki E, Ylijoki H. Treatment of juvenile rheumatoid arthritis with diclofenac sodium. Scand J Rheumatol. 1983; 12:325- 30. http://www.ncbi.nlm.nih.gov/pubmed/6361986?dopt=AbstractPlus
129. Bijlsma A. The long-term efficacy and tolerability of Voltaren (diclofenac sodium) and indomethacin in rheumatoid arthritis. Scand J Rheumatol. 1978; 22:74-80.
130. Holman RM, Celinska E. Voltarol in the treatment of acute gout—a double-blind trial in general practice. In: Chiswell RJ, Birdwood GF, eds. Current themes in rheumatology. Cambridge, UK: Cambridge Medical Publications; 1981:14-5.
131. Alcalay M, Bussière JL, Peltier A. Le Voltarène 100 suppositoire en rhumatologie: bilan clinique a propos de 16 419 nouvelles observations recueillies par 2895 omnipraticiens en France. Gaz Med Fr. 1980; 87:2036-40.
132. Rivet JP, Richard A. Le Voltarène, anti- inflammatoire de rhumatologie: bilan clinique a propos de 10 352 observations recueillies par 2 623 omnipraticiens en France. Gaz Med Fr. 1977; 84:3547- 54.
133. Machtey I. Diclofenac in the treatment of painful joints and traumatic tendinitis (including strains and sprains): a brief review. Semin Arthritis Rheum. 1985; 15:87-92. http://www.ncbi.nlm.nih.gov/pubmed/4081796?dopt=AbstractPlus
134. Huskisson EC, Bryans R. Diclofenac sodium in the treatment of painful stiff shoulder. Curr Med Res Opin. 1983; 8:350-3. http://www.ncbi.nlm.nih.gov/pubmed/6340976?dopt=AbstractPlus
135. Vecchini L, Grossi E. Ionization with diclofenac sodium in rheumatic disorders: a double- blind placebo-controlled trial. J Int Med Res. 1984; 12:346-50. http://www.ncbi.nlm.nih.gov/pubmed/6394405?dopt=AbstractPlus
136. Famaey JP, Ginsberg F. Treatment of periarthritis of the shoulder: a comparison of ibuprofen and diclofenac. J Int Med Res. 1984; 12:238-43. http://www.ncbi.nlm.nih.gov/pubmed/6381167?dopt=AbstractPlus
137. Keinanen-Kiukaanniemi S, Simila S, Kapyla H. Antipyretic therapy: evaluation of diclofenac sodium as an antipyretic agent. Clin Ther. 1980; 2:421-6.
138. Bettini R, Grossi E, Rapazzini P et al. Diclofenac sodium versus acetylsalicylic acid: a randomized study in febrile patients. J Int Med Res. 1986; 14:95-100. http://www.ncbi.nlm.nih.gov/pubmed/3516755?dopt=AbstractPlus
139. Polman HA, Huijbers WAR, Augusteijn R. The use of diclofenac sodium (Voltaren) suppositories as an antipyretic in children with fever due to acute infections: a double-blind, between-patient, placebo- controlled study. J Int Med Res. 1981; 9:343-48. http://www.ncbi.nlm.nih.gov/pubmed/7028533?dopt=AbstractPlus
140. Riihiluoma P, Wuolijoki E, Pulkkinen MO. Treatment of primary dysmenorrhea with diclofenac sodium. Eur J Obstet Gynecol Reprod Biol. 1981; 12:189-194. http://www.ncbi.nlm.nih.gov/pubmed/7028529?dopt=AbstractPlus
141. Weinberger M. Analgesic sensitivity in children with asthma. Pediatrics. 1978; 62(Suppl):910-5. http://www.ncbi.nlm.nih.gov/pubmed/103067?dopt=AbstractPlus
142. Settipane GA. Adverse reactions to aspirin and related drugs. Arch Intern Med. 1981; 141:328-32. http://www.ncbi.nlm.nih.gov/pubmed/7008734?dopt=AbstractPlus
143. Pleskow WW, Stevenson DD, Mathison DA et al. Aspirin desensitization in aspirin-sensitive asthmatic patients: clinical manifestations and characterization of the refractory period. J Allergy Clin Immunol. 1982; 69(1 Part 1):11-9. http://www.ncbi.nlm.nih.gov/pubmed/7054250?dopt=AbstractPlus
144. VanArsdel PP Jr. Aspirin idiosyncracy and tolerance. J Allergy Clin Immunol. 1984; 73:431-3. http://www.ncbi.nlm.nih.gov/pubmed/6423718?dopt=AbstractPlus
145. Stevenson DD. Diagnosis, prevention, and treatment of adverse reactions to aspirin and nonsteroidal anti-inflammatory drugs. J Allergy Clin Immunol. 1984; 74(4 Part 2):617-22. http://www.ncbi.nlm.nih.gov/pubmed/6436354?dopt=AbstractPlus
146. Stevenson DD, Mathison DA. Aspirin sensitivity in asthmatics: when may this drug be safe? Postgrad Med. 1985; 78:111-3,116-9. (IDIS 205854)
147. Settipane GA. Aspirin and allergic diseases: a review. Am J Med. 1983; 74(Suppl):102-9. http://www.ncbi.nlm.nih.gov/pubmed/6344621?dopt=AbstractPlus
148. AMA Department of Drugs. AMA drug evaluations. 5th ed. Chicago: American Medical Association; 1983:107-38.
149. Hart FD, Huskisson EC. Non-steroidal anti- inflammatory drugs: current status and rational therapeutic use. Drugs. 1984; 27:232-55. http://www.ncbi.nlm.nih.gov/pubmed/6368185?dopt=AbstractPlus
150. Frost A. Diclofenac versus lidocaine as injection therapy in myofascial pain. Scand J Rheumatol. 1986; 15:153-6. http://www.ncbi.nlm.nih.gov/pubmed/3749828?dopt=AbstractPlus
151. Carlborg L, Lindoff CL, Hellman A. Diclofenac versus pethidine in the treatment of pain after hysterectomy. Eur J Anaesth. 1987; 4:241-7.
152. Philip PJ, Lema LEK, Carneiro PMR. A comparison of diclofenac sodium (Voltaren) and pethidine as post-operative analgesics in major elective surgical procedures. E Afr Med J. 1985; 62:666-71.
153. Lindgren U, Djupsjo H. Diclofenac for pain after hip surgery. Acta Orthop Scand. 1985; 56:28-31. http://www.ncbi.nlm.nih.gov/pubmed/3885672?dopt=AbstractPlus
154. Valtonen EJ. A comparative short-term trial with Voltaren (diclofenac sodium) and naproxen in soft-tissue rheumatism. Scand J Rheumatol. 1978; 22:69-73.
155. Catalano MA. Worldwide safety experience with diclofenac. Am J Med. 1986; 80(Suppl 4B):81-7. http://www.ncbi.nlm.nih.gov/pubmed/3518436?dopt=AbstractPlus
156. O’Brien WM. Adverse reactions to nonsteroidal anti-inflammatory drugs: diclofenac compared with other nonsteroidal anti-inflammatory drugs. Am J Med. 1986; 80(Suppl 4B):70-80.
157. Adams SS. Non-steroidal anti-inflammatory drugs, plasma half-lives, and adverse reactions. Lancet. 1987; 2:1204-5. http://www.ncbi.nlm.nih.gov/pubmed/2890822?dopt=AbstractPlus
158. Willkens RF. Worldwide clinical safety experience with diclofenac. Semin Arthritis Rheum. 1985; 15:105-10. http://www.ncbi.nlm.nih.gov/pubmed/3909410?dopt=AbstractPlus
159. Beun GDM, Leunissen KML, Van Breda Vriesman PJC et al. Isolated minimal change nephropathy associated with diclofenac. BMJ. 1987; 295:182- 3. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1247037&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/3115369?dopt=AbstractPlus
160. Schwartz J, Altshuler E, Madjar J et al. Acute renal failure associated with diclofenac treatment in an elderly woman. J Am Geriatr Soc. 1988; 36:482. http://www.ncbi.nlm.nih.gov/pubmed/3361048?dopt=AbstractPlus
161. Dunn AM, Buckley BM. Non-steroidal anti-inflammatory drugs and the kidney. BMJ. 1986; 293:202-3. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1340929&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/3089448?dopt=AbstractPlus
162. Scott SJ, Bussey RA et al. Renal papillary necrosis associated with diclofenac sodium. BMJ. 1986; 292:1050. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1340115&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/20742631?dopt=AbstractPlus
163. Dunk AA, Walt RP, Jenkins WJ et al. Diclofenac hepatitis. BMJ. 1982; 284:1605-6. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1498512&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/6805622?dopt=AbstractPlus
164. Breen EG, McNicholl J, Cosgrove E et al. Fatal hepatitis associated with diclofenac. Gut. 1986; 27:1390-3. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1434053&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/3792922?dopt=AbstractPlus
165. Japanese Ministry of Health and Welfare. Diclofenac sodium. Jpn Med Gaz. 1978; 15:10.
166. Michalevicz R, Seligsohn U. Clinical bleeding due to diclofenac (Voltaren). Arthritis Rheum. 1982; 25:599. http://www.ncbi.nlm.nih.gov/pubmed/7082409?dopt=AbstractPlus
167. Palmer JF. Letter sent to Moscaritola JD of Geigy Pharmaceuticals regarding labeling revisions about gastrointestinal adverse reactions to Voltaren (diclofenac). Rockville, MD: Food and Drug Administration, Division of Oncology and Radiopharmaceutical Drug Products. 1988 Sep.
168. Szczeklik A, Gryglewski RJ, Czerniawska-Mysik G et al. Asthmatic attacks induced in aspirin-sensitive patients by diclofenac and naproxen. Br Med J. 1977; 2:231-2. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1631372&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/406961?dopt=AbstractPlus
169. Morris BAP, Remtulla SS. Erythema multiforme major following use of diclofenac. Can Med Assoc J. 1985; 133:665. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1346267&blobtype=pdf
170. Blekkenhorst GH, Cook ES, Eales L. Drug safety in porphyria. Lancet. 1980; 1:1367. http://www.ncbi.nlm.nih.gov/pubmed/6104166?dopt=AbstractPlus
171. Oates JA, FitzGerald GA, Branch RA et al. Clinical implications of prostaglandin and thromboxane A2 formation (second of two parts). N Engl J Med. 1988; 319:761-7. http://www.ncbi.nlm.nih.gov/pubmed/3045551?dopt=AbstractPlus
172. Vale JA, Meredith TJ. Acute poisoning due to non-steroidal anti-inflammatory drugs: clinical features and management. Med Toxicol. 1986; 1:12-31. http://www.ncbi.nlm.nih.gov/pubmed/3537613?dopt=AbstractPlus
173. Koopmans PP, Thien T, Gribnau FWJ. The influence of ibuprofen, diclofenac and sulindac on the blood pressure lowering effect of hydrochlorothiazide. Eur J Clin Pharmacol. 1987; 31:553-7. http://www.ncbi.nlm.nih.gov/pubmed/3549320?dopt=AbstractPlus
174. Harkönen M, Ekblom-Kullberg S. Reversible deterioration of renal function after diclofenac in patient receiving triamterene. BMJ. 1986; 293:698-9. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1341548&blobtype=pdf
175. Gabrielli A, Leoni P, Danieli G. Methotrexate and non-steroidal anti-inflammatory drugs. BMJ. 1987; 294:776. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1245843&blobtype=pdf
176. Reimann IW, Frölich JC. Effects of diclofenac on lithium kinetics. Clin Pharmacol Ther. 1981; 30:348-52. http://www.ncbi.nlm.nih.gov/pubmed/7273598?dopt=AbstractPlus
177. Faigle JW, Böttcher I, Godbillon J et al. A new metabolite of diclofenac sodium in human plasma. Xenobiotica. 1988; 18:1191-7. http://www.ncbi.nlm.nih.gov/pubmed/3266538?dopt=AbstractPlus
178. Derendorf H, Mullersman G, Barth J et al. Pharmacokinetics of diclofenac sodium after intramuscular administration in combination with triamcinolone acetate. Eur J Clin Pharmacol. 1986; 31:363-5. http://www.ncbi.nlm.nih.gov/pubmed/3792436?dopt=AbstractPlus
179. Brater DC. Drug-drug and drug-disease interactions with nonsteroidal anti-inflammatory drugs. Am J Med. 1986; 80(Suppl 1A):62-70. http://www.ncbi.nlm.nih.gov/pubmed/3511686?dopt=AbstractPlus
180. D’Arcy PF. Drug interactions with new drugs. Pharm Int. 1983; 4:285-91.
181. Food and Drug Administration. Labeling revisions for NSAIDs. FDA Drug Bull. 1989; 19:3-4.
182. Court H, Volans GN. Poisoning after overdose with non-steroidal anti-inflammatory drugs. Adv Drug React Ac Pois Rev. 1984; 3:1-21.
183. Segev S, Rehavi M, Rubinstein E. Quinolones, theophylline, and diclofenac interactions with the γ- aminobutyric acid receptor. Antimicrob Agents Chemother. 1988; 32:1624-6. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=175940&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/2855295?dopt=AbstractPlus
184. Müller FO, Hundt HKL, Müller DG. Pharmacokinetic and pharmacodynamic implications of long-term administration of non-steroidal anti- inflammatory agents. Int J Clin Pharmacol. 1977; 15:397-402.
185. Rossi E, Ferraccioli GF, Cavalieri F et al. Diclofenac-associated acute renal failure. Nephron. 1985; 40:491-3. http://www.ncbi.nlm.nih.gov/pubmed/4022222?dopt=AbstractPlus
186. Zandstra DF, Stoutenbeek CP, Alexander JP. Antipyretic therapy with diclofenac sodium. Intensive Care Med. 1983; 9:21-3. http://www.ncbi.nlm.nih.gov/pubmed/6833624?dopt=AbstractPlus
187. Deakin M et al. Small bowel perforation associated with an excessive dose of slow release diclofenac sodium. BMJ. 1988; 297:488-9.
188. Kanaya T, Kanda A, Saeki T et al. A case of lithium intoxication caused by diclofenac. Seishin Igaku. 1988; 30:919-21.
189. Anon. Diclofenac. Med Lett Drugs Ther. 1988; 30:109-11. http://www.ncbi.nlm.nih.gov/pubmed/3054450?dopt=AbstractPlus
190. Merck Sharp & Dohme. Indocin prescribing information. West Point, PA; 1985 Oct.
191. Clive DM, Stoff JS. Renal syndromes associated with nonsteroidal antiinflammatory drugs. N Engl J Med. 1984; 310:563-72. http://www.ncbi.nlm.nih.gov/pubmed/6363936?dopt=AbstractPlus
192. Capetola RJ, Rosenthale ME, Dubinsky B et al. Peripheral antialgesics: a review. J Clin Pharmacol. 1983; 23:545-56. http://www.ncbi.nlm.nih.gov/pubmed/6363465?dopt=AbstractPlus
193. Bernheim HA, Block LH, Atkins E. Fever: pathogenesis, pathophysiology, and purpose. Ann Intern Med. 1979; 91:261-70. http://www.ncbi.nlm.nih.gov/pubmed/223485?dopt=AbstractPlus
194. Schweizer A, Brom R. Differentiation of peripheral and central effects of analgesic drugs. Int J Tissue React. 1985; 7:79-83. http://www.ncbi.nlm.nih.gov/pubmed/4008177?dopt=AbstractPlus
195. Corli O, Sargentoni A, Catania S et al. Impiego di un F.A.N.S. (diclofenac sodico) in neuroleptoanalgesia: studio preliminare aperto. Giorn Chir. 1986; 7:1613-8.
196. Netter P, Lambert H, Larcan A et al. Diclofenac sodium-chlormezanone poisoning. Eur J Clin Pharmacol. 1984; 26:535-6. http://www.ncbi.nlm.nih.gov/pubmed/6734713?dopt=AbstractPlus
197. Ciprofloxacin hydrochloride: reviewers’ comments (personal observations). 1988 Oct.
198. Hori S, Shimada J, Saito A et al. A study on enhanced epileptogenicity of new quinolones in the presence of anti-inflammatory drugs. Proceedings of ICAAC New York 1987. Abstract No. 30.
199. McNeil Pharmaceutical. Tolectin DS and Tolectin prescribing information. Spring House, PA; 1985 Aug.
200. The Upjohn Company. Motrin prescribing information. Kalamazoo, MI; 1985 Jul.
201. Michot F, Ajdacic K, Glaus L. A double-blind clinical trial to determine if an interaction exists between diclofenac sodium and the oral anticoagulant acenocoumarol (Nicoumalone). J Int Med Res. 1975; 3:153-7. http://www.ncbi.nlm.nih.gov/pubmed/162671?dopt=AbstractPlus
202. Bird HA, Hill J, Letham P et al. A study to determine the clinical relevance of the pharmacokinetic interaction between aspirin and diclofenac. Agents Actions. 1986; 18:447-9. http://www.ncbi.nlm.nih.gov/pubmed/3529884?dopt=AbstractPlus
203. Hamor GH. Nonsteroidal anti-inflammatory drugs. In: Foye WO, ed. Principles of medicinal chemistry. 3rd ed. Philadelphia: Lea & Febiger; 1989:503-30.
204. Wilson DE. Antisecretory and mucosal protective actions of misoprostol: potential role in the treatment of peptic ulcer disease. Am J Med. 1987; 83:2-8. http://www.ncbi.nlm.nih.gov/pubmed/3113241?dopt=AbstractPlus
205. Aadland E, Fausa O, Vatn M et al. Protection by misoprostol against naproxen-induced gastric mucosal damage. Am J Med. 1987; 83(Suppl 1A):37-40. http://www.ncbi.nlm.nih.gov/pubmed/3113244?dopt=AbstractPlus
206. Grossi E, Broggini M, Quaranta M et al. Different pharmacological approaches to the treatment of acute biliary colic. Curr Ther Res. 1986; 40:876- 82.
207. International Agranulocytosis and Aplastic Anemia Study. Risks of agranulocytosis and aplastic anemia: a first report of their relation to drug use with special reference to analgesics. JAMA. 1986; 256:1749-57. http://www.ncbi.nlm.nih.gov/pubmed/3747087?dopt=AbstractPlus
208. Zimmerer J, Tittor W, Degen P. Rheuma-therapie bei Leberkranken. (German; with English abstract.) Fortschr Med. 1982; 100:1683-8.
209. Llorca G, Larbre JP, Collet P et al. Changing the class of NSAID in cases of hepatotoxicity. Ann Rheum Dis. 1988; 47:791. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1003601&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/3178321?dopt=AbstractPlus
210. Leak AM, Richter MR, Clemens LE et al. A crossover study of naproxen, diclofenac and tolmetin in seronegative juvenile chronic arthritis. Clin Exp Rheumatol. 1988; 6:157-60. http://www.ncbi.nlm.nih.gov/pubmed/3052965?dopt=AbstractPlus
211. Minotti V, Patoia L, Roila F et al. Double- blind evaluation of analgesic efficacy of orally administered diclofenac, nefopam, and acetylsalicylic acid (ASA) plus codeine in chronic cancer pain. Pain. 1989; 36:177-83. http://www.ncbi.nlm.nih.gov/pubmed/2645561?dopt=AbstractPlus
212. Schwarz A, Krause PH, Keller F et al. Granulomatous interstitial nephritis after nonsteroidal anti-inflammatory drugs. Am J Nephrol. 1988; 8:410-6. http://www.ncbi.nlm.nih.gov/pubmed/3071148?dopt=AbstractPlus
213. Duncan JJ, Farr JE. Comparison of diclofenac sodium and aspirin in the treatment of acute sports injuries. Am J Sports Med. 1988; 16:656-9. http://www.ncbi.nlm.nih.gov/pubmed/3149152?dopt=AbstractPlus
214. Lascar G, Grippon P, Lévy VG. Hépatite aigue mortelle au cours d’un traitement par le diclofenac (Voltarène). Gastroenterol Clin Biol. 1984; 8:881- 2. http://www.ncbi.nlm.nih.gov/pubmed/6526249?dopt=AbstractPlus
215. Yinnon AM, Moreb JS, Slotki IN. Nephrotic syndrome associated with diclofenac sodium. BMJ. 1987; 295:556. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1247465&blobtype=pdf
216. Gabrielsen TO, Staerfelt F, Thune PO. Drug- induced bullous dermatosis with linear IgA deposits along the basement membrane. Acta Derm Venereol. 1981; 61:439-41. http://www.ncbi.nlm.nih.gov/pubmed/6172936?dopt=AbstractPlus
217. Morris BAP, Remtulla SS. Erythema multiforme major following use of diclofenac. Can Med Assoc J. 1985; 133:665. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1346267&blobtype=pdf
218. Ehsanullah RS, Page MC, Tildesley G et al. Prevention of gastroduodenal damage induced by non-steroidal anti-inflammatory drugs: controlled trial of ranitidine. BMJ. 1988; 297:1017-21. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1834765&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/3142593?dopt=AbstractPlus
219. Parapia L, Cox JA. Spontaneous platelet aggregation after diclofenac treatment. BMJ. 1984; 288:368. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1444246&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/20742168?dopt=AbstractPlus
220. Alcalay M, Thomas P, Reboux JF et al. Myoclonies au cours d’un traitement par le diclofenac. Sem Hop Paris. 1979; 55:679-80. http://www.ncbi.nlm.nih.gov/pubmed/224483?dopt=AbstractPlus
221. Anon. NSAIDs for renal and biliary colic: intramuscular diclofenac. Drug Ther Bull. 1987; 25:85-6. http://www.ncbi.nlm.nih.gov/pubmed/3315540?dopt=AbstractPlus
222. Flygare U, Seuri M, Hurme J et al. Relief of spasm with diclofenac. Clin Rheum. 1988; 7:124-5.
223. Schapira D, Bassan L, Nahir AM et al. Diclofenac-induced hepatotoxicity. Postgrad Med J. 1986; 62:63-5. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=2418538&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/3797366?dopt=AbstractPlus
224. Joris J, Reuter AM, Vrindts-Gevaert Y et al. Effect of diclofenac on plasma levels of immunoreactive prolactin, follicle stimulating hormone, luteinizing hormone, thyrotropin, and β-endorphin in humans. Hormone Res. 1988; 29:143-6. http://www.ncbi.nlm.nih.gov/pubmed/2975630?dopt=AbstractPlus
225. Kramer MR, Levene C, Hershko C. Severe reversible autoimmune haemolytic anaemia and thrombocytopenia associated with diclofenac therapy. Scand J Haematol. 1986; 36:118-20. http://www.ncbi.nlm.nih.gov/pubmed/3952461?dopt=AbstractPlus
226. Szczeklik A, Gryglewski RJ, Czerniawska-Mysik G et al. Asthmatic attacks induced in aspirin-sensitive patients by diclofenac and naproxen. Br Med J. 1977; 2:231-2. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1631372&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/406961?dopt=AbstractPlus
227. Bioglan Pharma Inc. Solaraze (diclofenac sodium 3%) topical gel prescribing information. Malvern, PA: 2001 Jun 1.
228. Borghi C, Del Corno C, Palummeri C et al. Pharmacokinetics, efficacy and safety of diclofenac: elderly vs non elderly arthritic patients. Acta Pharmacol Toxicol (Copenh). 1986; 59(Suppl 5):101.
229. Samuelson CO Jr, Williams HJ. Ibuprofen- associated aseptic meningitis in systemic lupus erythematosus. West J Med. 1979; 131:57-9. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1271636&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/483800?dopt=AbstractPlus
230. Widener HL, Littman BH. Ibuprofen-induced meningitis in systemic lupus erythematosus. JAMA. 1978; 239:1062-4. http://www.ncbi.nlm.nih.gov/pubmed/304902?dopt=AbstractPlus
231. Ballas ZK, Donta ST. Sulindac-induced aseptic meningitis. Arch Intern Med. 1982; 142:165-6. http://www.ncbi.nlm.nih.gov/pubmed/7053720?dopt=AbstractPlus
232. Geigy Pharmaceuticals. Butazolidin prescribing information. In: Huff BB, ed. Physician’s desk reference. 43rd ed. Oradell, NJ: Medical Economics Company, Inc; 1989:964-6.
233. Mandell B, Shen HS, Hepburn B. Fever from ibuprofen in a patient with lupus erythematosus. Ann Intern Med. 1976; 85:209-10. http://www.ncbi.nlm.nih.gov/pubmed/942146?dopt=AbstractPlus
234. Harima Y, Maekawa T, Miyauchi Y et al. Intoxication with sulindac, tiaramide hydrochloride and diclofenac sodium. Intensive Care Med. 1987; 13:361- 2. http://www.ncbi.nlm.nih.gov/pubmed/3655104?dopt=AbstractPlus
235. Ellenhorn MJ, Barceloux DG. Enhancement of elimination. In: Medical toxicology: diagnosis and treatment of human poisoning. New York: Elsevier; 1988:66-72.
236. American Pharmaceutical Association. Evaluations of drug interactions. 3rd ed. Washington, DC: American Pharmaceutical Association; 1985:458.
237. Hansten PD. Drug interactions. 5th ed. Philadelphia: Lea & Febiger; 1985:402,408.
238. Lithium-ibuprofen; lithium-indomethacin; lithium-naproxen; lithium-piroxicam. In: Tatro DS, Olin BR, eds. Drug interaction facts. St. Louis: JB Lippincott Co; 1988(Apr):458,459,463,464.
239. Schumacher A, Faust-Tinnefeldt G, Geissler H et al. Voltaren in co-medication. In: Kass, ed. Voltaren—new findings. Bern, Switzerland: Hans Huber Publishers; 1982:31-38.
240. Terhaag B, le Petit G, Richter K et al. Zur Beziehung von in-vitro- und in-vivo-Untersuchungen beim Menschen am Beispiel von Diclofenac-Suppositorien. (German; with English abstract.) Pharmazie. 1985; 40:784-6.
241. Ruppert GB, Barth WF. Tolmetin-induced aseptic meningitis. JAMA. 1982; 245:67-68.
242. Morimoto K, Iwamoto Y, Katashima T et al. Absorption and bioavailability of diclofenac after rectal administration of diclofen-Na gel preparation in rat and man. Pharm Res. 1985; 4:166-70.
243. Wasner CK. Ibuprofen, meningitis, and systemic lupus erythematosus. J Rheumatol. 1978; 5:162-64. http://www.ncbi.nlm.nih.gov/pubmed/671432?dopt=AbstractPlus
244. Favre L, Glasson P, Vallotton MB. Reversible acute renal failure from combined triamterene and indomethacin. Ann Intern Med. 1982; 96:317-20. http://www.ncbi.nlm.nih.gov/pubmed/6949485?dopt=AbstractPlus
245. Weinberg MS, Quigg RJ, Salant DJ et al. Anuric renal failure precipitated by indomethacin and triamterene. Nephron. 1985; 40:216-8. http://www.ncbi.nlm.nih.gov/pubmed/4000350?dopt=AbstractPlus
246. Smith Kline & French. Dyrenium prescribing information. In: Huff BB, ed. Physicians’ desk reference. 43rd ed. Oradell, NJ: Medical Economics Company, Inc; 1989:2051-2.
247. Dapas F (Geigy, Ardsley, NY): Personal communication; 1989 Jul.
248. Reviewers’ comments (personal observations); 1989 Jul.
249. American College of Rheumatology Subcommittee on Rheumatoid Arthritis Guidelines. Guidelines for the management of rheumatoid arthritis: 2002 update. Arthritis Rheum. 2002; 46:328-46. http://www.ncbi.nlm.nih.gov/pubmed/11840435?dopt=AbstractPlus
250. Searle. Cytotec (misoprostol) prescribing information. 1989 Jan.
251. Hart FD. Rheumatic disorders. In: Avery GS, ed. Drug treatment: principles and practice of clinicial pharmacology and therapeutics. 3rd ed. New York: ADIS Press; 1987:910-57.
252. McCarthy JT, Torres VE, Romero JC et al. Acute intrinsic renal failure induced by indomethacin: role of prostaglandin synthetase inhibition. Mayo Clin Proc. 1982; 57:289-96. http://www.ncbi.nlm.nih.gov/pubmed/6952058?dopt=AbstractPlus
253. Mazeika PK, Ford MJ. Chronic active hepatitis associated with diclofenac sodium therapy. Br J Clin Pract. 1989; 43:125-6. http://www.ncbi.nlm.nih.gov/pubmed/2611118?dopt=AbstractPlus
254. Anon. Drugs for rheumatoid arthritis. Treat Guidel Med Lett. 2005; 3;83-90.
255. Helfgott SM, Sandberg-Cook J, Zakim D et al. Diclofenac-associated hepatotoxicity. JAMA. 1990; 264:2660-2. http://www.ncbi.nlm.nih.gov/pubmed/2232043?dopt=AbstractPlus
256. Carson J, Notis WM, Orris ES. Colonic ulceration and bleeding during diclofenac therapy. N Engl J Med. 1990; 323:135. http://www.ncbi.nlm.nih.gov/pubmed/2359424?dopt=AbstractPlus
257. Bernstein J. Colonic ulceration and bleeding during diclofenac therapy. N Engl J Med. 1990; 323:135.
258. Khazan V, Toth M, Mutgi A. Diclofenac sodium and bruising. Ann Intern Med. 1990; 112:472-3. http://www.ncbi.nlm.nih.gov/pubmed/2310112?dopt=AbstractPlus
259. Soll AH, Weinstein WM, Kurata J et al. Nonsteroidal anti-inflammatory drugs and peptic ulcer disease. Ann Intern Med. 1991; 114:307-19. http://www.ncbi.nlm.nih.gov/pubmed/1987878?dopt=AbstractPlus
260. Singh G, Triadafilopoulos G. Epidemiology of NSAID induced gastrointestinal complications. J Rheumatol. 1999; 26(Suppl 56):18-24.
261. Khalil H, Molinary E, Stoller JK. Diclofenac (Voltaren)–induced eosinophilic pneumonitis: case report and review of the literature. Arch Intern Med. 1993; 153:1649-52. http://www.ncbi.nlm.nih.gov/pubmed/8333802?dopt=AbstractPlus
262. Catella-Lawson F, Reilly MP, Kapoor SC et al. Cyclooxygenase inhibitors and the antiplatelet effects of aspirin. N Engl J Med. 2001; 345:1809-17. http://www.ncbi.nlm.nih.gov/pubmed/11752357?dopt=AbstractPlus
263. The United States Pharmacopeial Convention, Inc. Diclofenac sodium delayed-release tablets. Pharmacopeial Forum. 1993; 19:5991.
264. Ciba. Voltaren Ophthalmic (diclofenac sodium 0.1%) prescribing information. In: Physicians’ desk reference for ophthalmology. 21st ed. Montvale, NJ: Medical Economics Company Inc; 1993:273-4.
265. Stein G, Robertson M, Nadarajah J. Toxic interactions between lithium and non-steroidal anti-inflammatory drugs. Psych Med. 1988; 18:535-43.
266. Corticosteroid interactions: nonsteroidal anti-inflammatory drugs (NSAIDs). In: Hansten PD, Horn JR. Drug interactions and updates. Vancouver, WA: Applied Therapeutics, Inc; 1993:562.
267. Garcia Rodriguez LA, Jick H. Risk of upper gastrointestinal bleeding and perforation associated with individual non-steroidal anti-inflammatory drugs. Lancet. 1994; 343:769-72. http://www.ncbi.nlm.nih.gov/pubmed/7907735?dopt=AbstractPlus
268. Langman MJS, Weil J, Wainwright P et al. Risks of bleeding peptic ulcer associated with individual non-steroidal anti-inflammatory drugs. Lancet. 1994; 343:1075-8. http://www.ncbi.nlm.nih.gov/pubmed/7909103?dopt=AbstractPlus
269. Bateman DN. NSAIDs: time to re-evaluate gut toxicity. Lancet. 1994; 343:1051-2. http://www.ncbi.nlm.nih.gov/pubmed/7909094?dopt=AbstractPlus
270. Hollander D. Gastrointestinal complications of nonsteroidal anti-inflammatory drugs: prophylactic and therapeutic strategies. Am J Med. 1994; 96:274-81. http://www.ncbi.nlm.nih.gov/pubmed/8154516?dopt=AbstractPlus
271. Schubert TT, Bologna SD, Nensey Y et al. Ulcer risk factors: interaction between Helicobacter pylori infection, nonsteroidal use, and age. Am J Med. 1993; 94:413-8. http://www.ncbi.nlm.nih.gov/pubmed/8475935?dopt=AbstractPlus
272. Shorr RI, Ray WA, Daugherty JR et al. Concurrent use of nonsteroidal anti-inflammatory drugs and oral anticoagulants places elderly persons at high risk for hemorrhagic peptic ulcer disease. Arch Intern Med. 1993; 153:1665-70. http://www.ncbi.nlm.nih.gov/pubmed/8333804?dopt=AbstractPlus
273. Piper JM, Ray WA, Daugherty JR et al. Corticosteroid use and peptic ulcer disease: role of nonsteroidal anti-inflammatory drugs. Ann Intern Med. 1991; 114:735-40. http://www.ncbi.nlm.nih.gov/pubmed/2012355?dopt=AbstractPlus
274. Ciba-Geigy, Ardsley, NY; Personal communication.
275. Dawood MY. Dysmenorrhoea and prostaglandins: pharmacological and therapeutic considerations. Drugs. 1981; 22:42-56. http://www.ncbi.nlm.nih.gov/pubmed/6790261?dopt=AbstractPlus
276. Verstraeten A, Bakshi R. Diclofenac potassium for the treatment of traumatic joint distortions: an open multicentre study. J Int Med Res. 1991; 19:165-70. http://www.ncbi.nlm.nih.gov/pubmed/1864453?dopt=AbstractPlus
277. Morán M. Double-blind comparison of diclofenac potassium, ibuprofen and placebo in the treatment of ankle sprains. J Int Med Res. 1991; 19:121-30. http://www.ncbi.nlm.nih.gov/pubmed/1864448?dopt=AbstractPlus
278. Morán M. An observer-blind comparison of diclofenac potassium, piroxicam and placebo in the treatment of ankle sprains. Curr Med Res Opin. 1990; 12:268-74. http://www.ncbi.nlm.nih.gov/pubmed/2127562?dopt=AbstractPlus
279. Bahamonde LA, Saavedra H. Comparison of the analgesic and anti-inflammatory effects of diclofenac potassium versus piroxicam versus placebo in ankle sprain patients. J Int Med Res. 1990; 18:104-11. http://www.ncbi.nlm.nih.gov/pubmed/2111251?dopt=AbstractPlus
280. Alkhawajah AM, Eifawal M, Mahmoud SF. Fatal anaphylactic reaction to diclofenac. Forensic Sci Int. 1993; 60:107-10. http://www.ncbi.nlm.nih.gov/pubmed/8340033?dopt=AbstractPlus
281. George S, Rahi AHS. Thrombocytopenia associated with diclofenac therapy. Am J Health-Sys Pharm. 1995; 52:420-1.
282. Bateman DN, Kennedy JG. Non-steroidal anti-inflammatory drugs and elderly patients: the medicine may be worse than the disease. BMJ. 1995; 310:817-8. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=2549212&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/7711609?dopt=AbstractPlus
283. Nonsteroidal anti-inflammatory drug interactions: lithium-diclofenac. In: Hansten PD, Horn JR. Drug interactions and updates. Vancouver, WA: Applied Therapeutics, Inc; 1993:607.
284. Pfizer. Arthrotec (diclofenac sodium and misoprostol tablets) prescribing information. New York, NY; 2020 Dec.
285. Hawkey CJ. COX-2 inhibitors. Lancet. 1999; 353:307-14. http://www.ncbi.nlm.nih.gov/pubmed/9929039?dopt=AbstractPlus
286. Kurumabail RG, Stevens AM, Gierse JK et al. Structural basis for selective inhibition of cyclooxygenase-2 by anti-inflammatory agents. Nature. 1996; 384:644-8. http://www.ncbi.nlm.nih.gov/pubmed/8967954?dopt=AbstractPlus
287. Riendeau D, Charleson S, Cromlish W et al. Comparison of the cyclooxygenase-1 inhibitory properties of nonsteroidal anti-inflammatory drugs (NSAIDs) and selective COX-2 inhibitors, using sensitive microsomal and platelet assays. Can J Physiol Pharmacol. 1997; 75:1088-95. http://www.ncbi.nlm.nih.gov/pubmed/9365818?dopt=AbstractPlus
288. DeWitt DL, Bhattacharyya D, Lecomte M et al. The differential susceptibility of prostaglandin endoperoxide H synthases-1 and -2 to nonsteroidal anti-inflammatory drugs: aspirin derivatives as selective inhibitors. Med Chem Res. 1995; 5:325-43.
289. Cryer B, Dubois A. The advent of highly selective inhibitors of cyclooxygenase—a review. Prostaglandins Other Lipid Mediators. 1998; 56:341-61. http://www.ncbi.nlm.nih.gov/pubmed/9990677?dopt=AbstractPlus
290. Simon LS. Role and regulation of cyclooxygenase-2 during inflammation. Am J Med. 1999; 106(Suppl 5B):37-42S.
291. Morrison BW, Daniels SE, Kotey P et al. Rofecoxib, a specific cyclooxygenase-2 inhibitor, in primary dysmenorrhea: a randomized controlled study. Obstet Gynecol. 1999; 94:504-8. http://www.ncbi.nlm.nih.gov/pubmed/10511349?dopt=AbstractPlus
292. Wolfe MM, Lichtenstein DR, Singh G. Gastrointestinal toxicity of nosteroidal antiinflammatory drugs. N Engl J Med. 1999; 340:1888-99. http://www.ncbi.nlm.nih.gov/pubmed/10369853?dopt=AbstractPlus
293. Lanza FL, and the members of the Ad Hoc Committee on Practice Parameters of the American College of Gastroenterology. A guideline for the treatment and prevention of NSAID-induced ulcers. Am J Gastroenterol. 1998; 93:2037-46. http://www.ncbi.nlm.nih.gov/pubmed/9820370?dopt=AbstractPlus
294. in’t Veld BA, Ruitenberg A, Hofman A et al. Nonsteroidal antiinflammatory drugs and the risk of Alzheimer’s disease. N Engl J Med. 2001; 345:1515-21. http://www.ncbi.nlm.nih.gov/pubmed/11794217?dopt=AbstractPlus
295. Breitner JCS, Zandi PP. Do nonsteroidal antiinflammatory drugs reduce the risk of Alzheimer’s disease? N Engl J Med. 2001; 345:1567-8. Editorial.
296. McGeer PL, Schulzer M, McGeer EG. Arthritis and anti-inflammatory agents as possible protective factors for Alzheimer’s disease: a review of 17 epidemiologic studies. Neurology. 1996; 47:425-32. http://www.ncbi.nlm.nih.gov/pubmed/8757015?dopt=AbstractPlus
297. Beard CM, Waring SC, O’Brien PC et al. Nonsteroidal anti-inflammatory drug use and Alzheimer’s disease : a case-control study in Rochester, Minnesota, 1980 through 1984. Mayo Clin Proc. 1998; 73:951-5. http://www.ncbi.nlm.nih.gov/pubmed/9787743?dopt=AbstractPlus
298. in’t Veld BA, Launer LJ, Hoes AW et al. NSAIDs and incident Alzheimer’s disease: the Rotterdam Study. Neurobiol Aging. 1998; 19:607-11. http://www.ncbi.nlm.nih.gov/pubmed/10192221?dopt=AbstractPlus
299. Stewart WF, Kawas C, Corrada M et al. Risk of Alzheimer’s disease and duration of NSAID use. Neurology. 1997; 48:626-32. http://www.ncbi.nlm.nih.gov/pubmed/9065537?dopt=AbstractPlus
300. Pharmacia. Daypro (oxaprozin) caplets prescribing information. Chicago, IL; 2002 May.
301. Chan FKL, Hung LCT, Suen BY et al. Celecoxib versus diclofenac and omeprazole in reducing the risk of recurrent ulcer bleeding in patients with arthritis. N Engl J Med. 2002; 347:2104-10. http://www.ncbi.nlm.nih.gov/pubmed/12501222?dopt=AbstractPlus
302. Oceanside Pharmaceuticals. Diclofenac sodium extended-release tablets prescribing information. Bridgewater, NJ; 2020 Nov.
303. Mylan Pharmaceuticals. Diclofenac potassium film-coated tablets prescribing information. Morgantown, WV; 2020 Oct.
304. US Food and Drug Administration. Proposed NSAID Package Insert Labeling Template 1. From the FDA web site. Accessed 10 Oct 2005. http://www.fda.gov/downloads/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm106230.pdf
305. Food and Drug Administration. Analysis and recommendations for agency action regarding non-steroidal anti-inflammatory drugs and cardiovascular risk. 2005 Apr 6.
306. Novartis Pharmaceuticals. Diovan (valsartan) capsules prescribing information (dated 1997 Apr). In: Physicians’ desk reference. 53rd ed. Montvale, NJ: Medical Economics Company Inc; 1999:2013-5.
307. Novartis. Voltaren (diclofenac sodium delayed-release [enteric-coated] tablets), Voltaren-XR (diclofenac sodium extended-release tablets), and Cataflam (diclofenac potassium immediate-release tablets) prescribing information (dated 2000 May). In: Physicians’ desk reference. 56th ed. Montvale, NJ: Medical Economics Company Inc; 2002:2315-19.
308. Cush JJ. The safety of COX-2 inhibitors: deliberations from the February 16-18, 2005, FDA meeting. From the American College of Rheumatology website. Accessed 2005 Oct 12. http://www.rheumatology.org
309. Graham DY. NSAIDs, Helicobacter pylori, and Pandora’s box. N Engl J Med. 2002; 347:2162-4. http://www.ncbi.nlm.nih.gov/pubmed/12501230?dopt=AbstractPlus
310. Buller HR, Agnelli G, Hull RD et al. Antithrombotic therapy for venous thromboembolic disease. Chest. 2004; 126(Suppl):401S-28S. http://www.ncbi.nlm.nih.gov/pubmed/15383479?dopt=AbstractPlus
311. Becherucci A, Bagilet D, Marenghini J et al. Effect of topical and oral diclofenac on superficial thrombophlebitis caused by intravenous infusion. Med Clin (Barc). 2000; 114:371-3. http://www.ncbi.nlm.nih.gov/pubmed/10786346?dopt=AbstractPlus
312. McGettigan P, Henry D. Cardiovascular risk and inhibition of cyclooxygenase: a systematic review of observational studies of selective and nonselective inhibitors of cyclooxygenase 2. JAMA. 2006; 296: 1633-44. http://www.ncbi.nlm.nih.gov/pubmed/16968831?dopt=AbstractPlus
313. Kearney PM, Baigent C, Godwin J et al. Do selective cyclo-oxygenase-2 inhibitors and traditional non-steroidal anti-inflammatory drugs increase the risk of atherothrombosis? Meta-analysis of randomised trials. BMJ. 2006; 332: 1302-5. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=1473048&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/16740558?dopt=AbstractPlus
314. Graham DJ. COX-2 inhibitors, other NSAIDs, and cardiovascular risk; the seduction of common sense. JAMA. 2006; 296:1653-6. http://www.ncbi.nlm.nih.gov/pubmed/16968830?dopt=AbstractPlus
315. Merck & Co. Clinoril (sulindac) tablets prescribing information. Whitehouse Station, NJ; 2006 Feb.
316. Chou R, Helfand M, Peterson K et al. Comparative effectiveness and safety of analgesics for osteoarthritis. Comparative effectiveness review no. 4. (Prepared by the Oregon evidence-based practice center under contract no. 290-02-0024.) . Rockville, MD: Agency for Healthcare Research and Quality. 2006 Sep. From AHRQ website. http://www.effectivehealthcare.ahrq.gov/
317. Pfizer. Flector (diclofenac epolamine) topical patch prescribing information. New York, NY; 2018 Aug.
318. Endo Pharmaceuticals. Voltaren (diclofenac sodium 1%) topical gel prescribing information. Malvern, PA; 2018 Sep.
319. Anon. A diclofenac patch (Flector) for pain. Med Lett Drugs Ther. 2008; 50:1-2.
320. Galer BS, Rowbotham M, Perander J et al. Topical diclofenac patch relieves minor sports injury pain: results of a multicenter controlled clinical trial. J Pain Symptom Manage. 2000; 19:287-94. http://www.ncbi.nlm.nih.gov/pubmed/10799795?dopt=AbstractPlus
321. Anon. Diclofenac gel for osteoarthritis. Med Lett Drugs Ther. 2008; 50:31-2.
322. Saag KG, Teng GG, Patkar NM et al. American College of Rheumatology 2008 recommendations for the use of nonbiologic and biologic disease-modifying antirheumatic drugs in rheumatoid arthritis. Arthritis Rheum. 2008; 59:762-84. http://www.ncbi.nlm.nih.gov/pubmed/18512708?dopt=AbstractPlus
323. Endo Pharmaceuticals and Novartis Consumer Health. Dear Healthcare professional. From FDA website. (Accessed 2009 Dec 14.)
324. IBSA Pharma. Licart (diclofenac epolamine) transdermal system prescribing information. Parsippany, NJ; 2020 Sep.
325. GlaxoSmithKline Consumer Health. Voltaren Arthritis Pain (diclofenac sodium) 1% gel drug facts. Warren, NJ; Undated.
326. Apotex. Diclofenac sodium 1.5% topical solution prescribing information. Weston, FL; 2020 Oct.
327. Horizon Medicines. Pennsaid (diclofenac sodium) 2% topical solution prescribing information. Lake Forest, IL; 2020 Mar.
328. Assertio Therapeutics. Cambia (diclofenac potassium) for oral solution prescribing information. Lake Forest, IL; 2019 Sep.
329. Lipton RB, Grosberg B, Singer RP et al. Efficacy and tolerability of a new powdered formulation of diclofenac potassium for oral solution for the acute treatment of migraine: results from the International Migraine Pain Assessment Clinical Trial (IMPACT). Cephalalgia. 2010; 30:1336-45. http://www.ncbi.nlm.nih.gov/pubmed/20959428?dopt=AbstractPlus
330. Kolasinski SL, Neogi T, Hochberg MC et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Rheumatol. 2020; 72:220-233. http://www.ncbi.nlm.nih.gov/pubmed/31908163?dopt=AbstractPlus
331. Depomed. Zipsor (diclofenac potassium) liquid-filled capsules prescribing information. Newark, CA; 2019 May.
332. Lissy M, Scallion R, Stiff DD et al. Pharmacokinetic comparison of an oral diclofenac potassium liquid-filled soft gelatin capsule with a diclofenac potassium tablet. Expert Opin Pharmacother. 2010; 11:701-8. http://www.ncbi.nlm.nih.gov/pubmed/20187842?dopt=AbstractPlus
333. Daniels SE, Baum DR, Clark F et al. Diclofenac potassium liquid-filled soft gelatin capsules for the treatment of postbunionectomy pain. Curr Med Res Opin. 2010; 26:2375-84. http://www.ncbi.nlm.nih.gov/pubmed/20804444?dopt=AbstractPlus
334. Riff DS, Duckor S, Gottlieb I et al. Diclofenac potassium liquid-filled soft gelatin capsules in the management of patients with postbunionectomy pain: a Phase III, multicenter, randomized, double-blind, placebo-controlled study conducted over 5 days. Clin Ther. 2009; 31:2072-85. http://www.ncbi.nlm.nih.gov/pubmed/19922878?dopt=AbstractPlus
335. de Abajo FJ, Montero D, Madurga M et al. Acute and clinically relevant drug-induced liver injury: a population based case-control study. Br J Clin Pharmacol. 2004; 58:71-80. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=PMC1884531&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/15206996?dopt=AbstractPlus
500. Food and Drug Administration. Drug safety communication: FDA strengthens warning that non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) can cause heart attacks or strokes. Silver Spring, MD; 2015 Jul 9. From the FDA web site. Accessed 2016 Mar 22. http://www.fda.gov/Drugs/DrugSafety/ucm451800.htm
501. Coxib and traditional NSAID Trialists' (CNT) Collaboration, Bhala N, Emberson J et al. Vascular and upper gastrointestinal effects of non-steroidal anti-inflammatory drugs: meta-analyses of individual participant data from randomised trials. Lancet. 2013; 382:769-79. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=3778977&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/23726390?dopt=AbstractPlus
502. Food and Drug Administration. FDA briefing document: Joint meeting of the arthritis advisory committee and the drug safety and risk management advisory committee, February 10-11, 2014. From FDA web site http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/ArthritisAdvisoryCommittee/UCM383180.pdf
503. Trelle S, Reichenbach S, Wandel S et al. Cardiovascular safety of non-steroidal anti-inflammatory drugs: network meta-analysis. BMJ. 2011; 342:c7086. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=3019238&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/21224324?dopt=AbstractPlus
504. Gislason GH, Rasmussen JN, Abildstrom SZ et al. Increased mortality and cardiovascular morbidity associated with use of nonsteroidal anti-inflammatory drugs in chronic heart failure. Arch Intern Med. 2009; 169:141-9. http://www.ncbi.nlm.nih.gov/pubmed/19171810?dopt=AbstractPlus
505. Schjerning Olsen AM, Fosbøl EL, Lindhardsen J et al. Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: a nationwide cohort study. Circulation. 2011; 123:2226-35. http://www.ncbi.nlm.nih.gov/pubmed/21555710?dopt=AbstractPlus
506. McGettigan P, Henry D. Cardiovascular risk with non-steroidal anti-inflammatory drugs: systematic review of population-based controlled observational studies. PLoS Med. 2011; 8:e1001098. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=3181230&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/21980265?dopt=AbstractPlus
507. Yancy CW, Jessup M, Bozkurt B et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013; 62:e147-239. http://www.ncbi.nlm.nih.gov/pubmed/23747642?dopt=AbstractPlus
508. Novartis Pharmaceuticals Corporation. Voltaren-XR (diclofenac sodium extended-release tablets) prescribing information. East Hanover, NJ; 2016 May.
511. Olsen AM, Fosbøl EL, Lindhardsen J et al. Long-term cardiovascular risk of nonsteroidal anti-inflammatory drug use according to time passed after first-time myocardial infarction: a nationwide cohort study. Circulation. 2012; 126:1955-63. http://www.ncbi.nlm.nih.gov/pubmed/22965337?dopt=AbstractPlus
512. Olsen AM, Fosbøl EL, Lindhardsen J et al. Cause-specific cardiovascular risk associated with nonsteroidal anti-inflammatory drugs among myocardial infarction patients--a nationwide study. PLoS One. 2013; 8:e54309.
516. Bavry AA, Khaliq A, Gong Y et al. Harmful effects of NSAIDs among patients with hypertension and coronary artery disease. Am J Med. 2011; 124:614-20. http://www.pubmedcentral.nih.gov/picrender.fcgi?tool=pmcentrez&artid=4664475&blobtype=pdf http://www.ncbi.nlm.nih.gov/pubmed/21596367?dopt=AbstractPlus
520. Health Canada. Summary safety review: Diclofenac - risk of major heart and stroke related adverse events. Ottawa, ON, Canada; 2014 Oct 14. From Health Canada website. http://www.hc-sc.gc.ca/dhp-mps/medeff/reviews-examens/diclofenac-eng.php
521. European Medicines Agency. New safety advice for diclofenac: new measures aim to minimise cardiovascular risks. London, UK; 2013 Sep 25. From European Medicines Agency website. http://www.ema.europa.eu/docs/en_GB/document_library/Referrals_document/Diclofenac-containing_medicinal_products/European_Commission_final_decision/WC500155819.pdf
1200. US Food and Drug Administration. FDA drug safety communication: FDA recommends avoiding use of NSAIDs in pregnancy at 20 weeks or later because they can result in low amniotic fluid. 2020 Oct 15. From the FDA website. https://www.fda.gov/drugs/drug-safety-and-availability/fda-recommends-avoiding-use-nsaids-pregnancy-20-weeks-or-later-because-they-can-result-low-amniotic
1202. Actavis Pharma. Sulindac tablets prescribing information. Parsippany, NJ; 2020 Oct 20.
Frequently asked questions
- Can I take ibuprofen with blood pressure medications?
- Which painkiller should you use?
- Why is diclofenac prescription only but ibuprofen is OTC?
- Can NSAIDs be used to treat a COVID-19 fever?
- Does the drug diclofenac have narcotics in it?
More about diclofenac
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (685)
- Drug images
- Latest FDA alerts (11)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: Nonsteroidal anti-inflammatory drugs
- Breastfeeding
- En español
Patient resources
Professional resources
- Diclofenac prescribing information
- Diclofenac Capsule (FDA)
- Diclofenac Delayed Release Tablets (FDA)
- Diclofenac Extended Release Tablets 100mg (FDA)
- Diclofenac Oral Solution (FDA)
Other brands
Voltaren, Cataflam, Cambia, Voltaren-XR, ... +3 more